Abstract
Crit Care Sci. 2023;35(1):19-30
DOI 10.5935/2965-2774.20230203-pt
To evaluate the factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19.
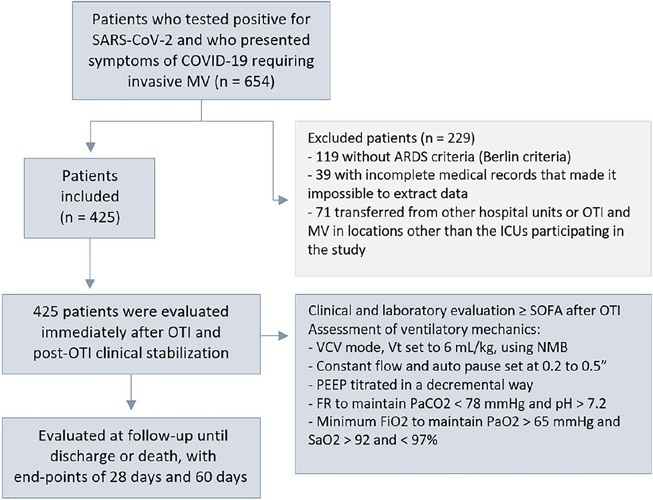
This was a retrospective, multicenter cohort study that included 425 mechanically ventilated adult patients with COVID-19 admitted to 4 intensive care units. Clinical data comprising the SOFA score, laboratory data and mechanical characteristics of the respiratory system were collected in a standardized way immediately after the start of invasive mechanical ventilation. The risk factors for death were analyzed using Cox regression to estimate the risk ratios and their respective 95%CIs.
Body mass index (RR 1.17; 95%CI 1.11 - 1.20; p < 0.001), SOFA score (RR 1.39; 95%CI 1.31 - 1.49; p < 0.001) and driving pressure (RR 1.24; 95%CI 1.21 - 1.29; p < 0.001) were considered independent factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19. Respiratory system compliance (RR 0.92; 95%CI 0.90 - 0.93; p < 0.001) was associated with lower mortality. The comparative analysis of the survival curves indicated that patients with respiratory system compliance (< 30mL/cmH2O), a higher SOFA score (> 5 points) and higher driving pressure (> 14cmH2O) were more significantly associated with the outcome of death at 28 days and 60 days.
Patients with a body mass index > 32kg/m2, respiratory system compliance < 30mL/cmH2O, driving pressure > 14cmH2O and SOFA score > 5.8 immediately after the initiation of invasive ventilatory support had worse outcomes, and independent risk factors were associated with higher mortality in this population.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):335-341
DOI 10.5935/0103-507X.20220040-en
To compare the lung mechanics and outcomes between COVID-19-associated acute respiratory distress syndrome and non-COVID-19-associated acute respiratory distress syndrome.
