Abstract
Rev Bras Ter Intensiva. 2021;33(1):138-145
DOI 10.5935/0103-507X.20210015
To double the percentage of time within the 100 - 180mg/dL blood glucose range in the first three months following a phased implementation of a formal education program, and then, of an insulin therapy protocol, without entailing an increased incidence of hypoglycemia.
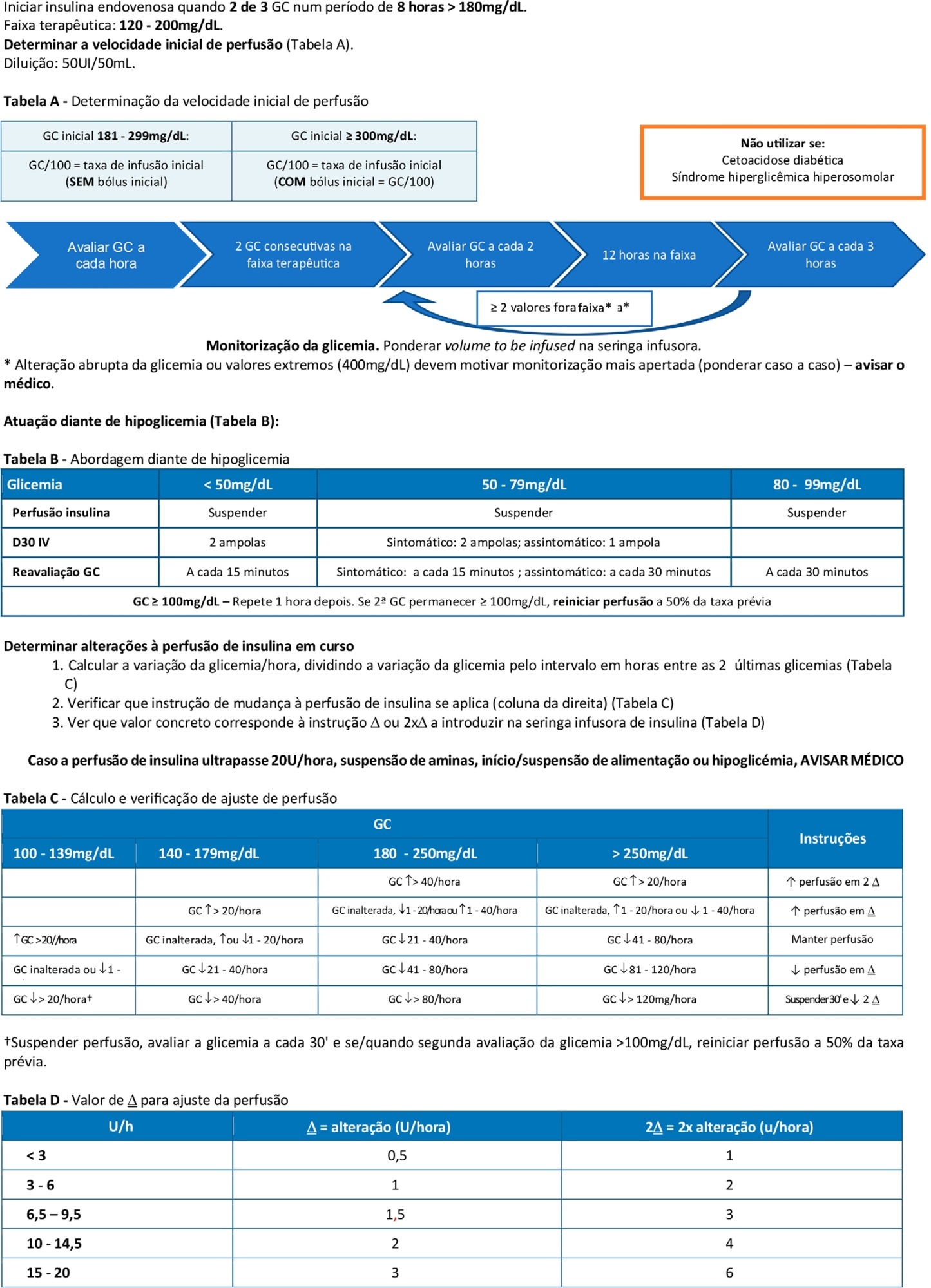
The pre-intervention glycemic control was assessed retrospectively. Next, were carried out the implementation of a formal education program, distribution of manual algorithms for intravenous insulin therapy - optimized by the users, based on the modified Yale protocol - and informal training of the nursing staff. The use of electronic blood glucose control systems was supported, and the results were recorded prospectively.
