You searched for:"Helena França Correia"
We found (3) results for your search.-
Original Article
Reproducibility of respiratory mechanics measurements in patients on invasive mechanical ventilation
Rev Bras Ter Intensiva. 2020;32(3):398-404
Abstract
Original ArticleReproducibility of respiratory mechanics measurements in patients on invasive mechanical ventilation
Rev Bras Ter Intensiva. 2020;32(3):398-404
DOI 10.5935/0103-507X.20200068
Views0See moreABSTRACT
Objective:
To evaluate the intra- and interexaminer reproducibility of measurements of the resistance and static and dynamic compliance of the respiratory system in patients on mechanical ventilation.
Methods:
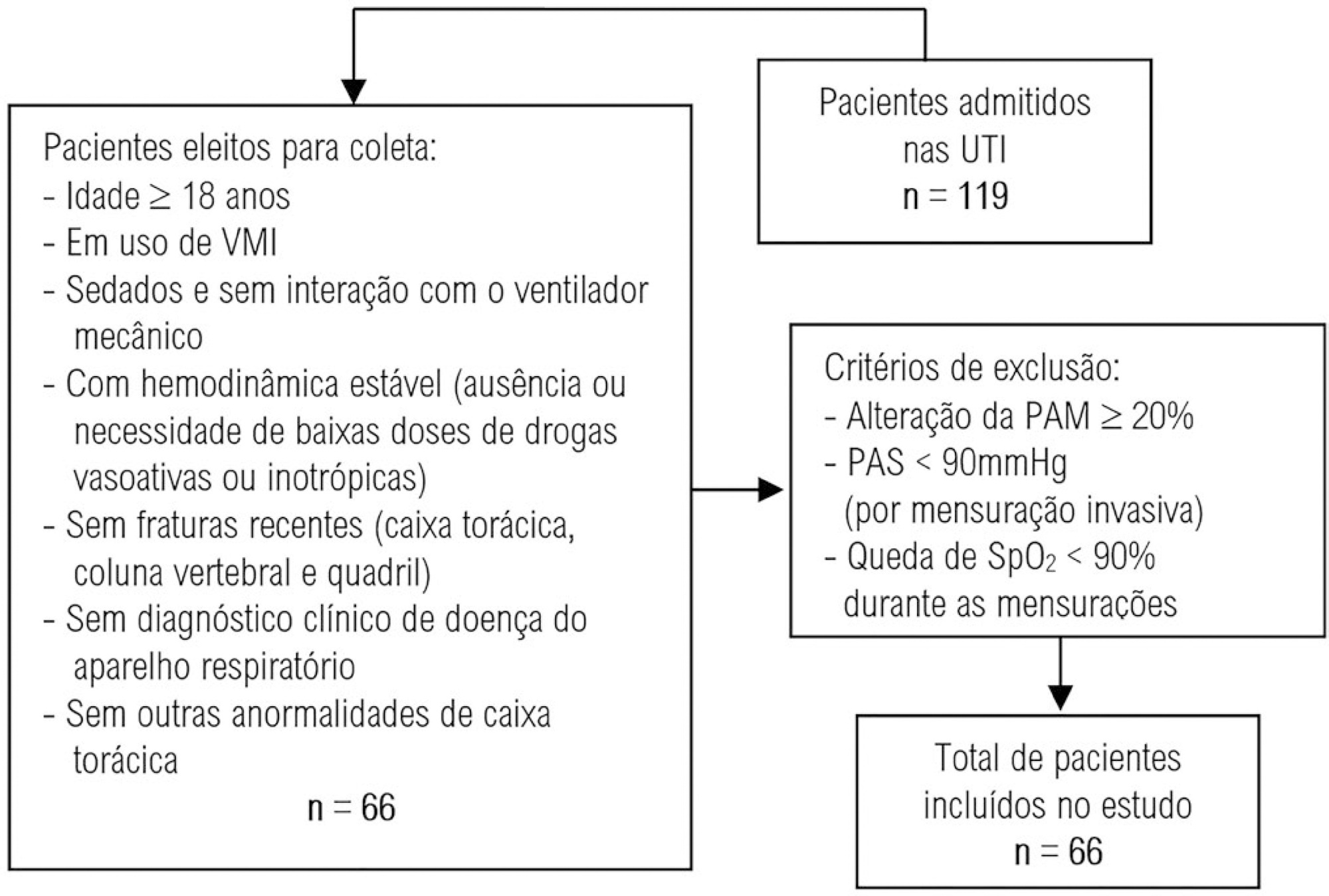
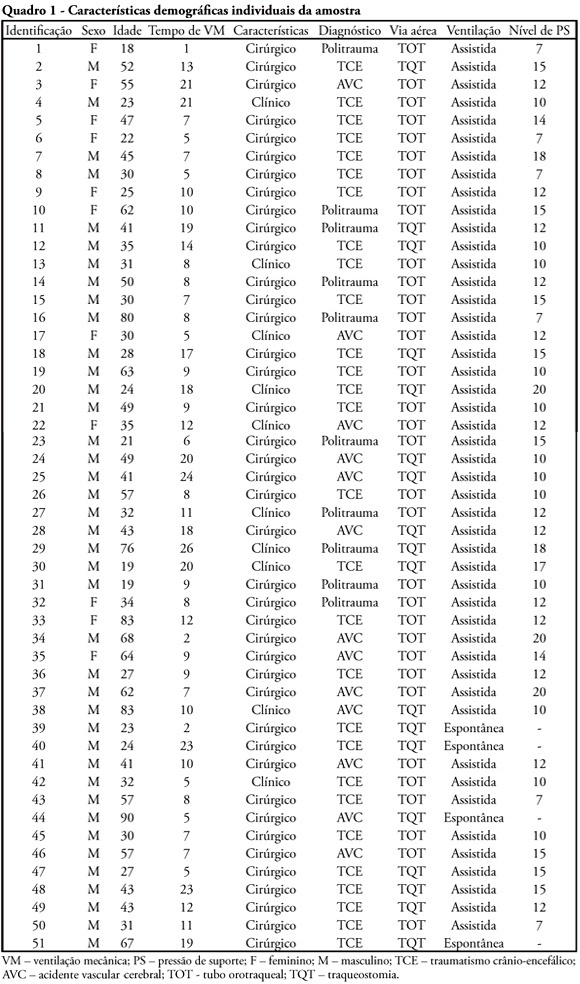
This was an analytical study conducted with individuals aged ≥ 18 years who were on invasive mechanical ventilation and had no clinical diagnosis of respiratory system disease and/or chest abnormality. Three measurements of respiratory mechanics were performed with a 1-minute interval between them. The first and third measurements were performed by examiner A, the second by examiner B. The values for the resistance and static and dynamic compliance of the respiratory system were compared using the intraclass correlation coefficient.
Results:
A total of 198 measurements of respiratory mechanics were performed for 66 patients on mechanical ventilation. The patients had a mean age of 52.6 ± 18.6 years and a mean body mass index of 21.6 ± 2.1kg/m2; a surgical profile (61.5%) and female sex (53.8%) were predominant. Mean values were obtained for the three measurements of respiratory system resistance (A1: 15.7 ± 6.8cmH2O/L/s; B1: 15.7 ± 6.4cmH2O/L/s and A2: 15.9 ± 6.2cmH2O/L/s), respiratory system static compliance (A1: 42.1 ± 13.7mL/cmH2O; B1: 42.4 ± 14.6mL/cmH2O and A2: 42.2 ± 14.5mL/cmH2O) and respiratory system dynamic compliance (A1: 21.3 ± 7.3mL/cmH2O; B1: 21.4 ± 7.5mL/cmH2O and A2: 21.3 ± 6.2mL/cmH2O). The intraclass correlation coefficient was also calculated for respiratory system resistance (R = 0.882 and p = 0.001; R = 0.949 and p = 0.001 – interexaminer A1 versus B and B versus A2, respectively; R = 0.932 and p = 0.001 – intraexaminer); respiratory system static compliance (R = 0.951 and p = 0.001; R = 0.958 and p = 0.001 – interexaminer A1 versus B and B versus A2, respectively; R = 0.965 and p = 0.001 – intraexaminer) and respiratory system dynamic compliance (R = 0.957 and p = 0.001; R = 0.946 and p = 0.001 – interexaminer A1 versus B and B versus A2, respectively; R = 0.926 and p = 0.001 – intraexaminer).