We combined data from two randomized trials in acute respiratory distress syndrome, one including only COVID-19 patients and the other including only patients without COVID-19, to determine whether COVID-19-associated acute respiratory distress syndrome is associated with higher 28-day mortality than non-COVID-19 acute respiratory distress syndrome and to examine the differences in lung mechanics between these two types of acute respiratory distress syndrome.
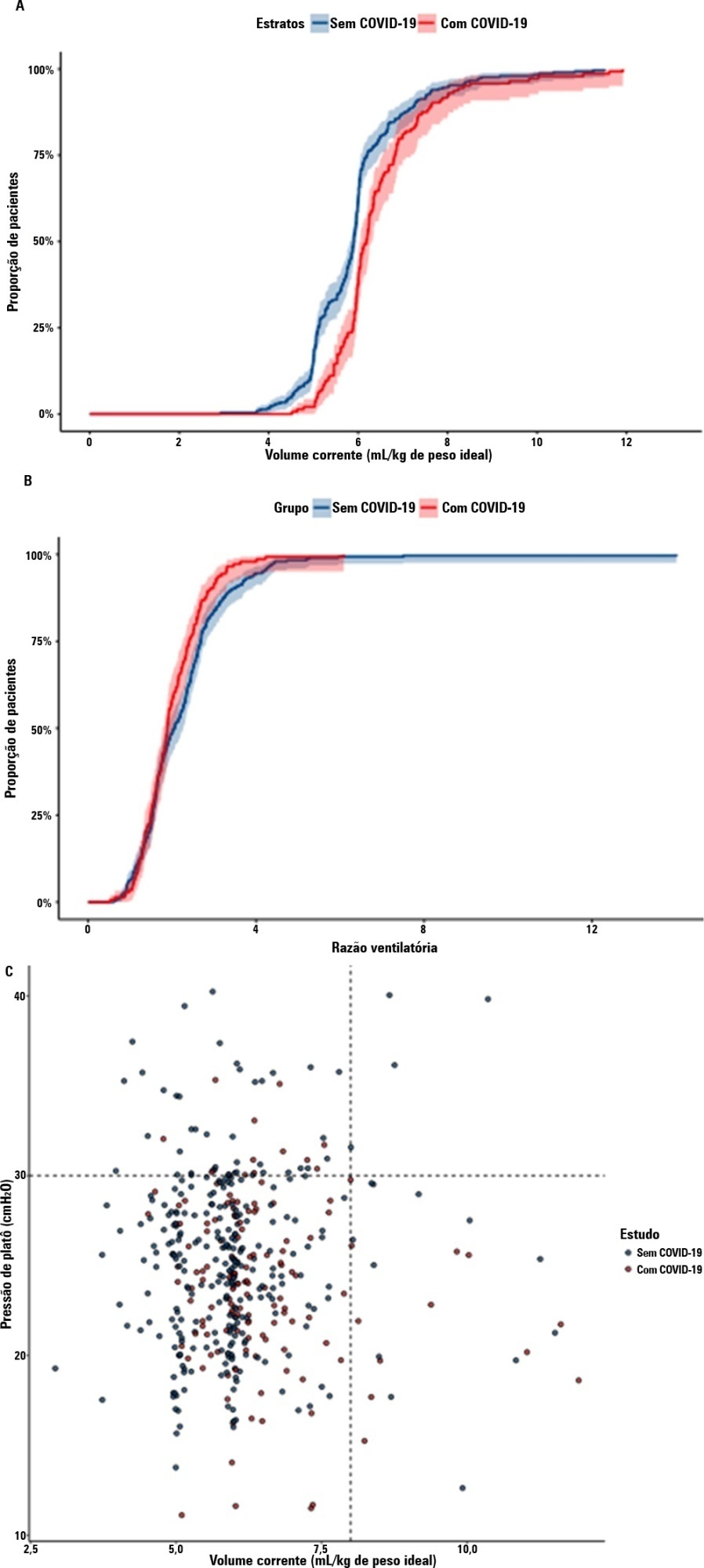
A total of 299 patients with COVID-19-associated acute respiratory distress syndrome and 1,010 patients with non-COVID-19-associated acute respiratory distress syndrome were included in the main analysis. The results showed that non-COVID-19 patients used higher positive end-expiratory pressure (12.5cmH2O; SD 3.2 versus 11.7cmH2O SD 2.8; p < 0.001), were ventilated with lower tidal volumes (5.8mL/kg; SD 1.0 versus 6.5mL/kg; SD 1.2; p < 0.001) and had lower static respiratory compliance adjusted for ideal body weight (0.5mL/cmH2O/kg; SD 0.3 versus 0.6mL/cmH2O/kg; SD 0.3; p = 0.01). There was no difference between groups in 28-day mortality (52.3% versus 58.9%; p = 0.52) or mechanical ventilation duration in the first 28 days among survivors (13 [IQR 5 - 22] versus 12 [IQR 6 - 26], p = 0.46).
This analysis showed that patients with non-COVID-19-associated acute respiratory distress syndrome have different lung mechanics but similar outcomes to COVID-19-associated acute respiratory distress syndrome patients. After propensity score matching, there was no difference in lung mechanics or outcomes between groups.
Abstract
Rev Bras Ter Intensiva. 2022;34(2):212-219
DOI 10.5935/0103-507X.20220018-en
To analyze the influence of mechanical power and its components on mechanical ventilation for patients infected with SARS-CoV-2; identify the values of the mechanical ventilation components and verify their correlations with each other and with the mechanical power and effects on the result of the Gattinoni-S and Giosa formulas.
