Abstract
Rev Bras Ter Intensiva. 2022;34(3):319-326
DOI 10.5935/0103-507X.20220101-en
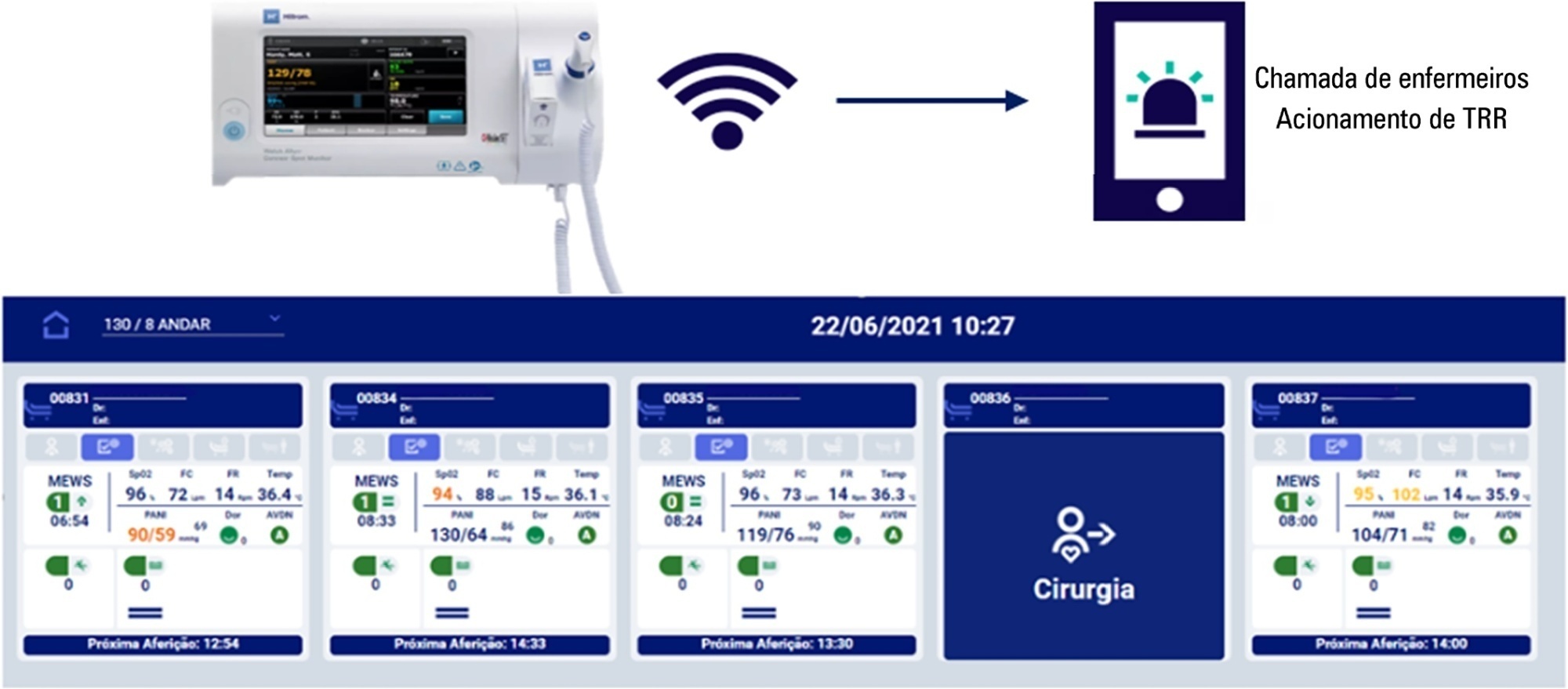
To evaluate the effectiveness of the Welch Allyn Connex® Spot Monitor/Hillrom Connecta™ solution in activating the rapid response team in a timely manner compared to manual activation.