The first phase of the program (formal education) lead to improvement of the time within the euglycemic interval (28% to 37%). In the second phase, euglycemia was achieved 66% of the time, and the incidence of hypoglycemia was decreased. The percentage of patients on intravenous insulin infusion at 48 hours from admission increased from 6% to 35%.
The phased implementation of a formal education program, fostering the use of electronic insulin therapy protocols and dynamic manuals, received good adherence and has shown to be safe and effective for blood glucose control in critically ill patients, with a concomitant decrease in hypoglycemia.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):471-478
DOI 10.5935/0103-507X.20180068
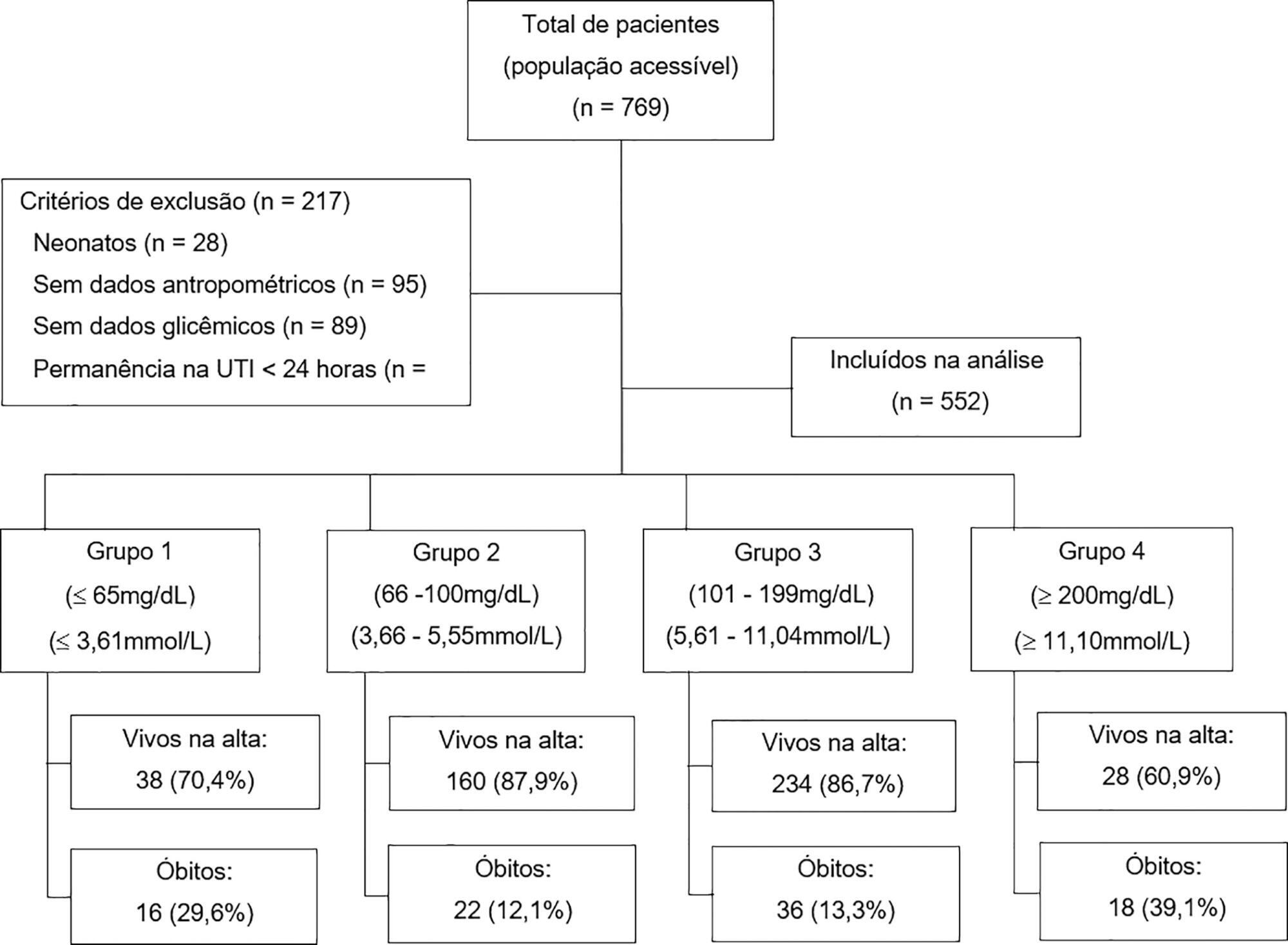
To analyze the association between glycemia levels upon pediatric intensive care unit admission and mortality in patients hospitalized.
