You searched for:"Marina Verçoza Viana"
We found (3) results for your search.-
Original Article
Changes in cardiac arrest profiles after the implementation of a Rapid Response Team
Rev Bras Ter Intensiva. 2021;33(1):96-101
Abstract
Original ArticleChanges in cardiac arrest profiles after the implementation of a Rapid Response Team
Rev Bras Ter Intensiva. 2021;33(1):96-101
DOI 10.5935/0103-507X.20210010
Views1See moreABSTRACT
Objective:
To evaluate changes in the characteristics of in-hospital cardiac arrest after the implementation of a Rapid Response Team.
Methods:
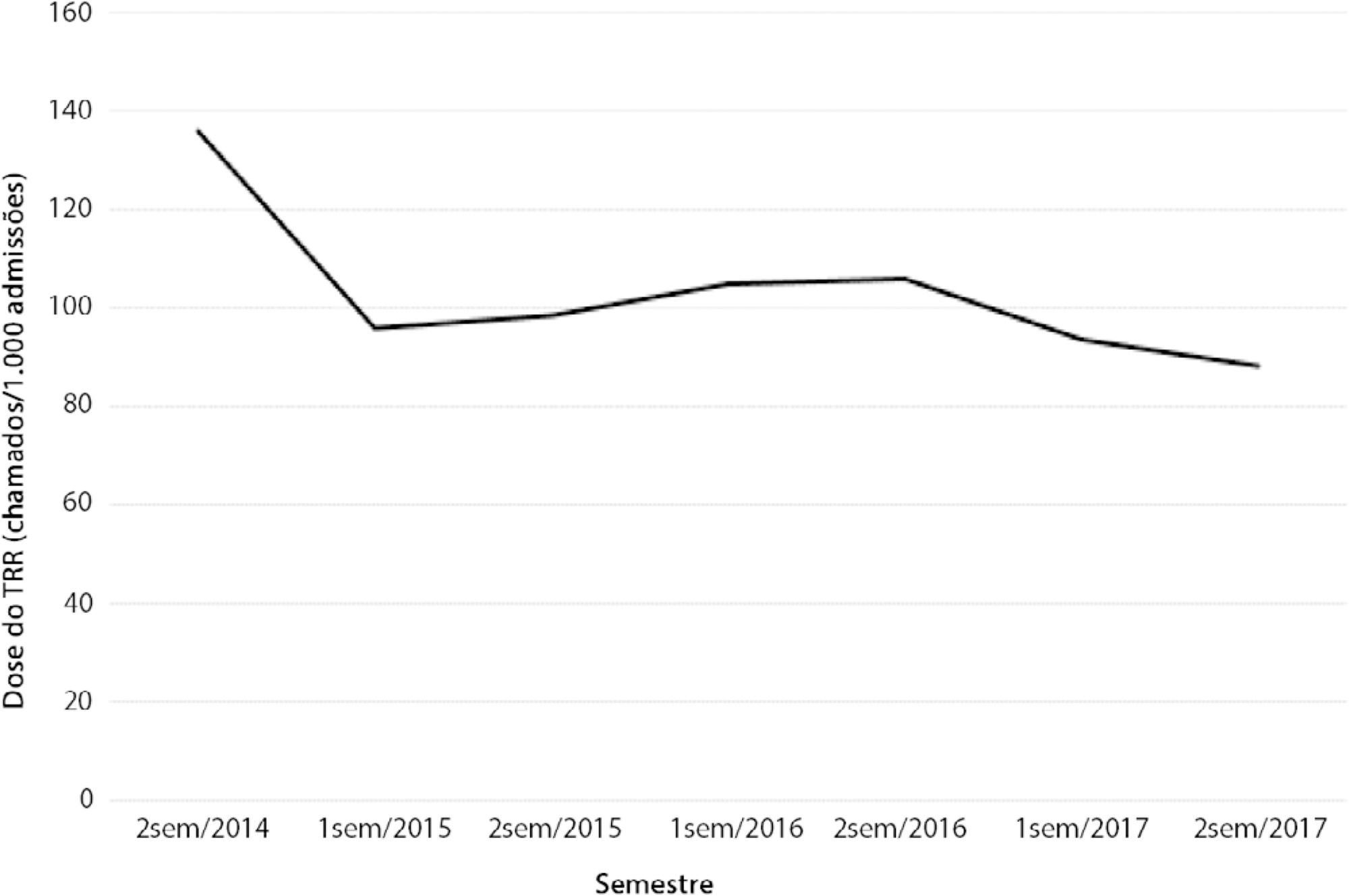
This was a prospective observational study of in-hospital cardiac arrest that occurred from January 2013 to December 2017. The exclusion criterion was in-hospital cardiac arrest in the intensive care unit, emergency room or operating room. The Rapid Response Team was implemented in July 2014 in the study hospital. Patients were classified into two groups: a Pre-Rapid Response Team (in-hospital cardiac arrest before Rapid Response Team implementation) and a Post-Rapid Response Team (in-hospital cardiac arrest after Rapid Response Team implementation). Patients were followed until hospital discharge or death.
