You searched for:"Janete Salles Brauner"
We found (3) results for your search.-
Original Article
Changes in cardiac arrest profiles after the implementation of a Rapid Response Team
Rev Bras Ter Intensiva. 2021;33(1):96-101
Abstract
Original ArticleChanges in cardiac arrest profiles after the implementation of a Rapid Response Team
Rev Bras Ter Intensiva. 2021;33(1):96-101
DOI 10.5935/0103-507X.20210010
Views1See moreABSTRACT
Objective:
To evaluate changes in the characteristics of in-hospital cardiac arrest after the implementation of a Rapid Response Team.
Methods:
This was a prospective observational study of in-hospital cardiac arrest that occurred from January 2013 to December 2017. The exclusion criterion was in-hospital cardiac arrest in the intensive care unit, emergency room or operating room. The Rapid Response Team was implemented in July 2014 in the study hospital. Patients were classified into two groups: a Pre-Rapid Response Team (in-hospital cardiac arrest before Rapid Response Team implementation) and a Post-Rapid Response Team (in-hospital cardiac arrest after Rapid Response Team implementation). Patients were followed until hospital discharge or death.
Results:
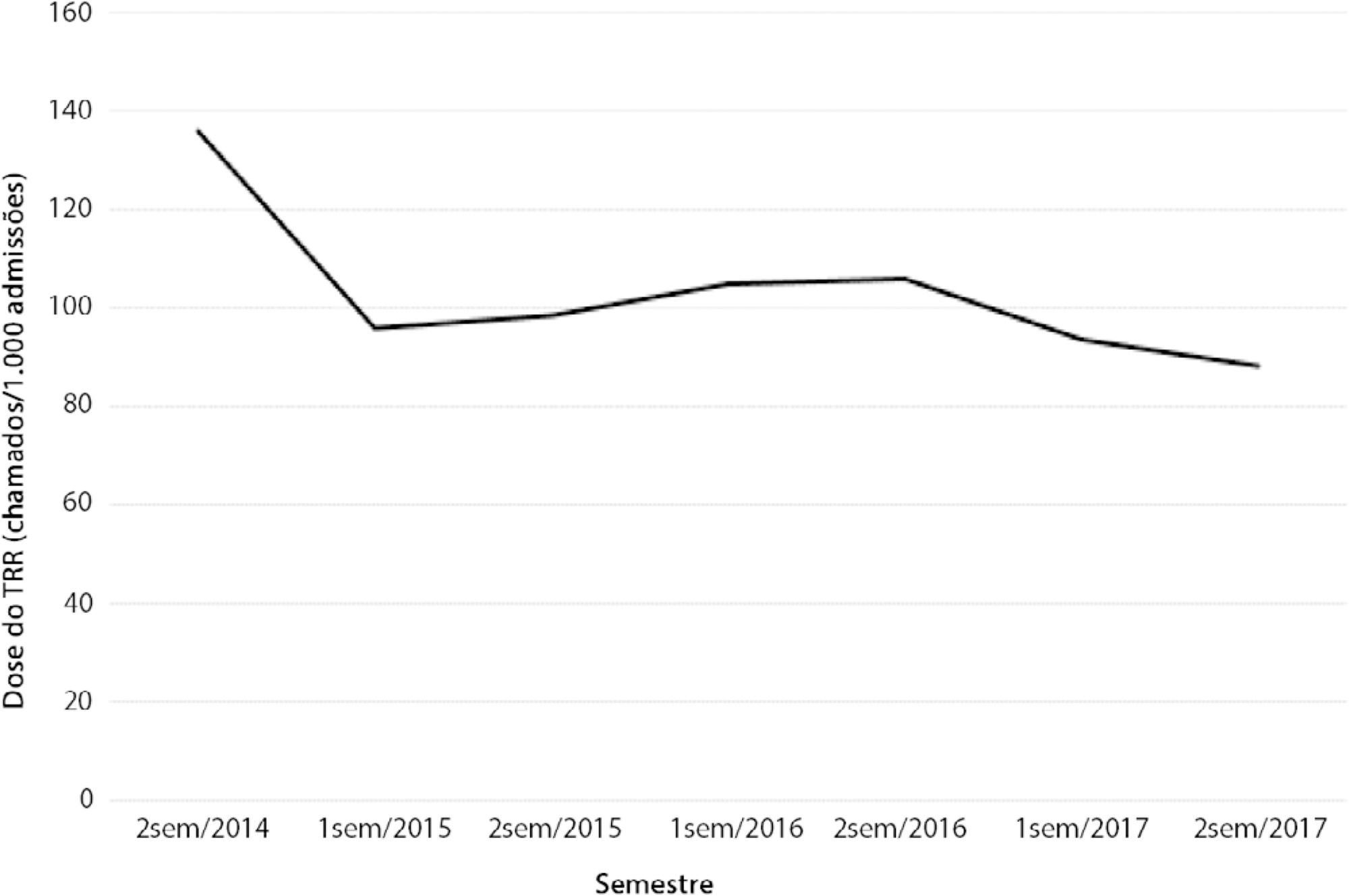
We had a total of 308 cardiac arrests (64.6 ± 15.2 years, 60.3% men, 13.9% with initial shockable rhythm). There was a decrease from 4.2 to 2.5 in-hospital cardiac arrest/1000 admissions after implementation of the Rapid Response Team, and we had approximately 124 calls/1000 admissions. Pre-Rapid Response Team cardiac arrest was associated with more hypoxia (29.4 versus 14.3%; p = 0.006) and an altered respiratory rate (14.7 versus 4.2%; p = 0.004) compared with post-Rapid Response Team cardiac arrest. Cardiac arrest due to hypoxia was more common before Rapid Response Team implementation (61.2 versus 38.1%, p < 0.001). In multivariate analysis, return of spontaneous circulation was associated with shockable rhythm (OR 2.97; IC95% 1.04 - 8.43) and witnessed cardiac arrest (OR 2.52; IC95% 1.39 - 4.59) but not with Rapid Response Team implementation (OR 1.40; IC95% 0.70 - 2.81) or premonitory signs (OR 0.71; IC95% 0.39 - 1.28). In multivariate analysis, in-hospital mortality was associated with non-shockable rhythm (OR 5.34; IC95% 2.28 - 12.53) and age (OR 1.03; IC95% 1.01 - 1.05) but not with Rapid Response Team implementation (OR 0.89; IC95% 0.40 - 2.02).
Conclusion:
Even though Rapid Response Team implementation is associated with a reduction in in-hospital cardiac arrest, it was not associated with the mortality of in-hospital cardiac arrest victims. A significant decrease in cardiac arrests due to respiratory causes was noted after Rapid Response Team implementation.
-
Special Articles
Guidelines for the management of accidental tetanus in adult patients