A retrospective cohort of pediatric intensive care unit patients admitted to the Instituto Nacional de Salud del Niño between 2012 and 2013. A Poisson regression model with robust variance was used to quantify the association. Diagnostic test performance evaluation was used to describe the sensitivity, specificity, positive predictive value, negative predictive value and likelihood ratios for each range of glycemia.
In total, 552 patients were included (median age 23 months, age range 5 months to 79.8 months). The mean glycemia level upon admission was 121.3mg/dL (6.73mmol/L). Ninety-two (16.6%) patients died during hospitalization. In multivariable analyses, significant associations were found between glycemia < 65mg/dL (3.61mmol/L) (RR: 2.01, 95%CI 1.14 - 3.53), glycemia > 200mg/dL (> 11.1mmol/L) (RR: 2.91, 95%CI 1.71 - 4.55), malnutrition (RR: 1.53, 95%CI 1.04 - 2.25), mechanical ventilation (RR: 3.71, 95%CI 1.17 - 11.76) and mortality at discharge. There was low sensitivity (between 17.39% and 39.13%) and high specificity (between 49.13% and 91.74%) for different glucose cut-off levels.
There was an increased risk of death at discharge in patients who developed hypoglycemia and hyperglycemia upon admission to the pediatric intensive care unit. Certain glucose ranges (> 200mg/dL (> 11.1mmol/L) and < 65mg/dL (3.61mmol/L)) have high specificity as predictors of death at discharge.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):466-475
DOI 10.5935/0103-507X.20170063
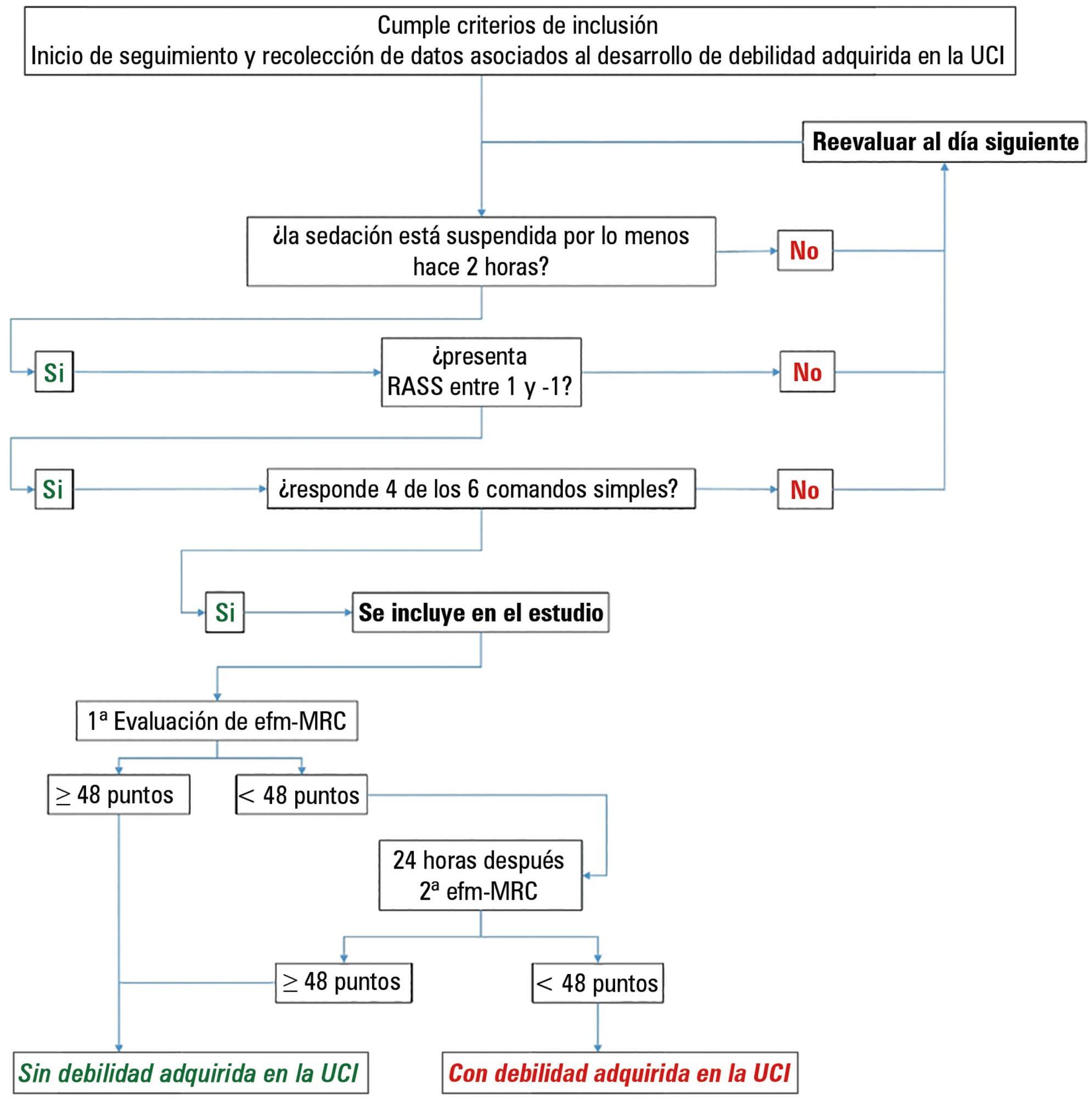
