You searched for:"Arthur de Sá Ferreira"
We found (2) results for your search.-
Original Article
Factors associated with mortality in mechanically ventilated patients with severe acute respiratory syndrome due to COVID-19 evolution
Crit Care Sci. 2023;35(1):19-30
Abstract
Original ArticleFactors associated with mortality in mechanically ventilated patients with severe acute respiratory syndrome due to COVID-19 evolution
Crit Care Sci. 2023;35(1):19-30
DOI 10.5935/2965-2774.20230203-pt
Views16ABSTRACT
Objectives:
To evaluate the factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19.
Methods:
This was a retrospective, multicenter cohort study that included 425 mechanically ventilated adult patients with COVID-19 admitted to 4 intensive care units. Clinical data comprising the SOFA score, laboratory data and mechanical characteristics of the respiratory system were collected in a standardized way immediately after the start of invasive mechanical ventilation. The risk factors for death were analyzed using Cox regression to estimate the risk ratios and their respective 95%CIs.
Results:
Body mass index (RR 1.17; 95%CI 1.11 – 1.20; p < 0.001), SOFA score (RR 1.39; 95%CI 1.31 - 1.49; p < 0.001) and driving pressure (RR 1.24; 95%CI 1.21 - 1.29; p < 0.001) were considered independent factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19. Respiratory system compliance (RR 0.92; 95%CI 0.90 - 0.93; p < 0.001) was associated with lower mortality. The comparative analysis of the survival curves indicated that patients with respiratory system compliance (< 30mL/cmH2O), a higher SOFA score (> 5 points) and higher driving pressure (> 14cmH2O) were more significantly associated with the outcome of death at 28 days and 60 days.
Conclusion:
Patients with a body mass index > 32kg/m2, respiratory system compliance < 30mL/cmH2O, driving pressure > 14cmH2O and SOFA score > 5.8 immediately after the initiation of invasive ventilatory support had worse outcomes, and independent risk factors were associated with higher mortality in this population.
Keywords:artificialCoronavirus infectionsCOVID-19MortalityRespirationRespiratory distress syndromeRespiratory mechanicsSARS-CoV-2See more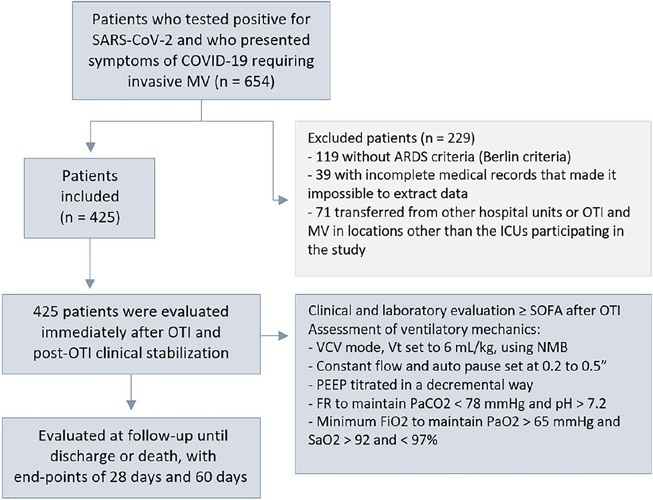
-
Review Article
Cough peak flow to predict extubation outcome: a systematic review and meta-analysis
Rev Bras Ter Intensiva. 2021;33(3):445-456
Abstract
Review ArticleCough peak flow to predict extubation outcome: a systematic review and meta-analysis
Rev Bras Ter Intensiva. 2021;33(3):445-456
DOI 10.5935/0103-507X.20210060
Views0See moreAbstract
Objective:
This systematic review was designed to assess the usefulness of cough peak flow to predict the extubation outcome in subjects who passed a spontaneous breathing trial.