The Hillrom study is a single-center, open-label, superiority, cluster-randomized, parallel-group (1:1 allocation ratio) clinical trial that will be conducted in a tertiary hospital. Two sets of three wards with 28 beds will be included (one as the intervention cluster and the other as the control). The wards will be randomly assigned to use the Welch Allyn Connex® Spot Monitor/Hillrom Connecta™ automated solution (intervention cluster) or to maintain the usual routine (control cluster) regarding rapid response team activation. The primary outcome will be the absolute number of episodes of rapid response team triggering in an appropriate time; as secondary outcomes, clinical features (mortality, cardiac arrest, need for intensive care unit admission and duration of hospitalization) will be assessed according to clusters in an exploratory way. A sample size of 216 rapid response team activations was estimated to identify a possible difference between the groups. The protocol has been approved by the institutional Research Ethics Committee.
The Welch Allyn Connex® Spot Monitor/Hillrom Connecta™ automated solution is expected to be more effective in triggering the nurse call system to activate the rapid response team in a timely and adequate manner compared to manual triggering (usual practice).
NCT04648579
Abstract
Rev Bras Ter Intensiva. 2021;33(1):96-101
DOI 10.5935/0103-507X.20210010
To evaluate changes in the characteristics of in-hospital cardiac arrest after the implementation of a Rapid Response Team.
This was a prospective observational study of in-hospital cardiac arrest that occurred from January 2013 to December 2017. The exclusion criterion was in-hospital cardiac arrest in the intensive care unit, emergency room or operating room. The Rapid Response Team was implemented in July 2014 in the study hospital. Patients were classified into two groups: a Pre-Rapid Response Team (in-hospital cardiac arrest before Rapid Response Team implementation) and a Post-Rapid Response Team (in-hospital cardiac arrest after Rapid Response Team implementation). Patients were followed until hospital discharge or death.
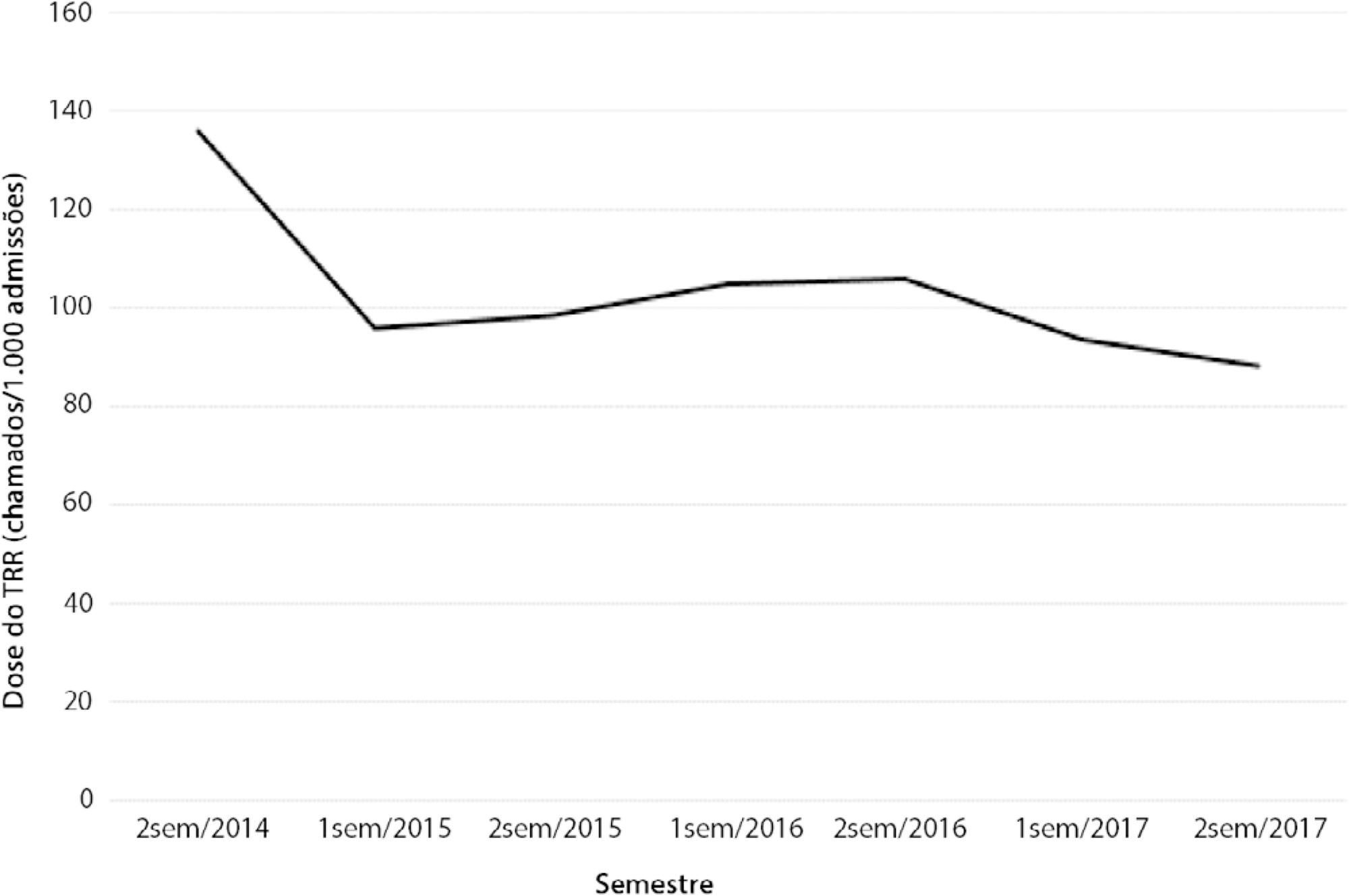
