Abstract
Crit Care Sci. 2024;36:e20240158en
DOI 10.62675/2965-2774.20240158-pt
To evaluate the association of biomarkers with successful ventilatory weaning in COVID-19 patients.
An observational, retrospective, and single-center study was conducted between March 2020 and April 2021. C-reactive protein, total lymphocytes, and the neutrophil/lymphocyte ratio were evaluated during attrition and extubation, and the variation in these biomarker values was measured. The primary outcome was successful extubation. ROC curves were drawn to find the best cutoff points for the biomarkers based on sensitivity and specificity. Statistical analysis was performed using logistic regression.
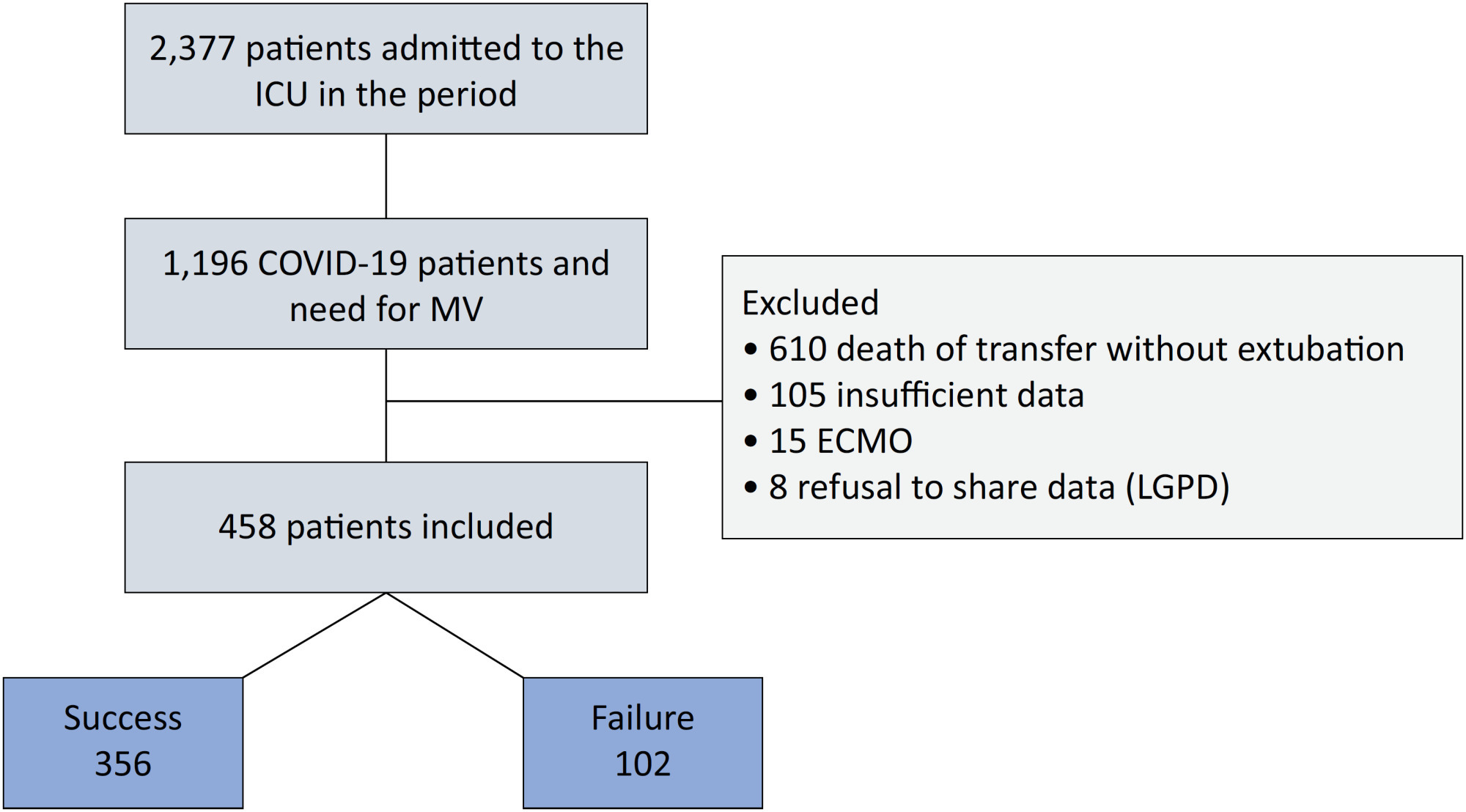
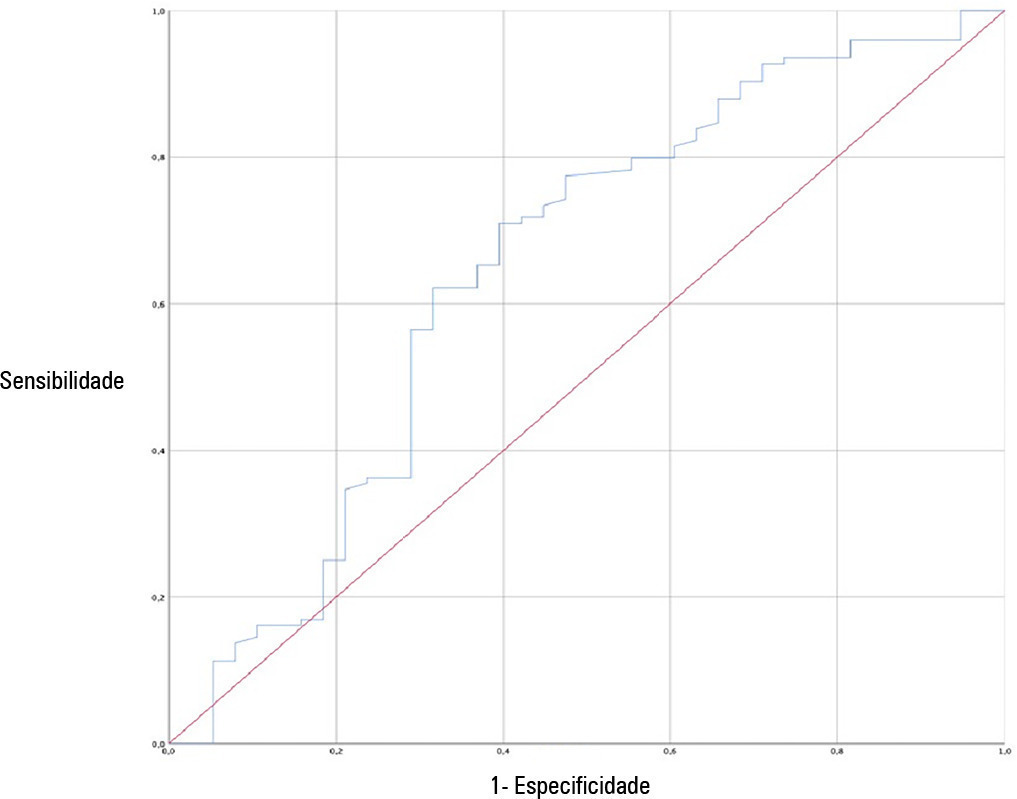
Of the 2,377 patients admitted to the intensive care unit, 458 were included in the analysis, 356 in the Successful Weaning Group and 102 in the Failure Group. The cutoff points found from the ROC curves were −62.4% for C-reactive protein, +45.7% for total lymphocytes, and −32.9% for neutrophil/lymphocyte ratio. These points were significantly associated with greater extubation success. In the multivariate analysis, only C-reactive protein variation remained statistically significant (OR 2.6; 95%CI 1.51 – 4.5; p < 0.001).
In this study, a decrease in C-reactive protein levels was associated with successful extubation in COVID-19 patients. Total lymphocytes and the neutrophil/lymphocyte ratio did not maintain the association after multivariate analysis. However, a decrease in C-reactive protein levels should not be used as a sole variable to identify COVID-19 patients suitable for weaning; as in our study, the area under the ROC curve demonstrated poor accuracy in discriminating extubation outcomes, with low sensitivity and specificity.
Abstract
Crit Care Sci. 2023;35(2):163-167
DOI 10.5935/2965-2774.20230009-pt
To assess the outcome of extubation in COVID-19 patients and the use of noninvasive ventilation in the weaning process.