Results:
We had a total of 308 cardiac arrests (64.6 ± 15.2 years, 60.3% men, 13.9% with initial shockable rhythm). There was a decrease from 4.2 to 2.5 in-hospital cardiac arrest/1000 admissions after implementation of the Rapid Response Team, and we had approximately 124 calls/1000 admissions. Pre-Rapid Response Team cardiac arrest was associated with more hypoxia (29.4 versus 14.3%; p = 0.006) and an altered respiratory rate (14.7 versus 4.2%; p = 0.004) compared with post-Rapid Response Team cardiac arrest. Cardiac arrest due to hypoxia was more common before Rapid Response Team implementation (61.2 versus 38.1%, p < 0.001). In multivariate analysis, return of spontaneous circulation was associated with shockable rhythm (OR 2.97; IC95% 1.04 - 8.43) and witnessed cardiac arrest (OR 2.52; IC95% 1.39 - 4.59) but not with Rapid Response Team implementation (OR 1.40; IC95% 0.70 - 2.81) or premonitory signs (OR 0.71; IC95% 0.39 - 1.28). In multivariate analysis, in-hospital mortality was associated with non-shockable rhythm (OR 5.34; IC95% 2.28 - 12.53) and age (OR 1.03; IC95% 1.01 - 1.05) but not with Rapid Response Team implementation (OR 0.89; IC95% 0.40 - 2.02).
Conclusion:
Even though Rapid Response Team implementation is associated with a reduction in in-hospital cardiac arrest, it was not associated with the mortality of in-hospital cardiac arrest victims. A significant decrease in cardiac arrests due to respiratory causes was noted after Rapid Response Team implementation.
-
Letters to the Editor
To: Therapeutic hypothermia after cardiac arrest: outcome predictors
Rev Bras Ter Intensiva. 2016;28(2):207-208
Abstract
Letters to the EditorTo: Therapeutic hypothermia after cardiac arrest: outcome predictors