This was an observational, longitudinal, analytical and quantitative study of respirator and mechanical power parameters in patients with SARS-CoV-2.
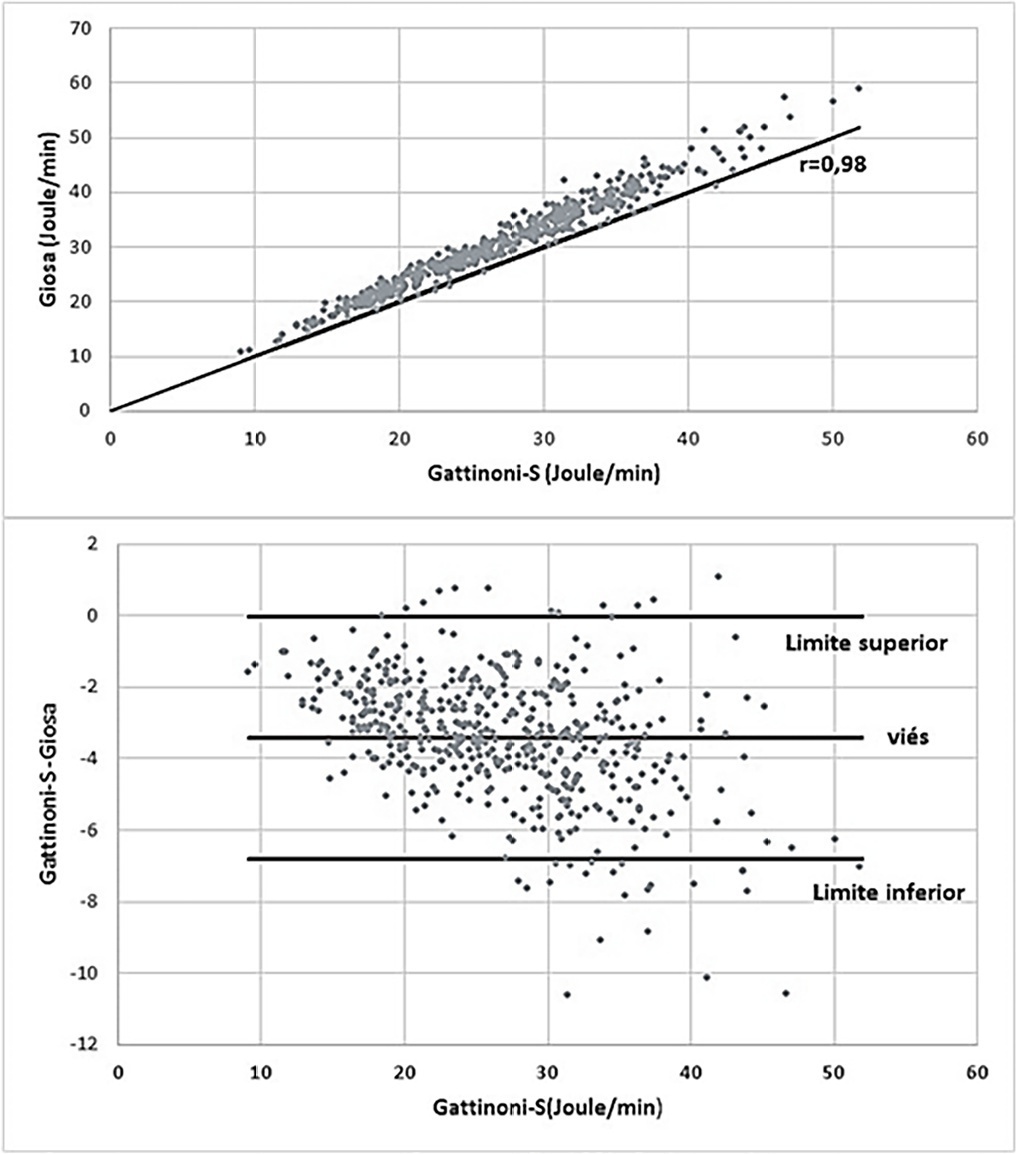
The mean mechanical power was 26.9J/minute (Gattinoni-S) and 30.3 J/minute (Giosa). The driving pressure was 14.4cmH2O, the plateau pressure was 26.5cmH2O, the positive end-expiratory pressure was 12.1cmH2O, the elastance was 40.6cmH2O/L, the tidal volume was 0.36L, and the respiratory rate was 32 breaths/minute. The correlation between the Gattinoni and Giosa formulas was 0.98, with a bias of -3.4J/minute and a difference in the correlation of the resistance pressure of 0.39 (Gattinoni) and 0.24 (Giosa). Among the components, the correlations between elastance and driving pressure (0.88), positive end-expiratory pressure (-0.54) and tidal volume (-0.44) stood out.
In the analysis of mechanical ventilation for patients with SARS-CoV-2, it was found that the correlations of its components with mechanical power influenced its high momentary values and and that the correlations of its components with each other influenced their behavior throughout the study period. Because they have specific effects on the Gatinnoni-S and Giosa formulas, the mechanical ventilation components influenced their calculations and caused divergence in the mechanical power values.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):537-543
DOI 10.5935/0103-507X.20210081
To compare gas exchange indices behavior by using liberal versus conservative oxygenation targets in patients with moderate to severe acute respiratory distress syndrome secondary to COVID-19 under invasive mechanical ventilation. We also assessed the influence of high FiO2 on respiratory system mechanics.