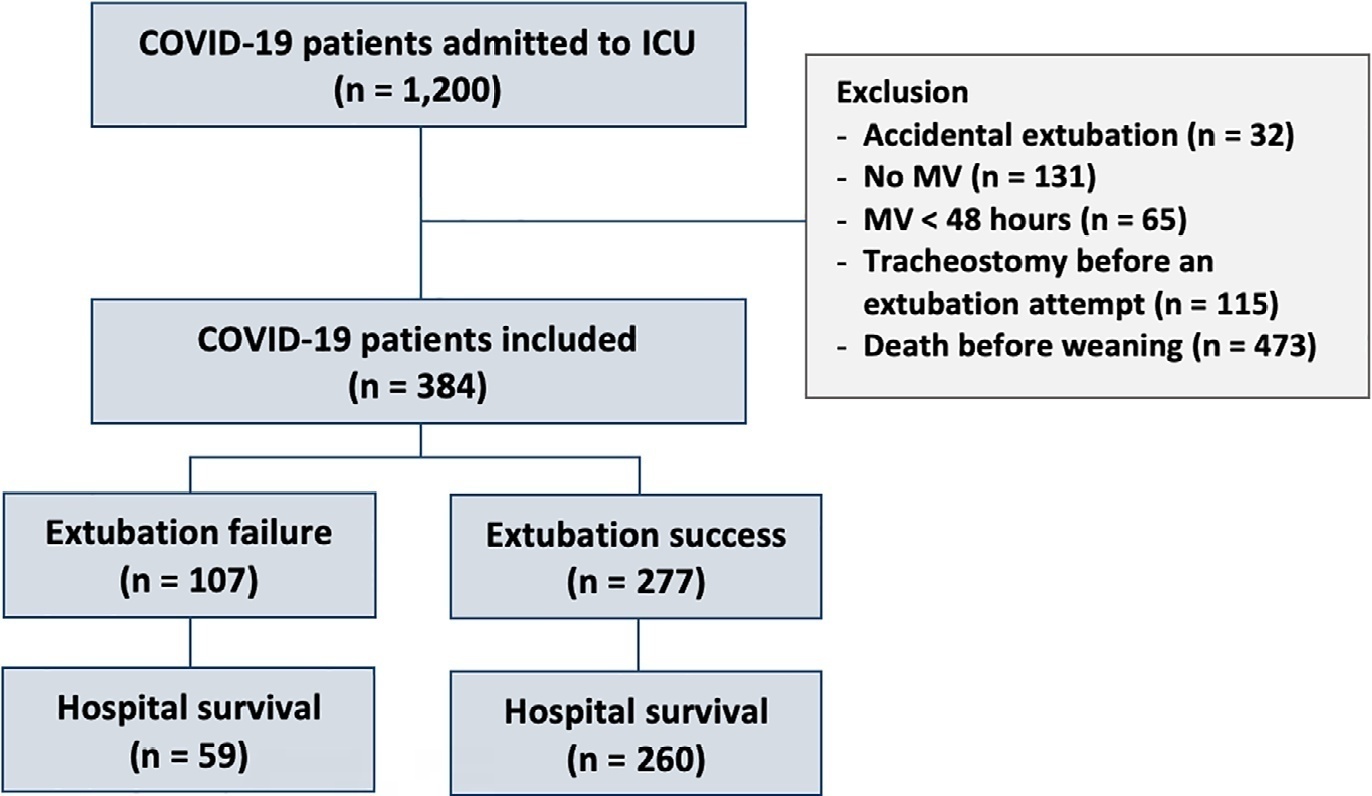
This retrospective, observational, single-center study was conducted in COVID-19 patients aged 18 years or older who were admitted to an intensive care unit between April 2020 and December 2021, placed under mechanical ventilation for more than 48 hours and progressed to weaning. Early extubation was defined as extubation without a spontaneous breathing trial and immediate use of noninvasive ventilation after extubation. In patients who underwent a spontaneous breathing trial, noninvasive ventilation could be used as prophylactic ventilatory assistance when started immediately after extubation (prophylactic noninvasive ventilation) or as rescue therapy in cases of postextubation respiratory failure (therapeutic noninvasive ventilation). The primary outcome was extubation failure during the intensive care unit stay.