We had a total of 308 cardiac arrests (64.6 ± 15.2 years, 60.3% men, 13.9% with initial shockable rhythm). There was a decrease from 4.2 to 2.5 in-hospital cardiac arrest/1000 admissions after implementation of the Rapid Response Team, and we had approximately 124 calls/1000 admissions. Pre-Rapid Response Team cardiac arrest was associated with more hypoxia (29.4 versus 14.3%; p = 0.006) and an altered respiratory rate (14.7 versus 4.2%; p = 0.004) compared with post-Rapid Response Team cardiac arrest. Cardiac arrest due to hypoxia was more common before Rapid Response Team implementation (61.2 versus 38.1%, p < 0.001). In multivariate analysis, return of spontaneous circulation was associated with shockable rhythm (OR 2.97; IC95% 1.04 - 8.43) and witnessed cardiac arrest (OR 2.52; IC95% 1.39 - 4.59) but not with Rapid Response Team implementation (OR 1.40; IC95% 0.70 - 2.81) or premonitory signs (OR 0.71; IC95% 0.39 - 1.28). In multivariate analysis, in-hospital mortality was associated with non-shockable rhythm (OR 5.34; IC95% 2.28 - 12.53) and age (OR 1.03; IC95% 1.01 - 1.05) but not with Rapid Response Team implementation (OR 0.89; IC95% 0.40 - 2.02).
Even though Rapid Response Team implementation is associated with a reduction in in-hospital cardiac arrest, it was not associated with the mortality of in-hospital cardiac arrest victims. A significant decrease in cardiac arrests due to respiratory causes was noted after Rapid Response Team implementation.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):217-226
DOI 10.5935/0103-507X.20190036
To describe the implementation of a rapid response team in a large nonprofit hospital, indicating relevant issues for other initiatives in similar contexts, particularly in Latin America.
In general terms, the intervention consisted of three major components: (1) a tool to detect aggravation of clinical conditions in general wards; (2) the structuring of a rapid response team to attend to all patients at risk; and (3) the monitoring of indicators regarding the intervention. This work employed four half-year Plan-Do-Study-Act cycles to test and adjust the intervention from January 2013 to December 2014.