Rev Bras Ter Intensiva. 2016;28(2):207-208
DOI 10.5935/0103-507X.20160038
Views0To the Editor, Determining the neurological prognosis of patients who have suffered cardiac arrest is extremely important because it allows the physician to inform the family about the life expectancy of their beloved relative, as well as to wisely plan for the allocation of available resources. We read with great interest the study performed by […]See more -
Review Article
Assessment and treatment of hyperglycemia in critically ill patients
Rev Bras Ter Intensiva. 2014;26(1):71-76
Abstract
Review ArticleAssessment and treatment of hyperglycemia in critically ill patients
Rev Bras Ter Intensiva. 2014;26(1):71-76
DOI 10.5935/0103-507X.20140011
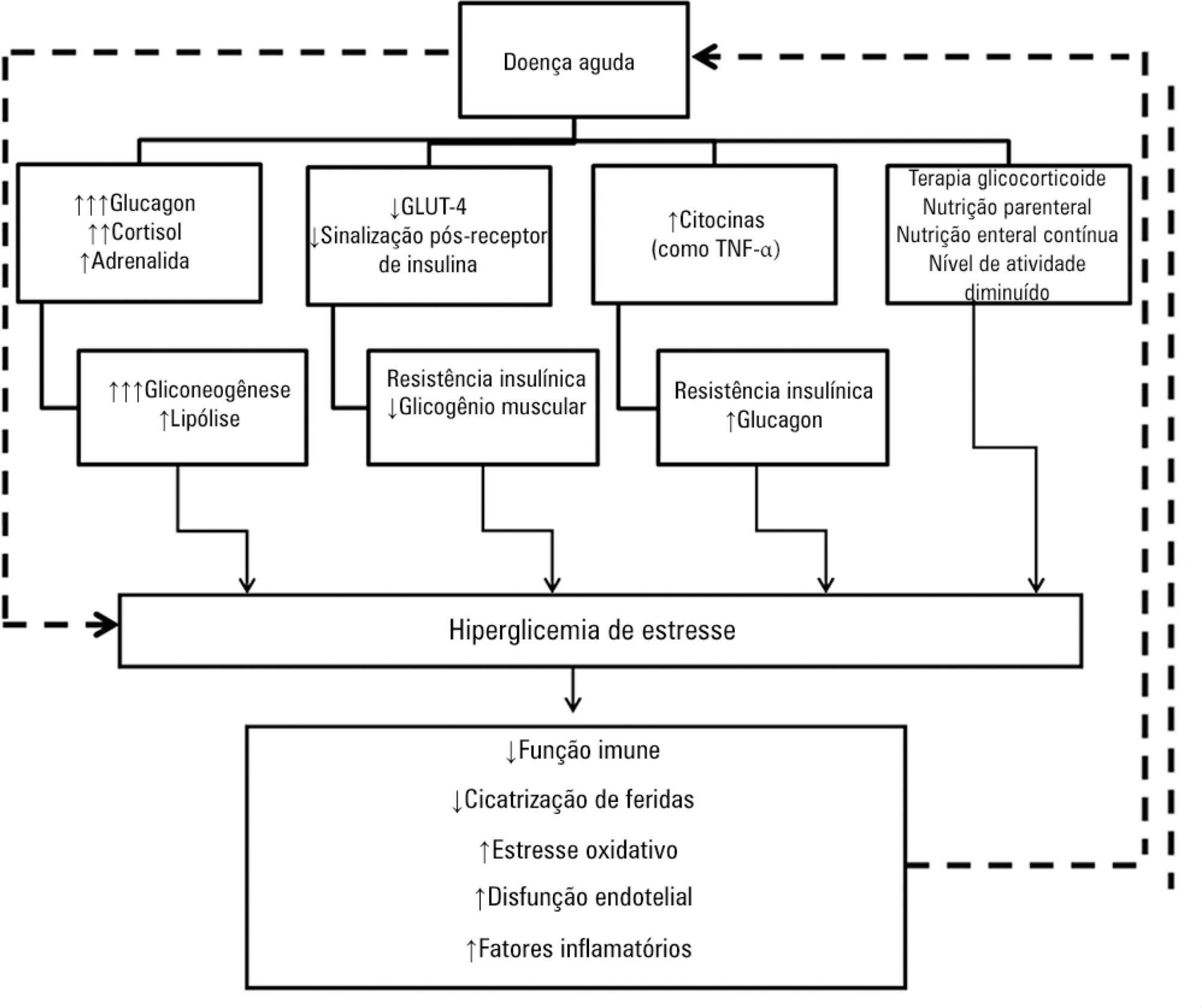
Views0See moreHyperglycemia is a commonly encountered issue in critically ill patients in the intensive care setting. The presence of hyperglycemia is associated with increased morbidity and mortality, regardless of the reason for admission (e.g., acute myocardial infarction, status post-cardiovascular surgery, stroke, sepsis). However, the pathophysiology and, in particular, the treatment of hyperglycemia in the critically ill patient remain controversial. In clinical practice, several aspects must be taken into account in the management of these patients, including blood glucose targets, history of diabetes mellitus, the route of nutrition (enteral or parenteral), and available monitoring equipment, which substantially increases the workload of providers involved in the patients’ care. This review describes the epidemiology, pathophysiology, management, and monitoring of hyperglycemia in the critically ill adult patient.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