Conclusion:
The measurements of resistance and static and dynamic compliance of the respiratory system show good intra- and interexaminer reproducibility for ventilated patients.
-
Original Articles
Association between the rapid shallow breathing index and extubation success in patients with traumatic brain injury
Rev Bras Ter Intensiva. 2013;25(3):212-217
Abstract
Original ArticlesAssociation between the rapid shallow breathing index and extubation success in patients with traumatic brain injury
Rev Bras Ter Intensiva. 2013;25(3):212-217
DOI 10.5935/0103-507X.20130037
Views0See moreOBJECTIVE:
To investigate the association between the rapid shallow breathing index and successful extubation in patients with traumatic brain injury.
METHODS:
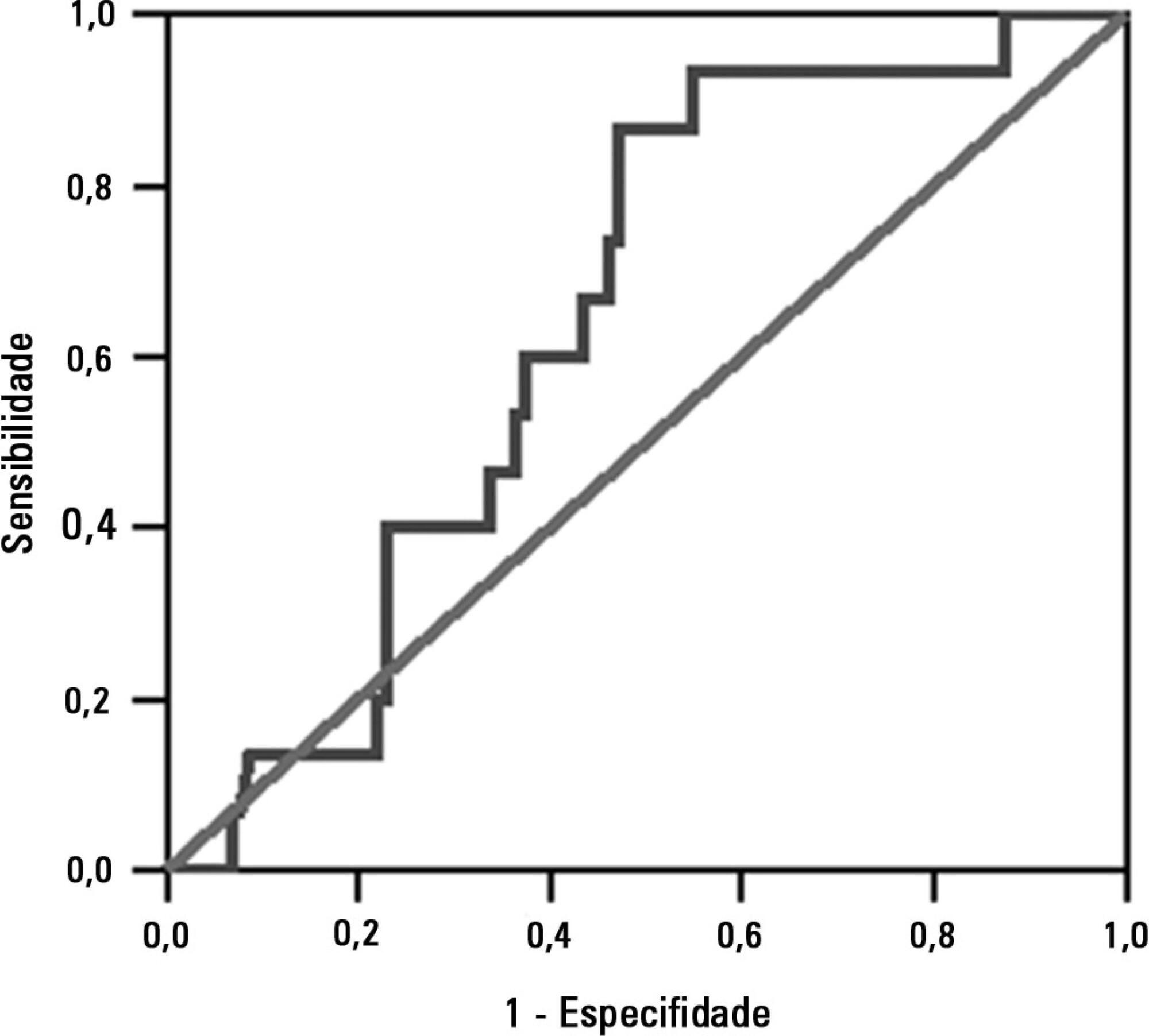
This study was a prospective study conducted in patients with traumatic brain injury of both genders who underwent mechanical ventilation for at least two days and who passed a spontaneous breathing trial. The minute volume and respiratory rate were measured using a ventilometer, and the data were used to calculate the rapid shallow breathing index (respiratory rate/tidal volume). The dependent variable was the extubation outcome: reintubation after up to 48 hours (extubation failure) or not (extubation success). The independent variable was the rapid shallow breathing index measured after a successful spontaneous breathing trial.
RESULTS:
The sample comprised 119 individuals, including 111 (93.3%) males. The average age of the sample was 35.0±12.9 years old. The average duration of mechanical ventilation was 8.1±3.6 days. A total of 104 (87.4%) participants achieved successful extubation. No association was found between the rapid shallow breathing index and extubation success.
CONCLUSION:
The rapid shallow breathing index was not associated with successful extubation in patients with traumatic brain injury.
-
Original Articles
Comparison and effects of two different airway occlusion times during measurement of maximal inspiratory pressure in adult intensive care unit neurological patients