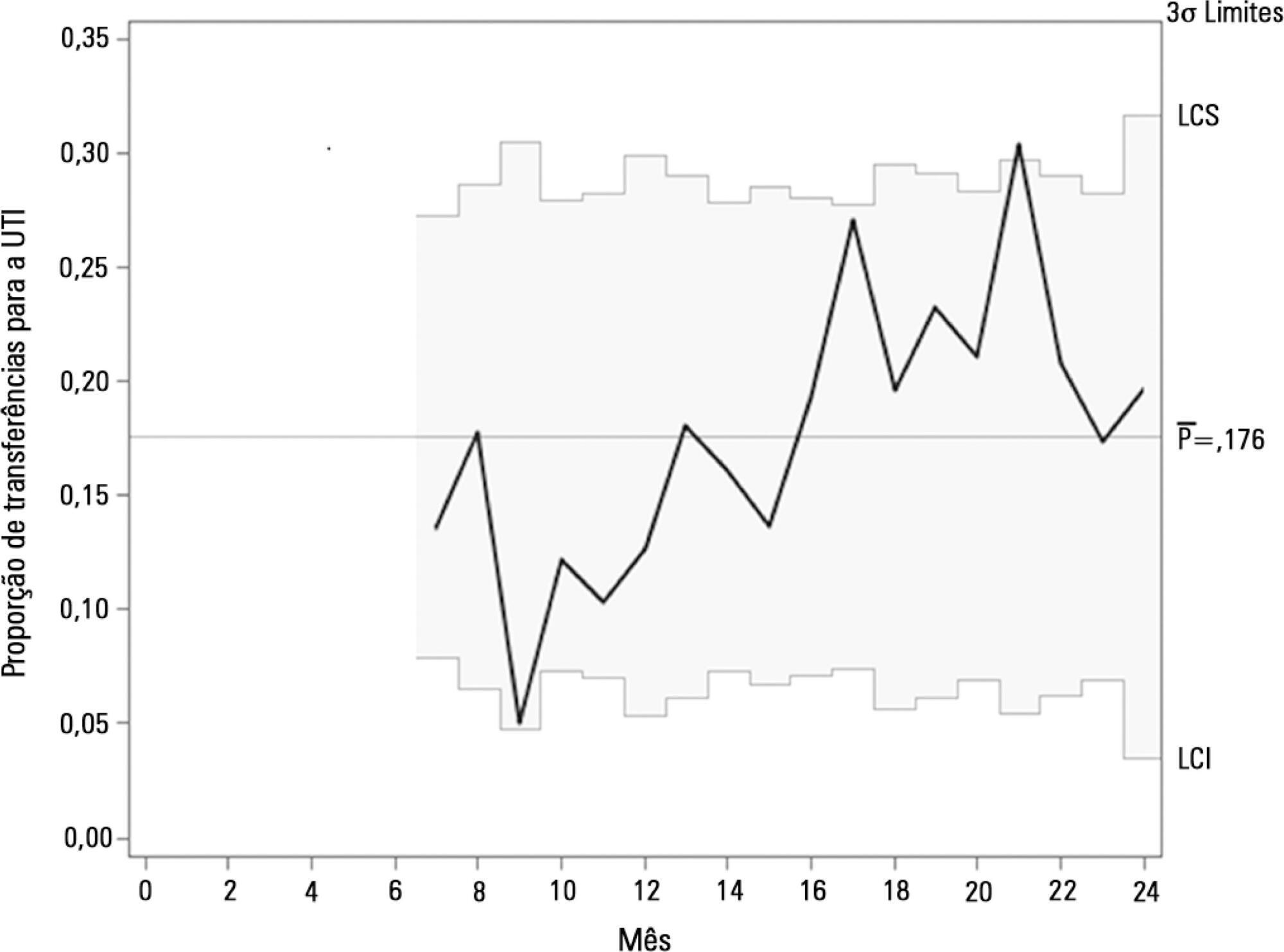
Between 2013 and 2014, the rapid response team attended to 2,296 patients. This study showed a nonsignificant reduction in mortality from 8.3% in cycle 1 to 5.0% in cycle 4; however, death rates remained stable in cycles 3 and 4, with frequencies of 5.2% and 5.0%, respectively. Regarding patient flow and continuum of critical care, which is a premise of the rapid response system, there was a reduction in waiting time for intensive care unit beds with a decrease from 45.9% to 19.0% in the frequency of inpatients who could not be admitted immediately after indication (p < 0.001), representing improved patient flow in the hospital. In addition, an increase in the recognition of palliative care patients from 2.8% to 10.3% was noted (p = 0.005).
Implementing a rapid response team in contexts where there are structural restrictions, such as lack of intensive care unit beds, may be very beneficial, but a strategy of adjustment is needed.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):278-284
DOI 10.5935/0103-507X.20160045
To evaluate the implementation of a multidisciplinary rapid response team led by an intensive care physician at a university hospital.