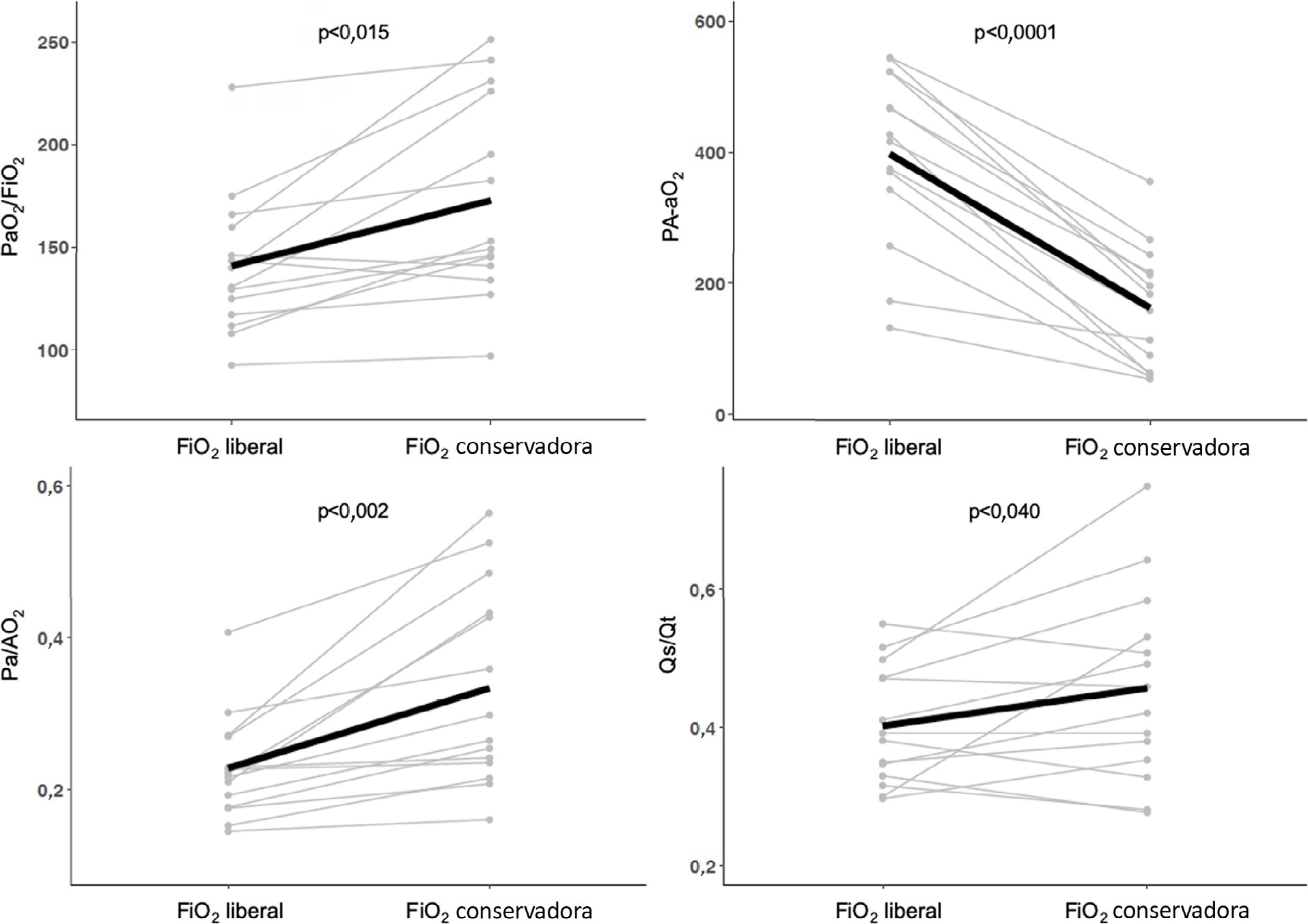
We prospectively included consecutive patients aged over 18 years old with a diagnosis of COVID-19 and moderate-severe acute respiratory distress syndrome. For each patient, we randomly applied two FiO2 protocols to achieve SpO2 88% - 92% or 96%. We assessed oxygenation indices and respiratory system mechanics.
We enrolled 15 patients. All the oxygenation indices were significantly affected by the FiO2 strategy (p < 0.05) selected. The PaO2/FiO2 deteriorated, PA-aO2 increased and Pa/AO2 decreased significantly when using FiO2 to achieve SpO2 96%. Conversely, the functional shunt fraction was reduced. Respiratory mechanics were not affected by the FiO2 strategy.
A strategy aimed at liberal oxygenation targets significantly deteriorated gas exchange indices, except for functional shunt, in COVID-19-related acute respiratory distress syndrome. The respiratory system mechanics were not altered by the FiO2 strategy.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):616-623
DOI 10.5935/0103-507X.20210071
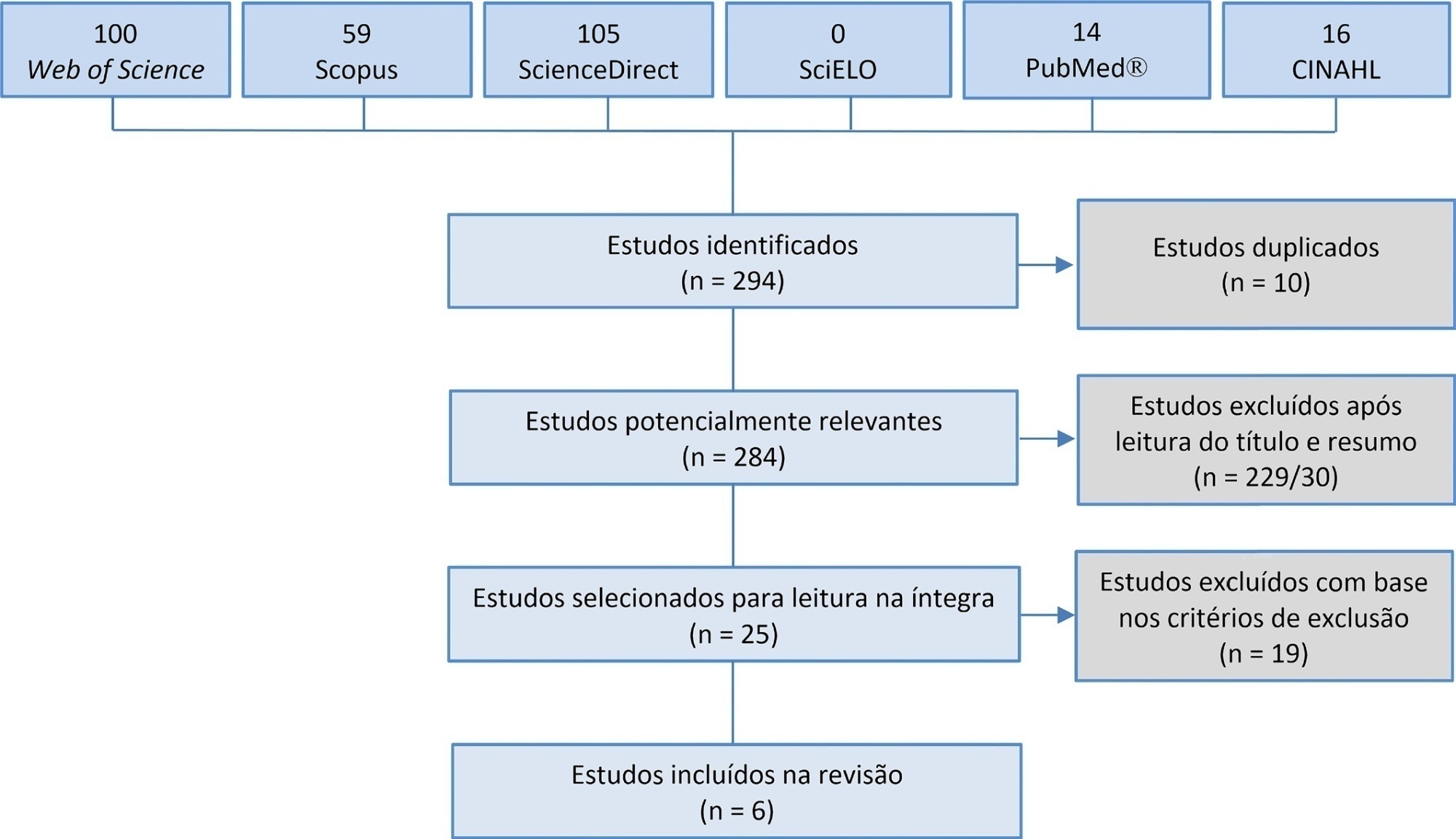
Manual hyperinflation is used in neonatal and pediatric intensive care units to promote expiratory flow bias, but there is no consensus on the benefits of the technique. Thus, a review that presents supporting evidence is necessary. This study aims to review the literature on the manual hyperinflation maneuver in neonatal and pediatric intensive care units to analyze the evidence for this technique in terms of the forms of application (associated with other techniques or not), its safety, the performance of manual resuscitators and the influence of the physical therapist’s experience, in addition to evaluating the methodological quality of the identified articles. A search was performed in the following databases: Web of Science, ScienceDirect, PubMedⓇ, Scopus, CINAHL and SciELO. Two researchers independently selected the articles. Duplicate studies were assessed, evaluated by title and abstract and then read in full. The quality of the articles was analyzed using the PEDro scale. Six articles were included, two of which had high methodological quality. The main results provided information on the contribution of the positive end-expiratory pressure valve to increasing lung volumes and the use of chest compressions to optimize expiratory flow bias, the negative influence of operator experience on the increase in peak inspiratory flow, the performance of different manual resuscitators when used with the technique and the safety of application in terms of maintaining hemodynamic stability and increasing peripheral oxygen saturation. The available studies point to a positive effect of the manual hyperinflation maneuver in children who are admitted to intensive care units.