This paper sought to determine the accumulated incidence and analyze the risk factors associated with the development of weakness acquired in the intensive care unit and its relationship to inspiratory weakness.
We conducted a prospective cohort study at a single center, multipurpose medical-surgical intensive care unit. We included adult patients who required mechanical ventilation ≥ 24 hours between July 2014 and January 2016. No interventions were performed. Demographic data, clinical diagnoses, the factors related to the development of intensive care unit -acquired weakness, and maximal inspiratory pressure were recorded.
Of the 111 patients included, 66 developed intensive care unit -acquired weakness, with a cumulative incidence of 40.5% over 18 months. The group with intensive care unit-acquired weakness were older (55.9 ± 17.6 versus 45.8 ± 16.7), required more mechanical ventilation (7 [4 - 10] days versus 4 [2 - 7.3] days), and spent more time in the intensive care unit (15.5 [9.2 - 22.8] days versus 9 [6 - 14] days). More patients presented with delirium (68% versus 39%), hyperglycemia > 3 days (84% versus 59%), and positive balance > 3 days (73.3% versus 37%). All comparisons were significant at p < 0.05. A multiple logistic regression identified age, hyperglycemia ≥ 3 days, delirium, and mechanical ventilation > 5 days as independent predictors of intensive care unit-acquired weakness. Low maximal inspiratory pressure was associated with intensive care unit-acquired weakness (p < 0.001), and the maximum inspiratory pressure cut-off value of < 36cmH2O had sensitivity and specificity values of 31.8% and 95.5%, respectively, when classifying patients with intensive care unit-acquired weakness.