This retrospective cohort study analyzed assessment forms that were completed during the assessments made by the rapid response team of a university hospital between March 2009 and February 2014.
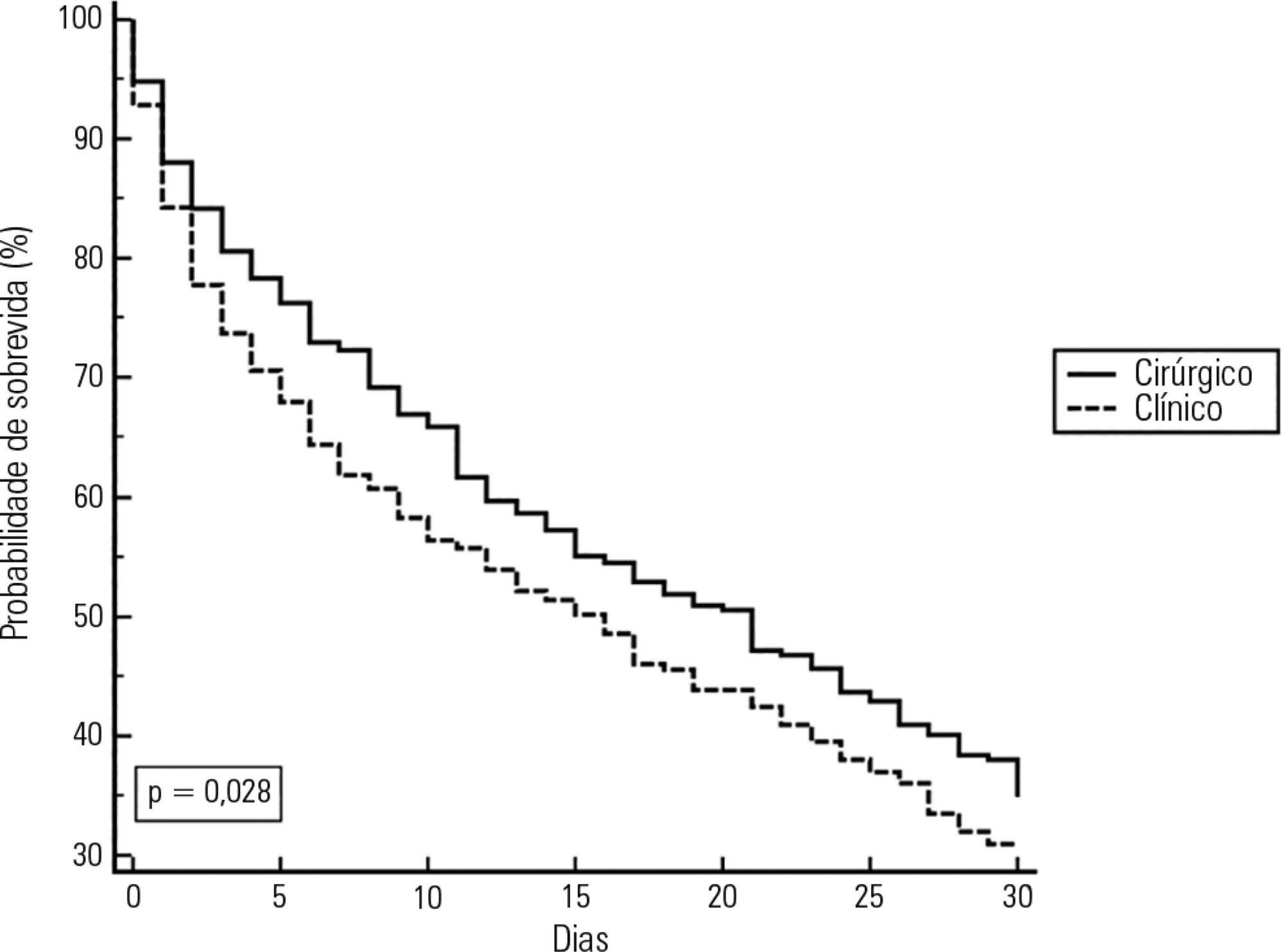
Data were collected from 1,628 assessments performed by the rapid response team for 1,024 patients and included 1,423 code yellow events and 205 code blue events. The number of assessments was higher in the first year of operation of the rapid response team. The multivariate analysis indicated that age (OR 1.02; 95%CI 1.02 - 1.03; p < 0.001), being male (OR 1.48; 95%CI 1.09 - 2.01; p = 0.01), having more than one assessment (OR 3.31; 95%CI, 2.32 - 4.71; p < 0.001), hospitalization for clinical care (OR 1.77; 95%CI 1.29 - 2.42; p < 0.001), the request of admission to the intensive care unit after the code event (OR 4.75; 95%CI 3.43 - 6.59; p < 0.001), and admission to the intensive care unit before the code event (OR 2.13; 95%CI 1.41 - 3.21; p = 0.001) were risk factors for hospital mortality in patients who were seen for code yellow events.