Registration PROSPERO: CRD42018108056.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):261-265
DOI 10.5935/0103-507X.20210033
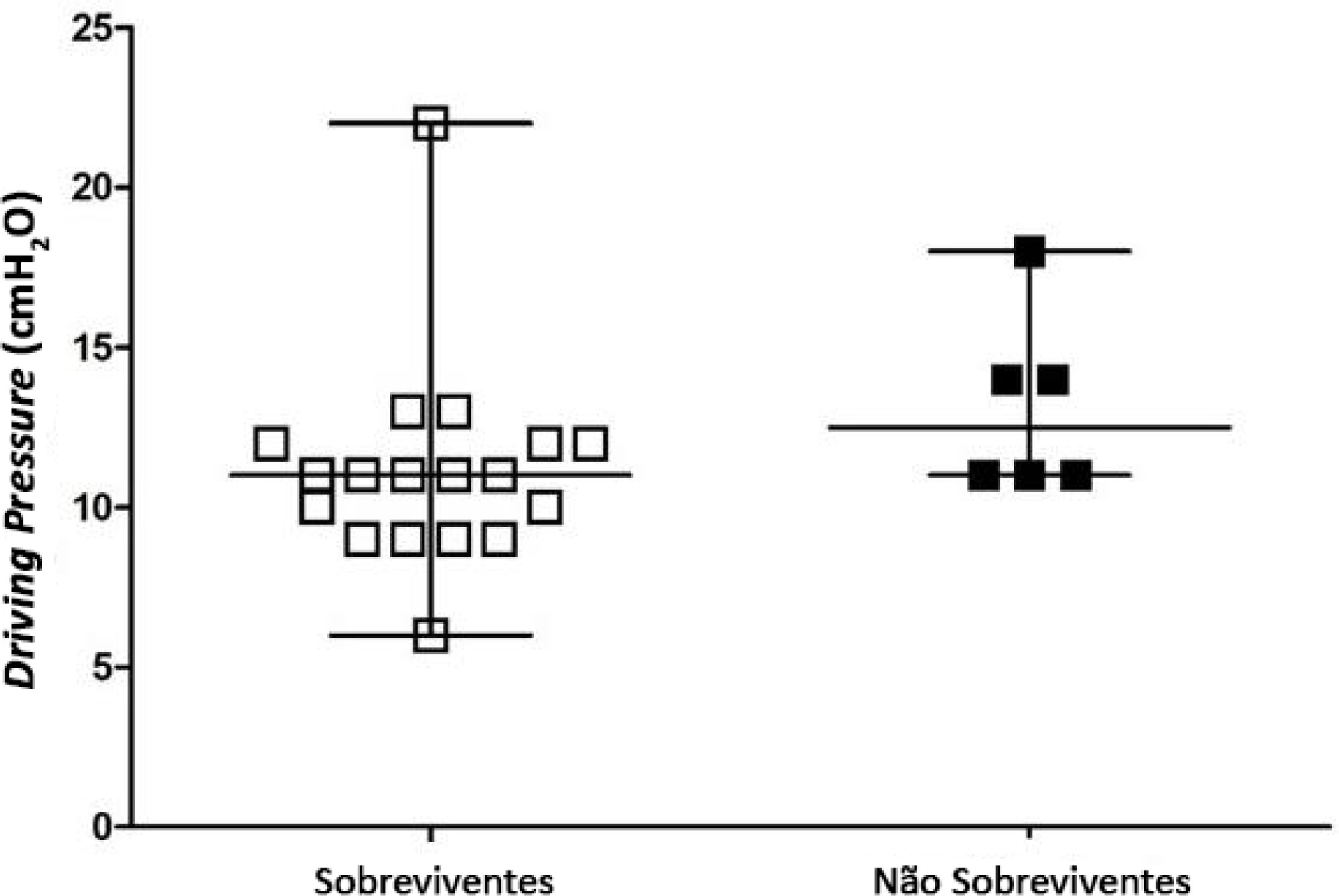
To identify the possible association between driving pressure and mechanical power values and oxygenation index on the first day of mechanical ventilation with the mortality of trauma patients without a diagnosis of acute respiratory distress syndrome.
Patients under pressure-controlled or volume-controlled ventilation were included, with data collection 24 hours after orotracheal intubation. Patient follow-up was performed for 30 days to obtain the clinical outcome. The patients were admitted to two intensive care units of the Hospital de Pronto Socorro de Porto Alegre from June to September 2019.
A total of 24 patients were evaluated. Driving pressure, mechanical power and oxygenation index were similar among patients who survived and those who died, with no statistically significant difference between groups.
Driving pressure, mechanical power and oxygenation index values obtained on the first day of mechanical ventilation were not associated with mortality of trauma patients without acute respiratory distress syndrome.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):398-404
DOI 10.5935/0103-507X.20200068
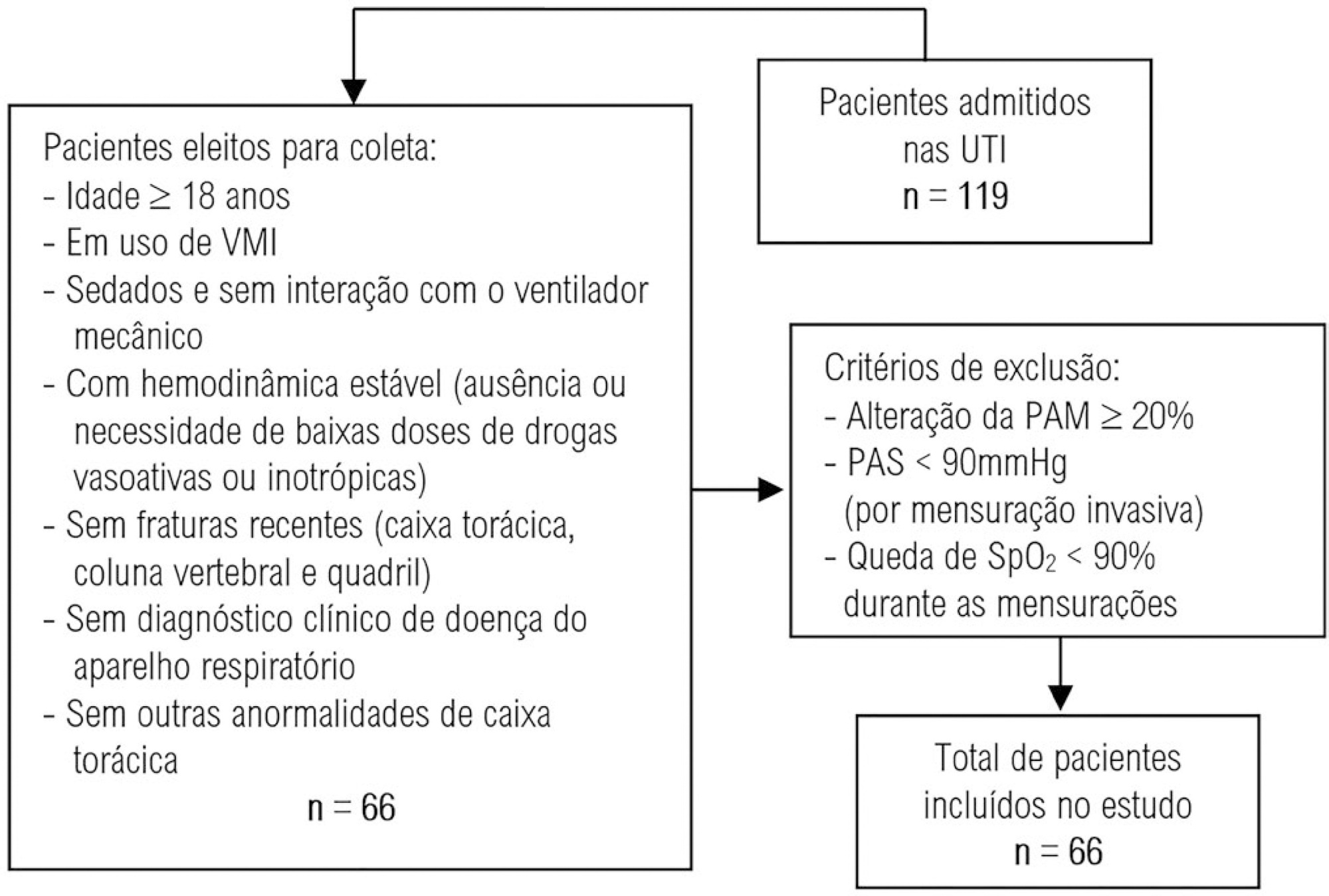
To evaluate the intra- and interexaminer reproducibility of measurements of the resistance and static and dynamic compliance of the respiratory system in patients on mechanical ventilation.