The intensive care unit acquired weakness is a condition with a high incidence in our environment. The development of intensive care unit-acquired weakness was associated with age, delirium, hyperglycemia, and mechanical ventilation > 5 days. The maximum inspiratory pressure value of ≥ 36cmH2O was associated with a high diagnostic value to exclude the presence of intensive care unit -acquired weakness.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):364-372
DOI 10.5935/0103-507X.20170054
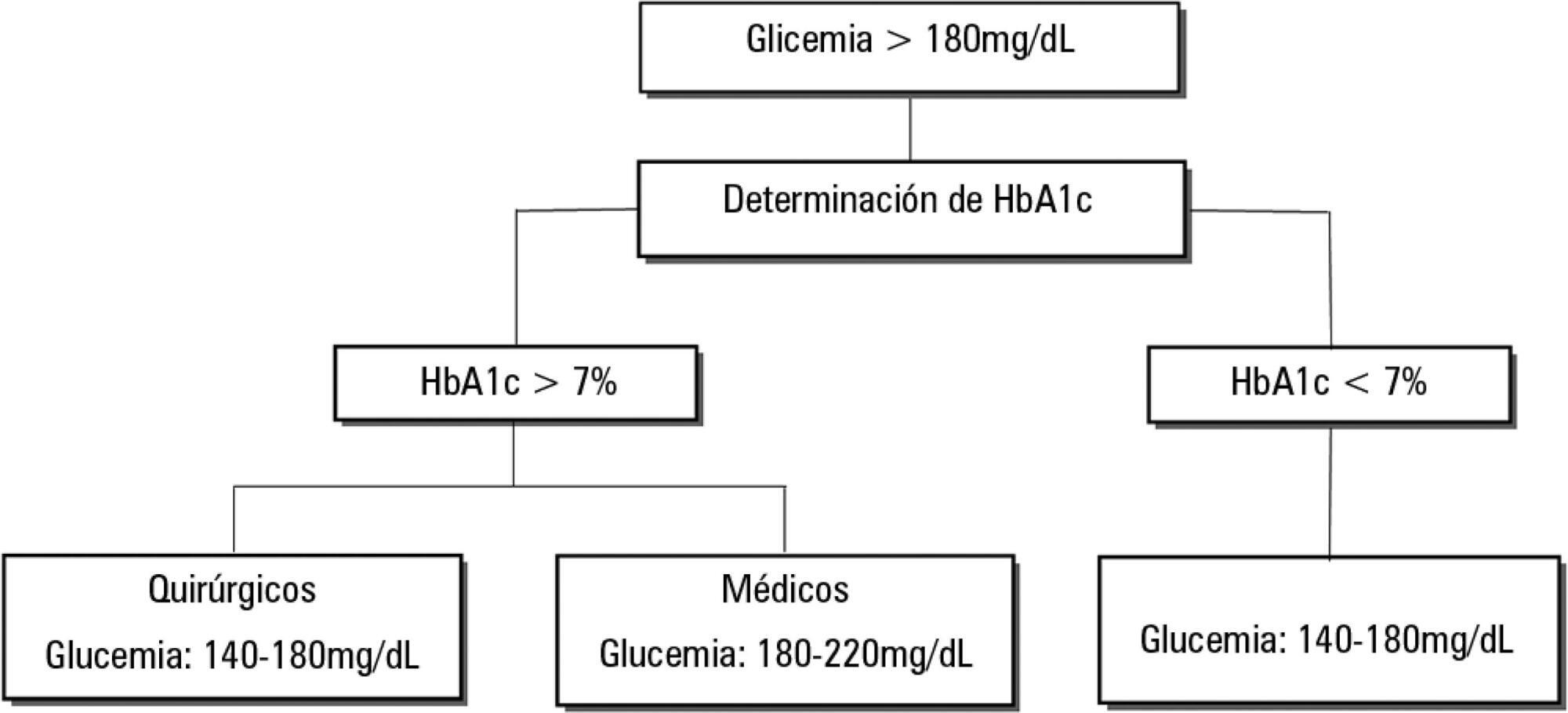
Dysglycemia in critically ill patients (hyperglycemia, hypoglycemia, glycemic variability and time in range) is a biomarker of disease severity and is associated with higher mortality. However, this impact appears to be weakened in patients with previous diabetes mellitus, particularly in those with poor premorbid glycemic control; this phenomenon has been called "diabetes paradox". This phenomenon determines that glycated hemoglobin (HbA1c) values should be considered in choosing glycemic control protocols on admission to an intensive care unit and that patients' target blood glucose ranges should be adjusted according to their HbA1c values. Therefore, HbA1c emerges as a simple tool that allows information that has therapeutic utility and prognostic value to be obtained in the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):71-76
DOI 10.5935/0103-507X.20140011
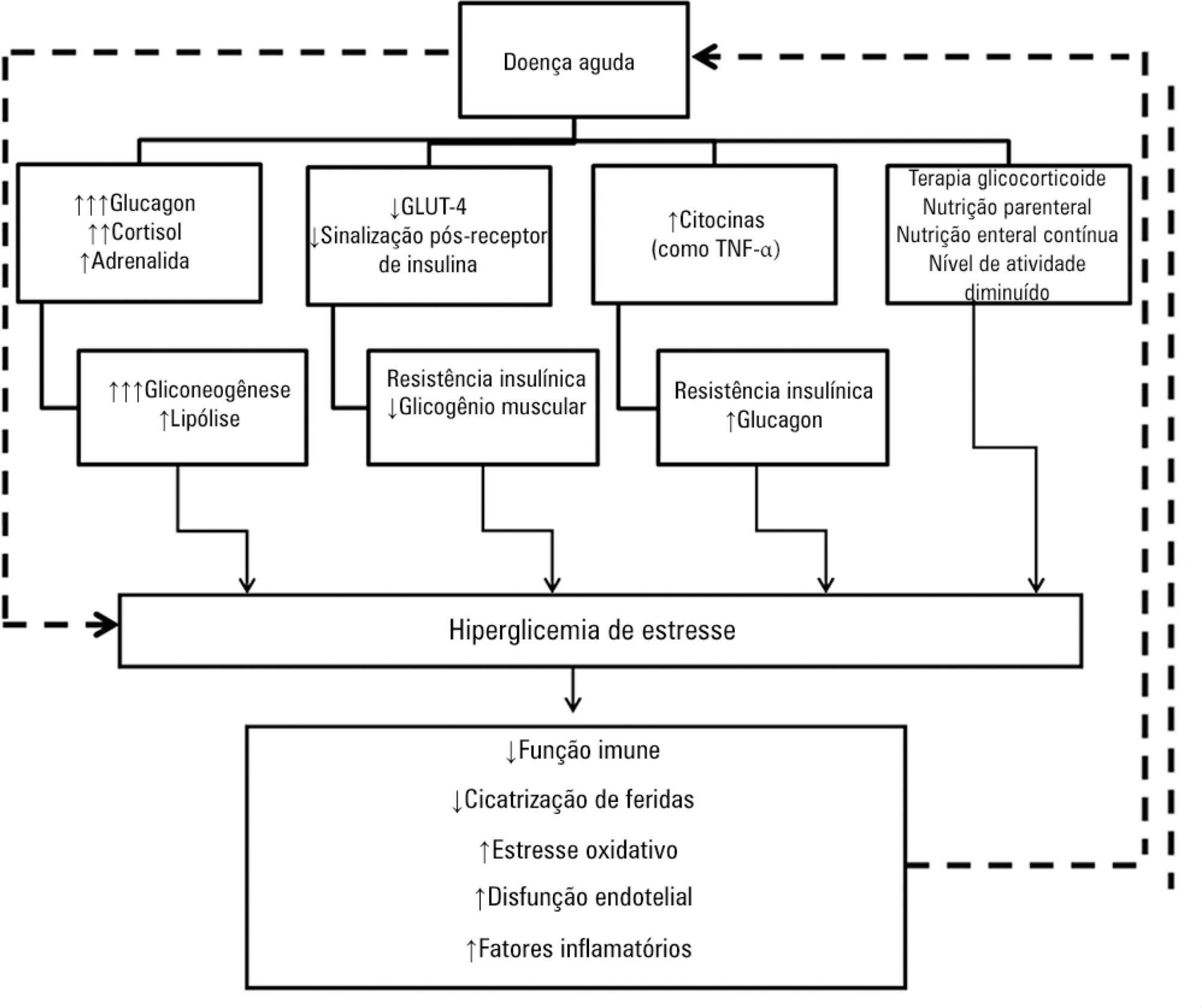
Hyperglycemia is a commonly encountered issue in critically ill patients in the intensive care setting. The presence of hyperglycemia is associated with increased morbidity and mortality, regardless of the reason for admission (e.g., acute myocardial infarction, status post-cardiovascular surgery, stroke, sepsis). However, the pathophysiology and, in particular, the treatment of hyperglycemia in the critically ill patient remain controversial. In clinical practice, several aspects must be taken into account in the management of