Three hundred eighty-four extubated patients were included. Extubation failure was observed in 107 (27.9%) patients. Forty-seven (12.2%) patients received prophylactic noninvasive ventilation. In 26 (6.8%) patients, early extubation was performed with immediate use of noninvasive ventilation. Noninvasive ventilation for the management of postextubation respiratory failure was administered to 64 (16.7%) patients.
We found that COVID-19 patients had a high rate of extubation failure. Despite the high risk of extubation failure, we observed low use of prophylactic noninvasive ventilation in these patients.
Abstract
Crit Care Sci. 2023;35(1):37-43
DOI 10.5935/2965-2774.20230275-pt
To compare the diagnostic performance of maximal expiratory pressure with maximal expiratory pressure during induced cough for predicting extubation failure within 72 hours in patients who completed a spontaneous breathing trial (SBT).
The study was conducted between October 2018 and September 2019. All patients aged over 18 years admitted to the intensive care unit who required invasive mechanical ventilation for over 48 hours and successfully completed a spontaneous breathing trial were included. The maximal expiratory pressure was assessed with a unidirectional valve for 40 seconds, and verbal encouragement was given. The maximal expiratory pressure during induced cough was measured with slow instillation of 2mL of a 0.9% saline solution. The primary outcome variable was extubation failure.
Eighty patients were included, of which 43 (54%) were male. Twenty-two patients [27.5% (95%CI 18.9 - 38.1)] failed extubation within 72 hours. Differences were observed in the maximal expiratory pressure during induced cough between the group who failed extubation, with a median of 0cmH2O (P25-75: 0 - 90), and the group without extubation failure, with a median of 120cmH2O (P25-75: 73 - 120); p < 0.001.
In patients who completed a spontaneous breathing trial, the maximal expiratory pressure during induced cough had a higher diagnostic performance for predicting extubation failure within 72 hours.

Abstract
Crit Care Sci. 2023;35(1):66-72
DOI 10.5935/2965-2774.20230312-pt
To evaluate whether a model of a daily fitness checklist for spontaneous breathing tests is able to identify predictive variables of extubation failure in pediatric patients admitted to a Brazilian intensive care unit.
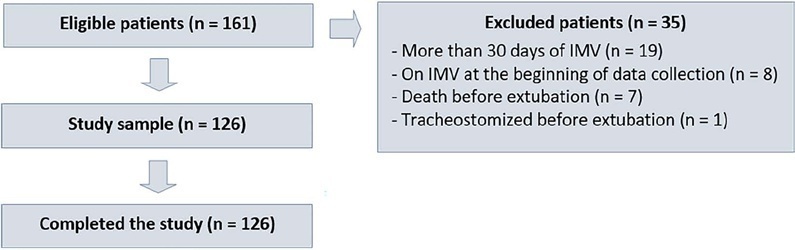
This was a single-center, cross-sectional study with prospective data collection. The checklist model comprised 20 items and was applied to assess the ability to perform spontaneous breathing tests.
The sample consisted of 126 pediatric patients (85 males (67.5%)) on invasive mechanical ventilation, for whom 1,217 daily assessments were applied at the bedside. The weighted total score of the prediction model showed the highest discriminatory power for the spontaneous breathing test, with sensitivity and specificity indices for fitness failure of 89.7% or success of 84.6%. The cutoff point suggested by the checklist was 8, with a probability of extubation failure less than 5%. Failure increased progressively with increasing score, with a maximum probability of predicting extubation failure of 85%.
The extubation failure rate with the use of this model was within what is acceptable in the literature. The daily checklist model for the spontaneous breathing test was able to identify predictive variables of failure in the extubation process in pediatric patients.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):360-366
DOI 10.5935/0103-507X.20220477-en
To investigate the applicability of the Respiratory Rate-Oxygenation Index to identify the risk of high-flow nasal cannula failure in post-extubation pneumonia patients.
This was a 2-year retrospective observational study conducted in a reference hospital in Bogotá, Colombia. All patients in whom post-extubation high-flow nasal cannula therapy was used as a bridge to extubation were included in the study. The Respiratory Rate-Oxygenation Index was calculated to assess the risk of post-extubation high-flow nasal cannula failure.