Methods:
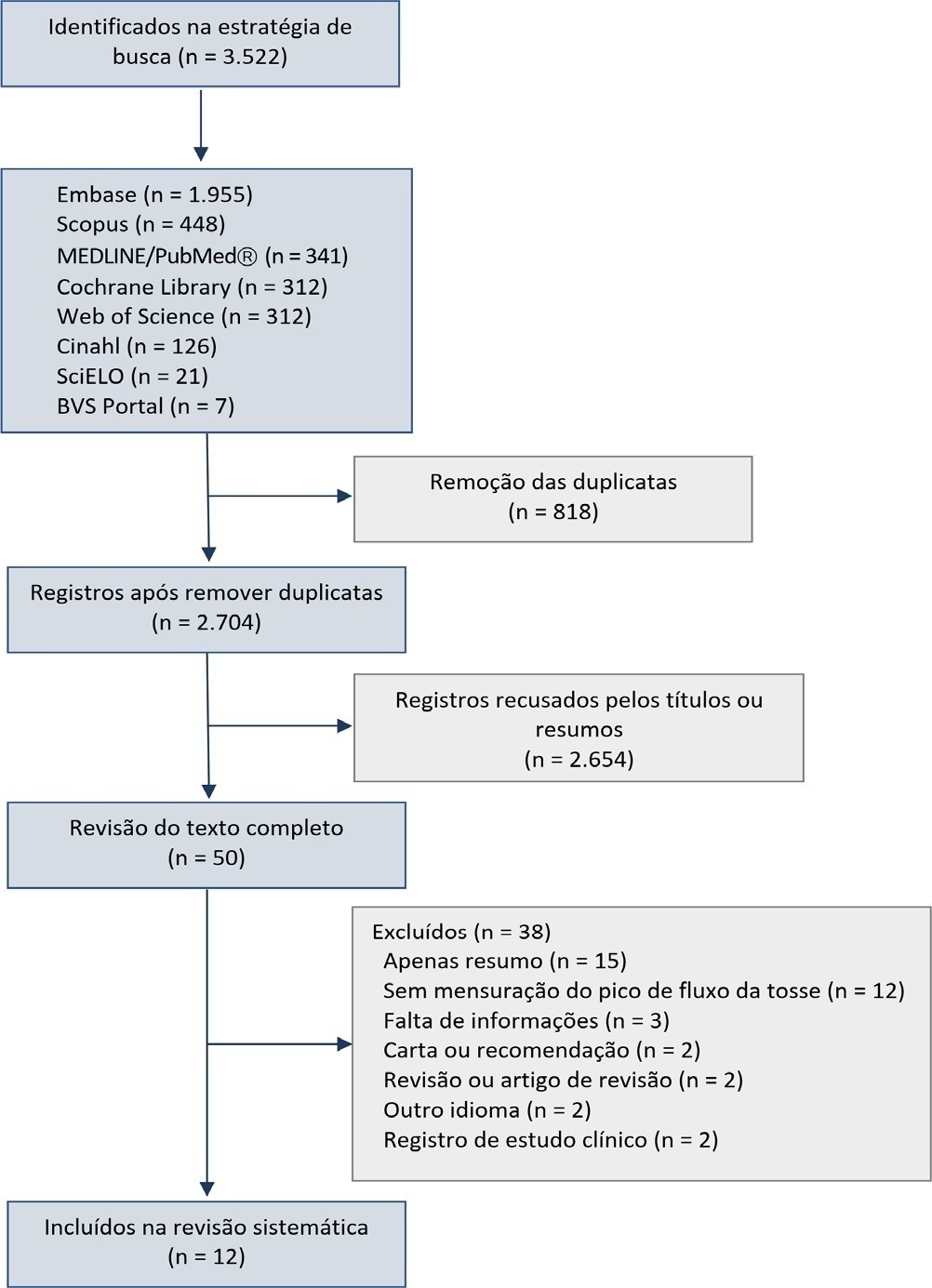
The search covered the scientific databases MEDLINE, Lilacs, Ibecs, Cinahl, SciELO, Cochrane, Scopus, Web of Science and gray literature. The Quality Assessment of Diagnostic Accuracy Studies was used to assess the methodological quality and risk of study bias. The statistical heterogeneity of the likelihood (LR) and diagnostic odds ratios were evaluated using forest plots and Cochran’s Q statistic, and a crosshair summary Receiver Operating Characteristic plot using the multiple cutoffs model was calculated.
Results:
We initially retrieved 3,522 references from the databases; among these, 12 studies including 1,757 subjects were selected for the qualitative analysis. Many studies presented an unclear risk of bias in the “patient selection” and “flow and time” criteria. Among the 12 included studies, seven presented “high risk” and five “unclear risk” for the item “reference standard.” The diagnostic performance of the cough peak flow for the extubation outcome was low to moderate when we considered the results from all included studies, with a +LR of 1.360 (95%CI 1.240 – 1.530), -LR of 0.218 (95%CI 0.159 – 0.293) and a diagnostic odds ratio of 6.450 (95%CI 4.490 – 9.090). A subgroup analysis including only the studies with a cutoff between 55 and 65 L/minute showed a slightly better, although still moderate, performance.
Conclusion:
A cough peak flow assessment considering a cutoff between 55 and 65L/minute may be useful as a complementary measurement prior to extubation. Additional well-designed studies are necessary to identify the best method and equipment to record the cough peak flow as well as the best cutoff.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