these patients, including blood glucose targets, history of diabetes mellitus, the route of nutrition (enteral or parenteral), and available monitoring equipment, which substantially increases the workload of providers involved in the patients' care. This review describes the epidemiology, pathophysiology, management, and monitoring of hyperglycemia in the critically ill adult patient.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):352-356
DOI 10.1590/S0103-507X2012000400010
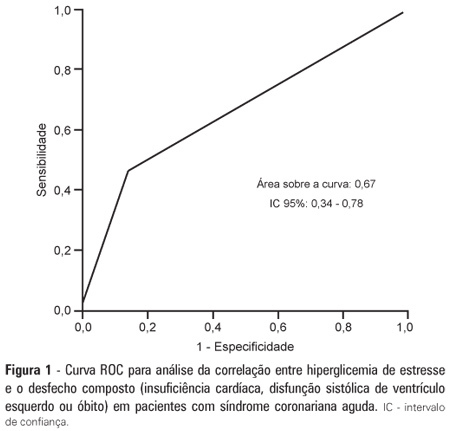
OBJECTIVE: To demonstrate the prevalence of stress hyperglycemia in a cohort of patients with acute coronary syndrome and to determine the correlation of stress hyperglycemia with death, heart failure and/or left ventricular systolic dysfunction during the intrahospital phase. METHODS: A prospective initial cohort study of hospitalized patients with acute coronary syndrome with or without ST segment elevation. The groups were compared to demonstrate the correlation between stress hyperglycemia and cardiovascular events. The chi-square test or Fisher's exact test and student's t-test were used to compare the groups with and without stress hyperglycemia. The variables with p<0.20 in the univariate analysis were submitted to logistic regression. RESULTS: In total, 363 patients with an average age of 12.45 ± 62.06 were studied. There was a predominance of males (64.2%). In total, 96 patients (26.4%) presented with stress hyperglycemia. There were no differences between the groups with or without stress hyperglycemia. The area under the ROC curve was 0.67 for the relationship between stress hyperglycemia and the composite outcome heart failure, left ventricular systolic dysfunction or death at the end of the hospital admission. The ROC curve proved that stress hyperglycemia was the predictor of the composite outcome (death, heart failure and/or ventricular dysfunction). The multivariate analysis did not indicate age, stress hyperglycemia or admission