A total of 162 patients were included in the study. Of these, 23.5% developed high-flow nasal cannula failure. The Respiratory Rate-Oxygenation Index was significantly lower in patients who had high-flow nasal cannula failure [median (IQR): 10.0 (7.7 - 14.4) versus 12.6 (10.1 - 15.6); p = 0.006]. Respiratory Rate-Oxygenation Index > 4.88 showed a crude OR of 0.23 (95%CI 0.17 - 0.30) and an adjusted OR of 0.89 (95%CI 0.81 - 0.98) stratified by severity and comorbidity. After logistic regression analysis, the Respiratory Rate-Oxygenation Index had an adjusted OR of 0.90 (95%CI 0.82 - 0.98; p = 0.026). The area under the Receiver Operating Characteristic curve for extubation failure was 0.64 (95%CI 0.53 - 0.75; p = 0.06). The Respiratory Rate-Oxygenation Index did not show differences between patients who survived and those who died during the intensive care unit stay.
The Respiratory Rate-Oxygenation Index is an accessible tool to identify patients at risk of failing high-flow nasal cannula post-extubation treatment. Prospective studies are needed to broaden the utility in this scenario.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):422-427
DOI 10.5935/0103-507X.20210057
To assess whether there is an association between 48-hour postextubation fluid balance and extubation failure.
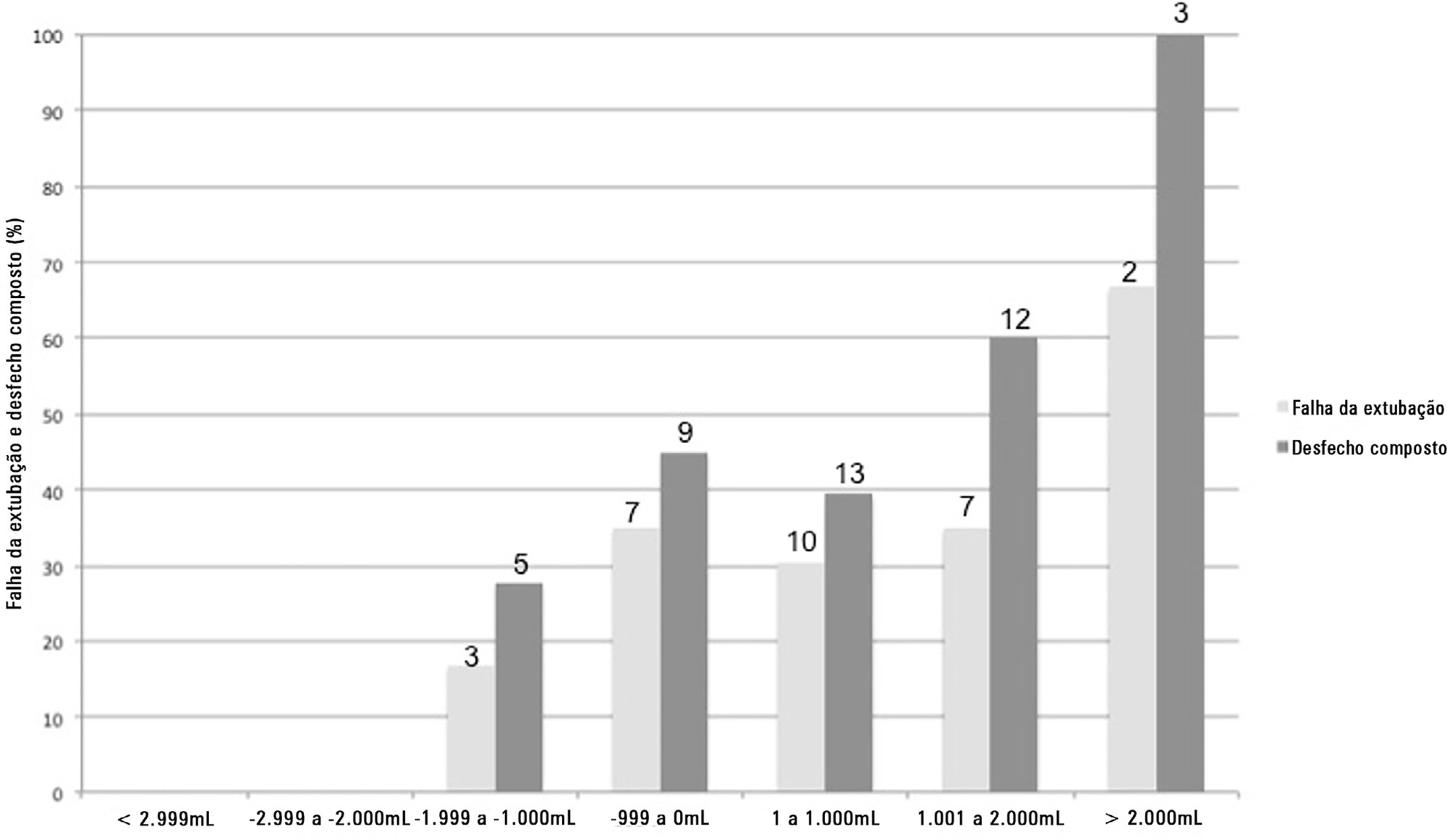