Rev Bras Ter Intensiva. 2011;23(4):394-409
Abstract
Special ArticlesGuidelines for the management of accidental tetanus in adult patients
Rev Bras Ter Intensiva. 2011;23(4):394-409
DOI 10.1590/S0103-507X2011000400004
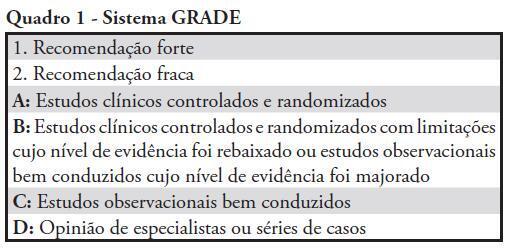
Views0See moreAlthough tetanus can be prevented by appropriate immunization, accidental tetanus continues to occur frequently in underdeveloped and developing countries. Tetanus mortality rates remain high in these areas, and studies regarding the best therapy for tetanus are scarce. Because of the paucity of data on accidental tetanus and the clinical relevance of this condition, the Associação de Medicina Intensiva Brasileira (AMIB) organized a group of experts to develop these guidelines, which are based on the best available evidence for the management of tetanus in patients requiring admission to the intensive care unit. The guidelines discuss the management of tetanus patients in the intensive care unit, including the use of immunoglobulin therapy, antibiotic therapy, management of analgesics, sedation and neuromuscular blockade, management of dysautonomia and specific issues related to mechanical ventilation and physiotherapy in this population.
-
Artigos de Revisão
Serum neuron-specific enolase as a prognostic marker after a cardiac arrest
Rev Bras Ter Intensiva. 2006;18(4):396-401
Abstract
Artigos de RevisãoSerum neuron-specific enolase as a prognostic marker after a cardiac arrest
Rev Bras Ter Intensiva. 2006;18(4):396-401
DOI 10.1590/S0103-507X2006000400013
Views0See moreBACKGROUND AND OBJECTIVES: Cardiac arrest is a state of severe cerebral perfusion deficit. Patients recovering from a cardiopulmonary resuscitation are at great risk of subsequent death or incapacitating neurologic injury, including persistent vegetative state. The early definition of prognosis for these patients has ethical and economic implications. The main purpose of this manuscript was to review the prognostic value of serum Neuron-Specific Enolase (NSE) in predicting outcomes in patients early after a cardiac arrest. CONTENTS: Severe neurologic disability is the most feared complication after a cardiac arrest. Many studies are trying to find prognostic markers that can be associated with outcomes in patients surviving a cardiac arrest. Biochemical markers of neuronal injury seem to be promising in this scenario. Therefore, NSE levels have been studied in patients after a cardiac arrest and high enzyme levels suggest more extensive brain damage and are associated with unfavorable clinical outcomes. CONCLUSIONS: Outcome after a cardiac arrest is mostly determined by the degree of hypoxic brain damage and early determinations of serum NSE level can be a valuable ancillary method for assessing outcome in these patients.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