Rev Bras Ter Intensiva. 2010;22(1):33-39
Abstract
Original ArticlesComparison and effects of two different airway occlusion times during measurement of maximal inspiratory pressure in adult intensive care unit neurological patients
Rev Bras Ter Intensiva. 2010;22(1):33-39
DOI 10.1590/S0103-507X2010000100007
Views0See moreOBJECTIVE: To verify if the maximal inspiratory pressure values with 40 seconds occlusion time are greater than with the 20 seconds occlusion time, and the impacts on the following patient’s physiological variables: respiratory rate, pulse oxygen saturation, heart rate and blood pressure, before and after the measurements. METHODS: This was a transversal prospective randomized study. Fifty-one patients underwent maximal inspiratory pressure measurement, measured by one single investigator. The manometer was calibrated before each measurement, and then connected to the adapter and this to the unidirectional valve inspiratory branch for 20 or 40 seconds. RESULTS: The values with 40 seconds occlusion (57.6 ± 23.4 cmH2O) were significantly higher than the measurements taken with 20 seconds occlusion (40.5 ± 23.4 cmH2O; p=0.0001). The variables changes between the before and after measurement respiratory and hemodynamic parameters monitoring showed: heart rate variation for the 20 seconds occlusion 5.13 ± 8.56 beats per minute and after 40 seconds occlusion 7.94 ± 12.05 beats per minute (p = 0.053), versus baseline. The mean blood pressure change for 20 seconds occlusion was 9.29 ± 13.35 mmHg and for 40 seconds occlusion 15.52 ± 2.91 mmHg (p=0.021). The oxygen saturation change for 20 seconds occlusion was 1.66 ± 12.66%, and for 40 seconds 4.21 ± 5.53% (p=0.0001). The respiratory rate change for 20 seconds occlusion was 6.68 ± 12.66 movements per minute and for 40 seconds 6.94 ± 6.01 (p=0.883). CONCLUSION: The measurement of maximal inspiratory pressure using a longer occlusion (40 seconds) produced higher values, without triggering clinically significant stress according to the selected variables.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