This was a prospective cohort study that included patients admitted to the intensive care unit of a tertiary hospital in southern Brazil from March 2019 to December 2019. Patients who required mechanical ventilation for at least 24 hours and who were extubated during the study period were included. The primary outcome was extubation failure, considered as the need for reintubation in the first 72 hours after extubation. The secondary outcome was a combined outcome with extubation failure or the need for therapeutic noninvasive ventilation.
A total of 101 patients were included. Extubation failure was observed in 29 (28.7%) patients. In univariate analysis, patients with a negative 48-hour postextubation fluid balance higher than one liter had a lower rate of extubation failure (12.0%) than patients with a negative 48-hour postextubation fluid balance lower than 1L (34.2%; p = 0.033). Mechanical ventilation duration and negative 48-hour postextubation fluid balance lower than one liter were associated with extubation failure when corrected for Simplified Acute Physiology Score 3 in multivariate analysis. When we evaluated the combined outcome, only negative 48-hour postextubation lower than 1L maintained an association when corrected for for Simplified Acute Physiology Score 3 and mechanical ventilation duration.
The 48-hour postextubation fluid balance is associated with extubation failure. Further studies are necessary to assess whether avoiding positive fluid balance in this period might improve weaning outcomes.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):445-456
DOI 10.5935/0103-507X.20210060
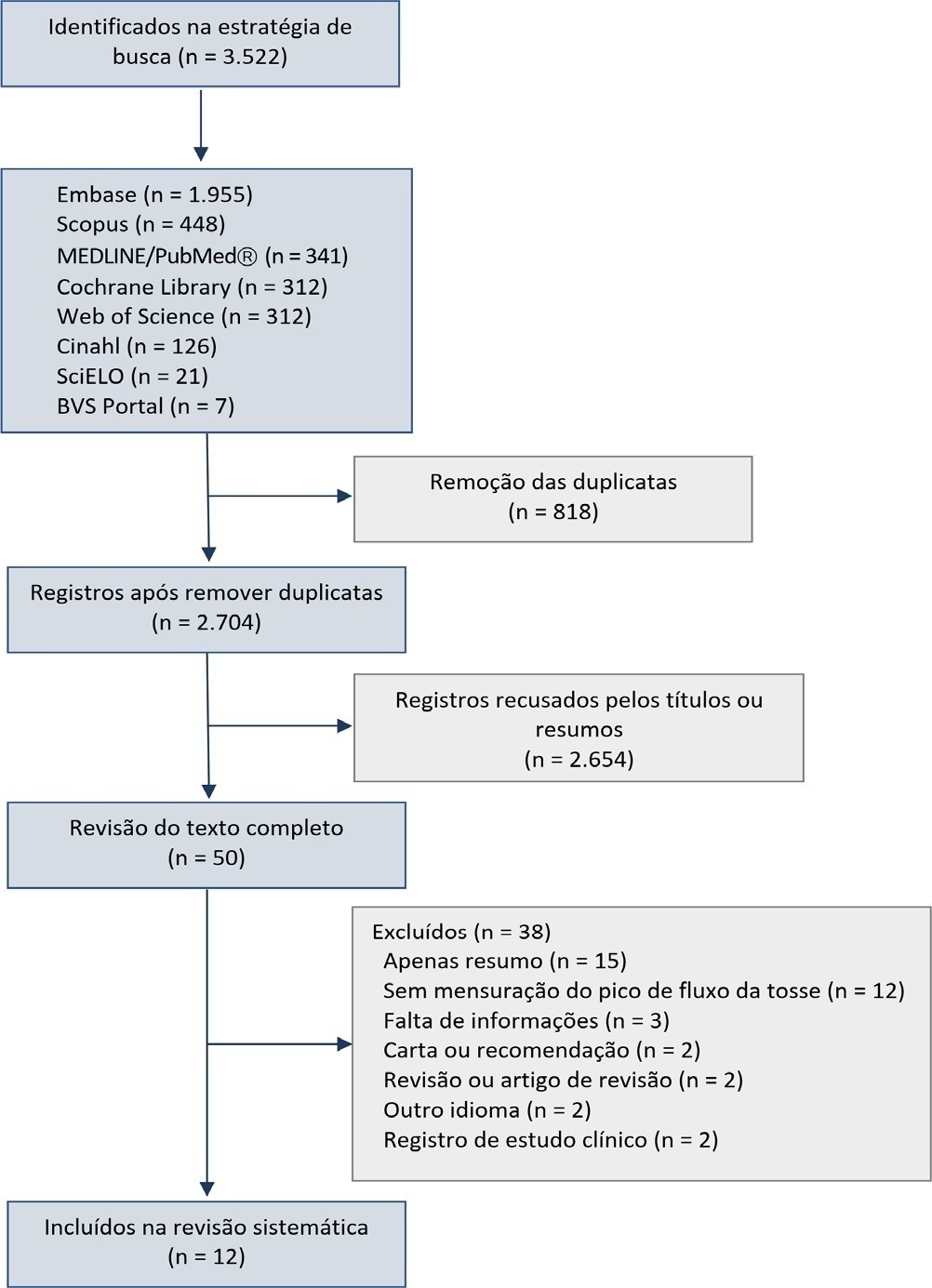
