Abstract
Rev Bras Ter Intensiva. 2010;22(4):358-362
DOI 10.1590/S0103-507X2010000400008
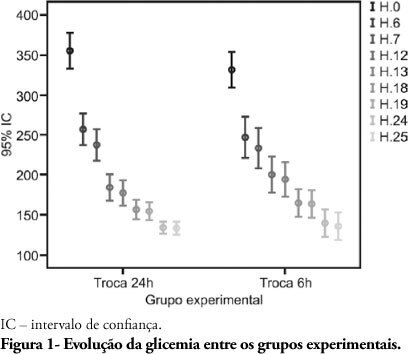
BACKGROUND: Hyperglycemia is frequent in the critically ill patient, and is a risk factor for unfavorable clinical outcomes, including mortality. During the recent years, intensive blood glucose control using intravenous insulin infusion has gained a prominent role in the critically ill patient management. There is important concern on insulin solution continued efficacy over the time, as little the literature available on this subject is poor. Lack of evidence is known to lead to inappropriate practices. This study aimed to compare the blood glucose levels between two different protocols in an intensive care unit in Porto Alegre, using the same solution concentration and two different replacement times during the first 24 hours, and additionally to assess the protocol-related hypoglycemia rate. METHODS: The medical charts of 80 patients under insulin therapy for over 24 hours during 2008 were revised; 40 patients had their insulin solution replaced every 6 hours and for 40 patients the insulin solution was replaced after 24 hours. RESULTS: The causes for admission to the intensive care unit included more frequently hypertensive (68.8%) and diabetic (45%) patients. No significant capillary blood glucose differences were seen for the every 6 or 24 hours solution replacement groups. Only 3 mild hypoglycemia cases were observed in the every 6 hours replacement group, and no hypoglycemia was seen in the 24 hours replacement group. CONCLUSION: We concluded that keeping insulin infusion, replacing the solution every 24 hours is feasible. However, longer infusion time studies are required to check for possible hypoglycemic events as insulin therapy advances.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):398-403
DOI 10.1590/S0103-507X2009000400010
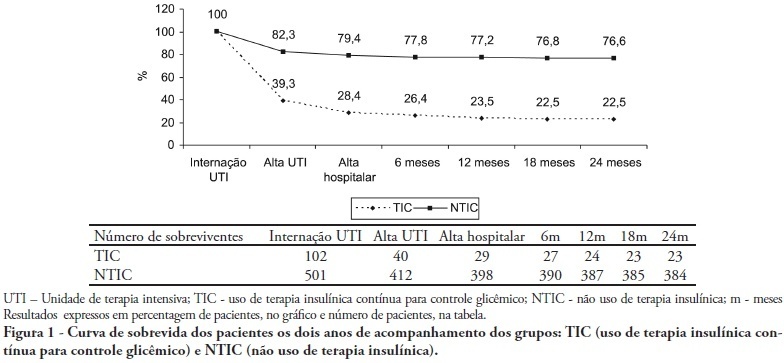
OBJECTIVES: Stress-induced hyperglycemia is frequent in critically ill patients and has been associated with increased mortality and morbidity (both in diabetic and non-diabetic patients). This study objective was to evaluate the profile and long-term prognosis of critically ill patients undergoing tight glucose-control. METHODS: Prospective cohort. All patients admitted to the intensive care unit over 1-year were enrolled. We analyzed demographic data, therapeutic intervention, and short- (during the stay) and long-term (2 years after discharge) mortality. The patients were categorized in 2 groups: tight glucose control and non-tight glucose-control, based on the unit staff decision. RESULTS: From the 603 enrolled patients, 102 (16.9%) underwent tight control (glucose <150 mg/dL) while 501 patients (83.1%) non-tight control. Patients in the TGC-group were more severely ill than those in the non-tight control group [APACHE II score (14 ± 3 versus 11 ± 4, P=0.04), SOFA (4.9 ± 3.2 versus 3.5 ± 3.4, P<0.001) and TISS-24h (25.7 ± 6.9 versus 21.1 ± 7.2, P< 0.001)]. The tight control group patients also had worse prognosis: [acute renal failure (51% versus 18.5%, P<0.001), critical illness neuropathy (16.7% versus 5.6%, P<0.001)] and increased mortality (during the ICU-stay [60.7% versus 17.7%, P<0.001] and within 2-years of the discharge [77.5% versus 23.4%; P<0.001]). CONCLUSION: Critically ill patients needing tight glucose control during the unit stay have more severe disease and have worse short and long-term prognosis.
Abstract
Rev Bras Ter Intensiva. 2006;18(3):268-275
DOI 10.1590/S0103-507X2006000300009
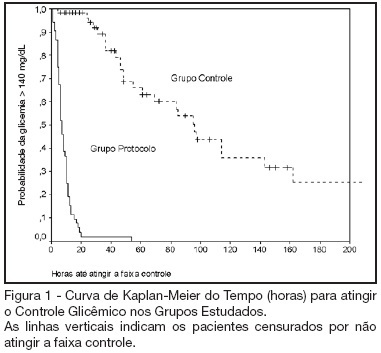
BACKGROUND AND OBJECTIVES: Actually tight glycemic control is a major concern in critical care. The objective of this study was to evaluate effectiveness and safety of Yale insulin infusion protocol in a Brazilian medical and surgical intensive care unit. METHODS: Retrospective, before-after cohort study. Selected end-points were mean blood glucose levels, time-to-reach target range of 80 - 140 mg/dL, and percent of blood glucose in target range and hypoglycemia incidence. RESULTS: Were studied 112 patients: 60 in control group (CG) and 52 in protocol group (PG). Bedside blood glucose was measured 5392 times for a mean value of 131.2 ± 14.7 mg/dL in the PG versus 2485 times for a mean value of 181.7 ± 36.1 mg/dL in the CG. Blood glucose values were in the target range 65% and 32% of the times, respectively for PG and CG groups (p < 0.001). The median time to reach glucose target range was 7 h (range 4 -10 h) for PG and 96 hr (range 46 - 278 h) for CG (p < 0.001). Incidence of severe hypoglycemia did not reach difference statistically significant: 4 patients in PG versus 2 patients in CG. CONCLUSIONS: Yale insulin infusion protocol was effective and safe to improve blood glucose control in a Brazilian medical and surgical intensive care unit.