The hospital mortality rates were higher than those found in previous studies. The number of assessments was higher in the first year of operation of the rapid response team. Moreover, hospital mortality was higher among patients admitted for clinical care.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):420-426
DOI 10.5935/0103-507X.20160075
To determine the incidence of afferent limb failure of the in-hospital Medical Emergency Team, characterizing it and comparing the mortality between the population experiencing afferent limb failure and the population not experiencing afferent limb failure.
A total of 478 activations of the Medical Emergency Team of Hospital Pedro Hispano occurred from January 2013 to July 2015. A sample of 285 activations was obtained after excluding incomplete records and activations for patients with less than 6 hours of hospitalization. The sample was divided into two groups: the group experiencing afferent limb failure and the group not experiencing afferent limb failure of the Medical Emergency Team. Both populations were characterized and compared. Statistical significance was set at p ≤ 0.05.
Afferent limb failure was observed in 22.1% of activations. The causal analysis revealed significant differences in Medical Emergency Team activation criteria (p = 0.003) in the group experiencing afferent limb failure, with higher rates of Medical Emergency Team activation for cardiac arrest and cardiovascular dysfunction. Regarding patient outcomes, the group experiencing afferent limb failure had higher immediate mortality rates and higher mortality rates at hospital discharge, with no significant differences. No significant differences were found for the other parameters.
The incidence of cardiac arrest and the mortality rate were higher in patients experiencing failure of the afferent limb of the Medical Emergency Team. This study highlights the need for health units to invest in the training of all healthcare professionals regarding the Medical Emergency Team activation criteria and emergency medical response system operations.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):99-105
DOI 10.5935/0103-507X.20130020
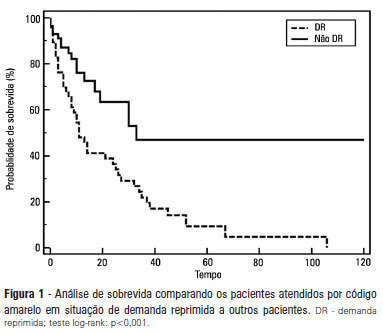
OBJECTIVE: To describe the epidemiological data of the clinical instability events in patients attended to by the rapid response team and to identify prognostic factors. METHODS: This was a longitudinal study, performed from January to July 2010, with an adult inpatient population in a hospital environment. The data collected regarding the code yellow service included the criteria of the clinical instability, the drug and non-drug therapies administered and the activities and procedures performed. The outcomes evaluated were the need for intensive care unit admission and the hospital mortality rates. A level of p=0.05 was considered to be significant. RESULTS: A total of 150 code yellow events that occurred in 104 patients were evaluated. The most common causes were related to acute respiratory insufficiency with hypoxia or a change in the respiratory rate and a concern of the team about the patient's clinical condition. It was necessary to request a transfer to the intensive care unit in 80 of the 150 cases (53.3%). It was necessary to perform 42 procedures. The most frequent procedures were orotracheal intubation and the insertion of a central venous catheter. The patients who were in critical condition and had to wait for an intensive care unit bed had a higher risk of death compared to the other patients (hazard ratio: 3.12; 95% CI: 1.80-5.40; p<0.001). CONCLUSIONS: There are patients in critical condition that require expert intensive care in the regular ward unit hospital beds. The events that most frequently led to the code yellow activation were related to hemodynamic and respiratory support. The interventions performed indicate the need for a physician on the team. The situation of pent-up demand is associated with a higher mortality rate.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)