This systematic review was designed to assess the usefulness of cough peak flow to predict the extubation outcome in subjects who passed a spontaneous breathing trial.
The search covered the scientific databases MEDLINE, Lilacs, Ibecs, Cinahl, SciELO, Cochrane, Scopus, Web of Science and gray literature. The Quality Assessment of Diagnostic Accuracy Studies was used to assess the methodological quality and risk of study bias. The statistical heterogeneity of the likelihood (LR) and diagnostic odds ratios were evaluated using forest plots and Cochran’s Q statistic, and a crosshair summary Receiver Operating Characteristic plot using the multiple cutoffs model was calculated.
We initially retrieved 3,522 references from the databases; among these, 12 studies including 1,757 subjects were selected for the qualitative analysis. Many studies presented an unclear risk of bias in the “patient selection” and “flow and time” criteria. Among the 12 included studies, seven presented “high risk” and five “unclear risk” for the item “reference standard.” The diagnostic performance of the cough peak flow for the extubation outcome was low to moderate when we considered the results from all included studies, with a +LR of 1.360 (95%CI 1.240 - 1.530), -LR of 0.218 (95%CI 0.159 - 0.293) and a diagnostic odds ratio of 6.450 (95%CI 4.490 - 9.090). A subgroup analysis including only the studies with a cutoff between 55 and 65 L/minute showed a slightly better, although still moderate, performance.
