Abstract
Crit Care Sci. 2023;35(1):37-43
DOI 10.5935/2965-2774.20230275-pt
To compare the diagnostic performance of maximal expiratory pressure with maximal expiratory pressure during induced cough for predicting extubation failure within 72 hours in patients who completed a spontaneous breathing trial (SBT).
The study was conducted between October 2018 and September 2019. All patients aged over 18 years admitted to the intensive care unit who required invasive mechanical ventilation for over 48 hours and successfully completed a spontaneous breathing trial were included. The maximal expiratory pressure was assessed with a unidirectional valve for 40 seconds, and verbal encouragement was given. The maximal expiratory pressure during induced cough was measured with slow instillation of 2mL of a 0.9% saline solution. The primary outcome variable was extubation failure.
Eighty patients were included, of which 43 (54%) were male. Twenty-two patients [27.5% (95%CI 18.9 - 38.1)] failed extubation within 72 hours. Differences were observed in the maximal expiratory pressure during induced cough between the group who failed extubation, with a median of 0cmH2O (P25-75: 0 - 90), and the group without extubation failure, with a median of 120cmH2O (P25-75: 73 - 120); p < 0.001.
In patients who completed a spontaneous breathing trial, the maximal expiratory pressure during induced cough had a higher diagnostic performance for predicting extubation failure within 72 hours.

Abstract
Rev Bras Ter Intensiva. 2017;29(4):466-475
DOI 10.5935/0103-507X.20170063
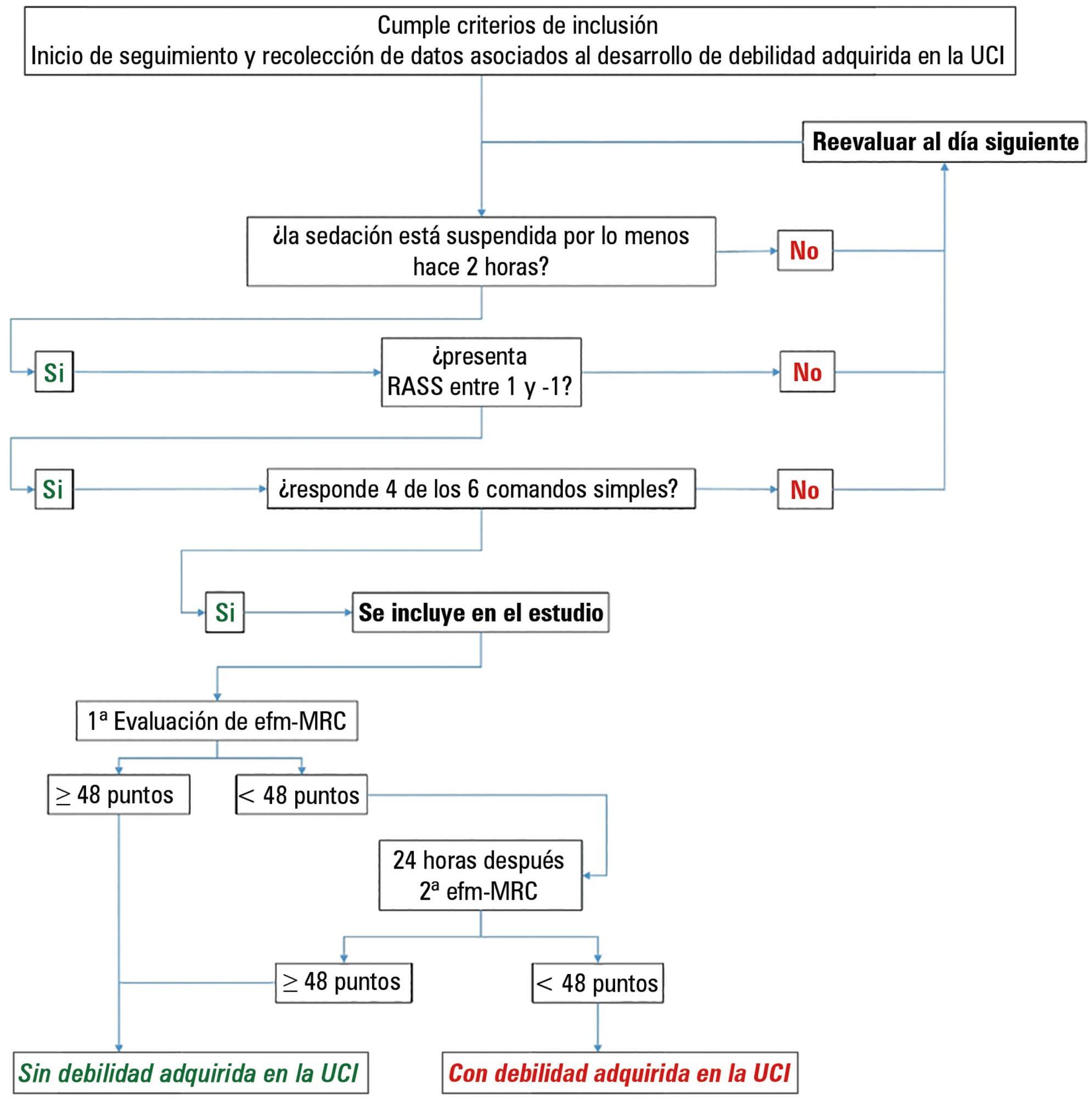
This paper sought to determine the accumulated incidence and analyze the risk factors associated with the development of weakness acquired in the intensive care unit and its relationship to inspiratory weakness.
We conducted a prospective cohort study at a single center, multipurpose medical-surgical intensive care unit. We included adult patients who required mechanical ventilation ≥ 24 hours between July 2014 and January 2016. No interventions were performed. Demographic data, clinical diagnoses, the factors related to the development of intensive care unit -acquired weakness, and maximal inspiratory pressure were recorded.
Of the 111 patients included, 66 developed intensive care unit -acquired weakness, with a cumulative incidence of 40.5% over 18 months. The group with intensive care unit-acquired weakness were older (55.9 ± 17.6 versus 45.8 ± 16.7), required more mechanical ventilation (7 [4 - 10] days versus 4 [2 - 7.3] days), and spent more time in the intensive care unit (15.5 [9.2 - 22.8] days versus 9 [6 - 14] days). More patients presented with delirium (68% versus 39%), hyperglycemia > 3 days (84% versus 59%), and positive balance > 3 days (73.3% versus 37%). All comparisons were significant at p < 0.05. A multiple logistic regression identified age, hyperglycemia ≥ 3 days, delirium, and mechanical ventilation > 5 days as independent predictors of intensive care unit-acquired weakness. Low maximal inspiratory pressure was associated with intensive care unit-acquired weakness (p < 0.001), and the maximum inspiratory pressure cut-off value of < 36cmH2O had sensitivity and specificity values of 31.8% and 95.5%, respectively, when classifying patients with intensive care unit-acquired weakness.
The intensive care unit acquired weakness is a condition with a high incidence in our environment. The development of intensive care unit-acquired weakness was associated with age, delirium, hyperglycemia, and mechanical ventilation > 5 days. The maximum inspiratory pressure value of ≥ 36cmH2O was associated with a high diagnostic value to exclude the presence of intensive care unit -acquired weakness.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)