heart rate as risk factors. CONCLUSION: Stress hyperglycemia was common in the studied sample. In the univariate analysis, the presence of stress hyperglycemia was associated with such events as death, heart failure and/or intrahospital ventricular dysfunction in patients with acute coronary syndrome.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):157-161
DOI 10.1590/S0103-507X2012000200010
OBJECTIVE: Because patients hospitalized in intensive care units are at risk for poor nutrition, and nutritional therapy is not always started at an appropriate time, the present study aimed to correlate nutritional status, early nutrition, and hyperglycemia with patient mortality in an intensive care unit. METHODS: This archival cohort study used the secondary database of 453 patients who stayed at least 48 hours in an intensive care unit and were assessed for 8 days of hospitalization. Patient nutritional status was defined according to the body mass index. Early nutrition was defined as an feeding energy within the first 48 hours of hospitalization, regardless of the administration route. Blood glucose levels were monitored using a glucometer. RESULTS: A majority of patients were male (54.2%), and approximately half of patients were overweight (48.4%). At the end of the first 48 hours, 69.4% of patients had received nutrition, and only 13.5% of patients still exhibited hyperglycemia. The patients who received early nutritional therapy exhibited lower a mortality risk (p = 0.002), regardless of the presence of other factors associated with mortality. CONCLUSIONS: The significant correlation between early nutritional therapy and survival emphasizes the importance of nutrition in severely ill patients. The low frequency of hyperglycemia found in this study might indicate that the prescription of nutritional therapy and the application of an insulin protocol are appropriate at institutional intensive care units.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)