A cough peak flow assessment considering a cutoff between 55 and 65L/minute may be useful as a complementary measurement prior to extubation. Additional well-designed studies are necessary to identify the best method and equipment to record the cough peak flow as well as the best cutoff.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):304-311
DOI 10.5935/0103-507X.20210039
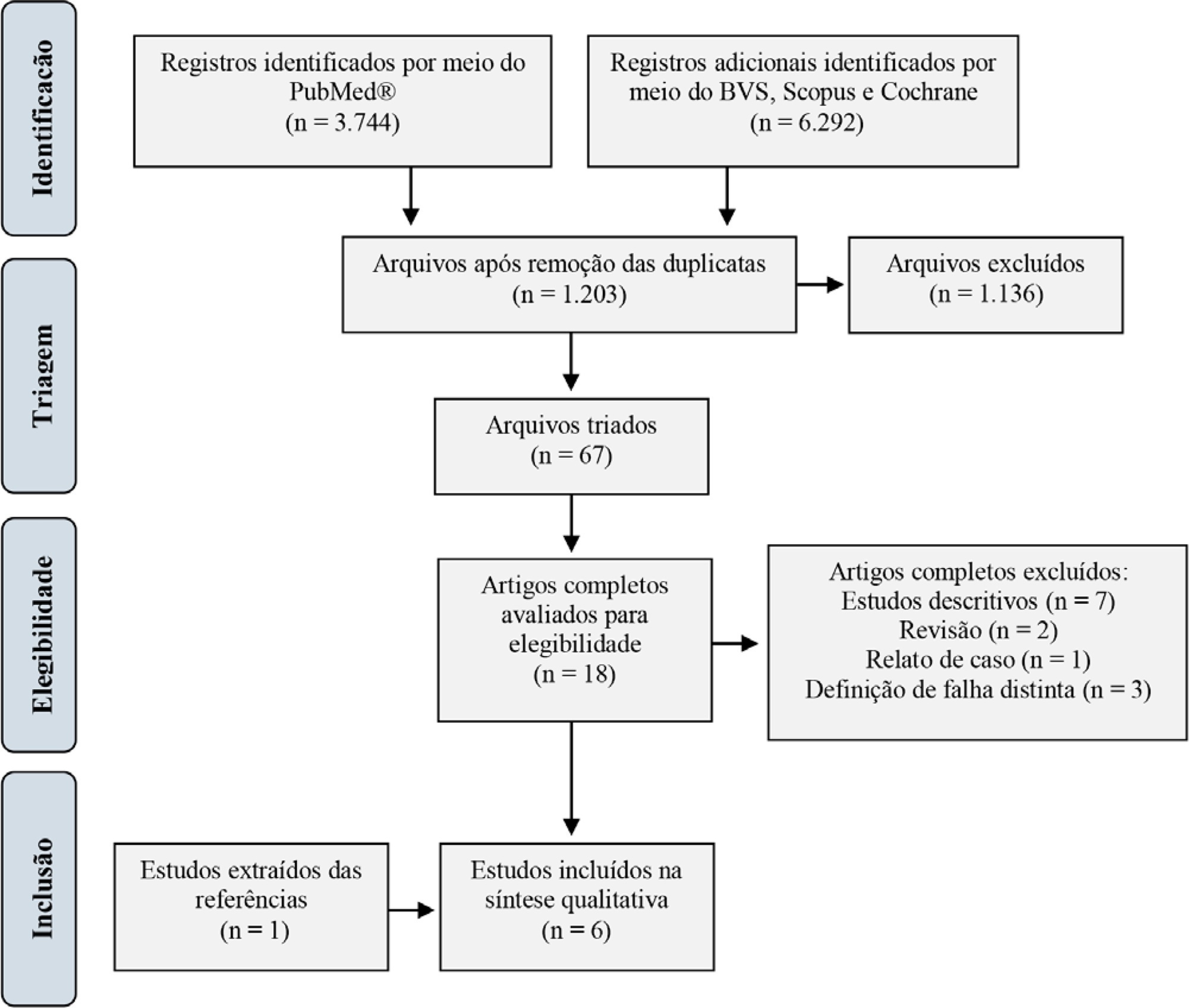
For extubation in pediatric patients, the evaluation of readiness is strongly recommended. However, a device or practice that is superior to clinical judgment has not yet been accurately determined. Thus, it is important to conduct a review on the techniques of choice in clinical practice to predict extubation failure in pediatric patients. Based on a search in the PubMed®, Biblioteca Virtual em Saúde, Cochrane Library and Scopus databases, we conducted a survey of the predictive variables of extubation failure most commonly used in clinical practice in pediatric patients. Of the eight predictors described, the three most commonly used were the spontaneous breathing test, the rapid shallow breathing index and maximum inspiratory pressure. Although the disparity of the data presented in the studies prevented statistical treatment, it was still possible to describe and analyze the performance of these tests.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) ICU (25) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)