This was an analytical study conducted with individuals aged ≥ 18 years who were on invasive mechanical ventilation and had no clinical diagnosis of respiratory system disease and/or chest abnormality. Three measurements of respiratory mechanics were performed with a 1-minute interval between them. The first and third measurements were performed by examiner A, the second by examiner B. The values for the resistance and static and dynamic compliance of the respiratory system were compared using the intraclass correlation coefficient.
A total of 198 measurements of respiratory mechanics were performed for 66 patients on mechanical ventilation. The patients had a mean age of 52.6 ± 18.6 years and a mean body mass index of 21.6 ± 2.1kg/m2; a surgical profile (61.5%) and female sex (53.8%) were predominant. Mean values were obtained for the three measurements of respiratory system resistance (A1: 15.7 ± 6.8cmH2O/L/s; B1: 15.7 ± 6.4cmH2O/L/s and A2: 15.9 ± 6.2cmH2O/L/s), respiratory system static compliance (A1: 42.1 ± 13.7mL/cmH2O; B1: 42.4 ± 14.6mL/cmH2O and A2: 42.2 ± 14.5mL/cmH2O) and respiratory system dynamic compliance (A1: 21.3 ± 7.3mL/cmH2O; B1: 21.4 ± 7.5mL/cmH2O and A2: 21.3 ± 6.2mL/cmH2O). The intraclass correlation coefficient was also calculated for respiratory system resistance (R = 0.882 and p = 0.001; R = 0.949 and p = 0.001 - interexaminer A1 versus B and B versus A2, respectively; R = 0.932 and p = 0.001 - intraexaminer); respiratory system static compliance (R = 0.951 and p = 0.001; R = 0.958 and p = 0.001 - interexaminer A1 versus B and B versus A2, respectively; R = 0.965 and p = 0.001 - intraexaminer) and respiratory system dynamic compliance (R = 0.957 and p = 0.001; R = 0.946 and p = 0.001 - interexaminer A1 versus B and B versus A2, respectively; R = 0.926 and p = 0.001 - intraexaminer).
The measurements of resistance and static and dynamic compliance of the respiratory system show good intra- and interexaminer reproducibility for ventilated patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):289-295
DOI 10.5935/0103-507X.20190052
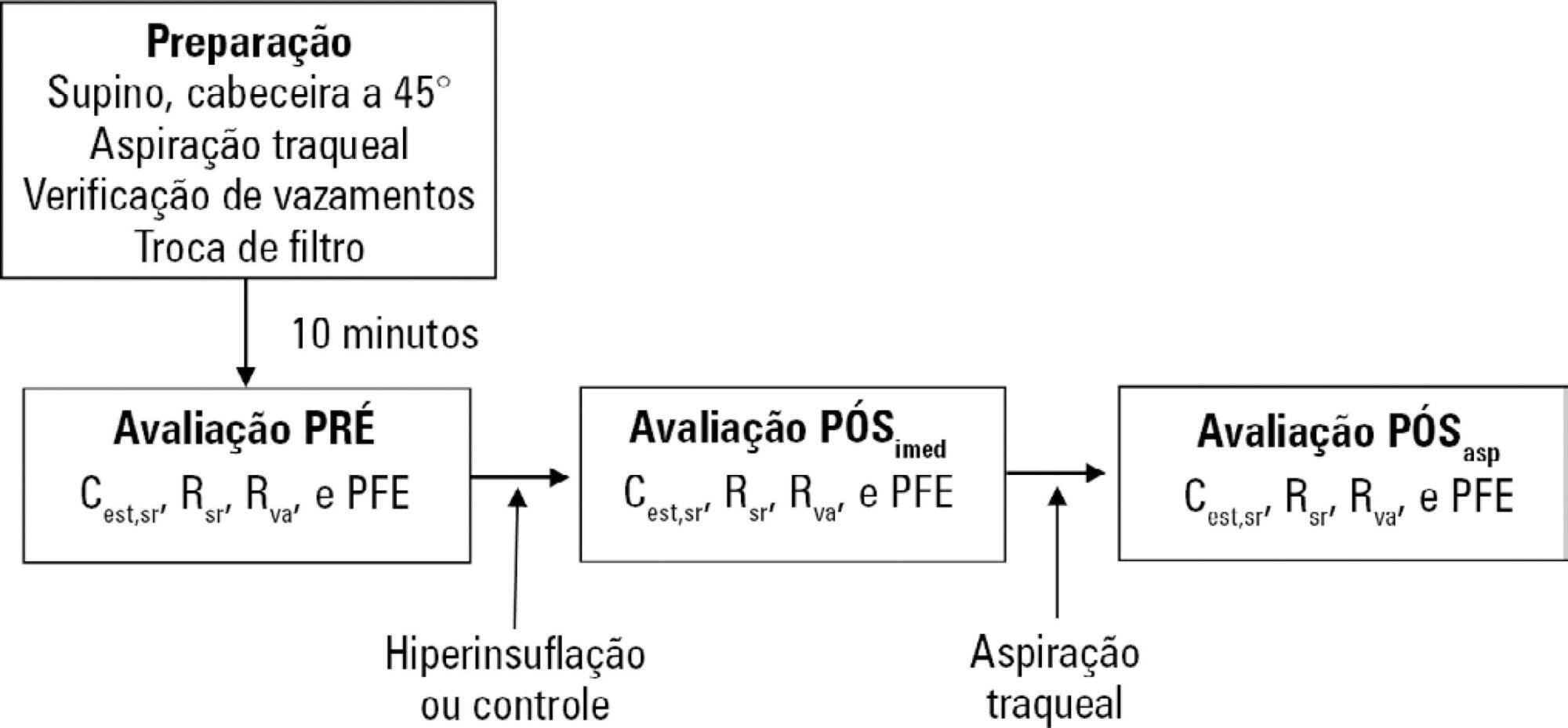
To evaluate the effects of ventilator hyperinflation on respiratory mechanics.
A randomized crossover clinical trial was conducted with 38 mechanically ventilated patients with pulmonary infection. The order of the hyperinflation and control (without changes in the parameters) conditions was randomized. Hyperinflation was performed for 5 minutes in pressure-controlled ventilation mode, with progressive increases of 5cmH2O until a maximum pressure of 35cmH2O was reached, maintaining positive end expiratory pressure. After 35cmH2O was reached, the inspiratory time and respiratory rate were adjusted so that the inspiratory and expiratory flows reached baseline levels. Measurements of static compliance, total resistance and airway resistance, and peak expiratory flow were evaluated before the technique, immediately after the technique and after aspiration. Two-way analysis of variance for repeated measures was used with Tukey's post hoc test, and p < 0.05 was considered significant.
Ventilator hyperinflation increased static compliance, which remained at the same level after aspiration (46.2 ± 14.8 versus 52.0 ± 14.9 versus 52.3 ± 16.0mL/cmH2O; p < 0.001). There was a transient increase in airway resistance (6.6 ± 3.6 versus 8.0 ± 5.5 versus 6.6 ± 3.5cmH2O/Ls-1; p < 0.001) and a transient reduction in peak expiratory flow (32.0 ± 16.0 versus 29.8 ± 14.8 versus 32.1 ± 15.3Lpm; p <0.05) immediately after the technique; these values returned to pretechnique levels after tracheal aspiration. There were no changes in the control condition, nor were hemodynamic alterations observed.
Ventilator hyperinflation promoted increased compliance associated with a transient increase in airway resistance and peak expiratory flow, with reduction after aspiration.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)