Abstract
Rev Bras Ter Intensiva. 2022;34(4):524-528
DOI 10.5935/0103-507X.20220342-en
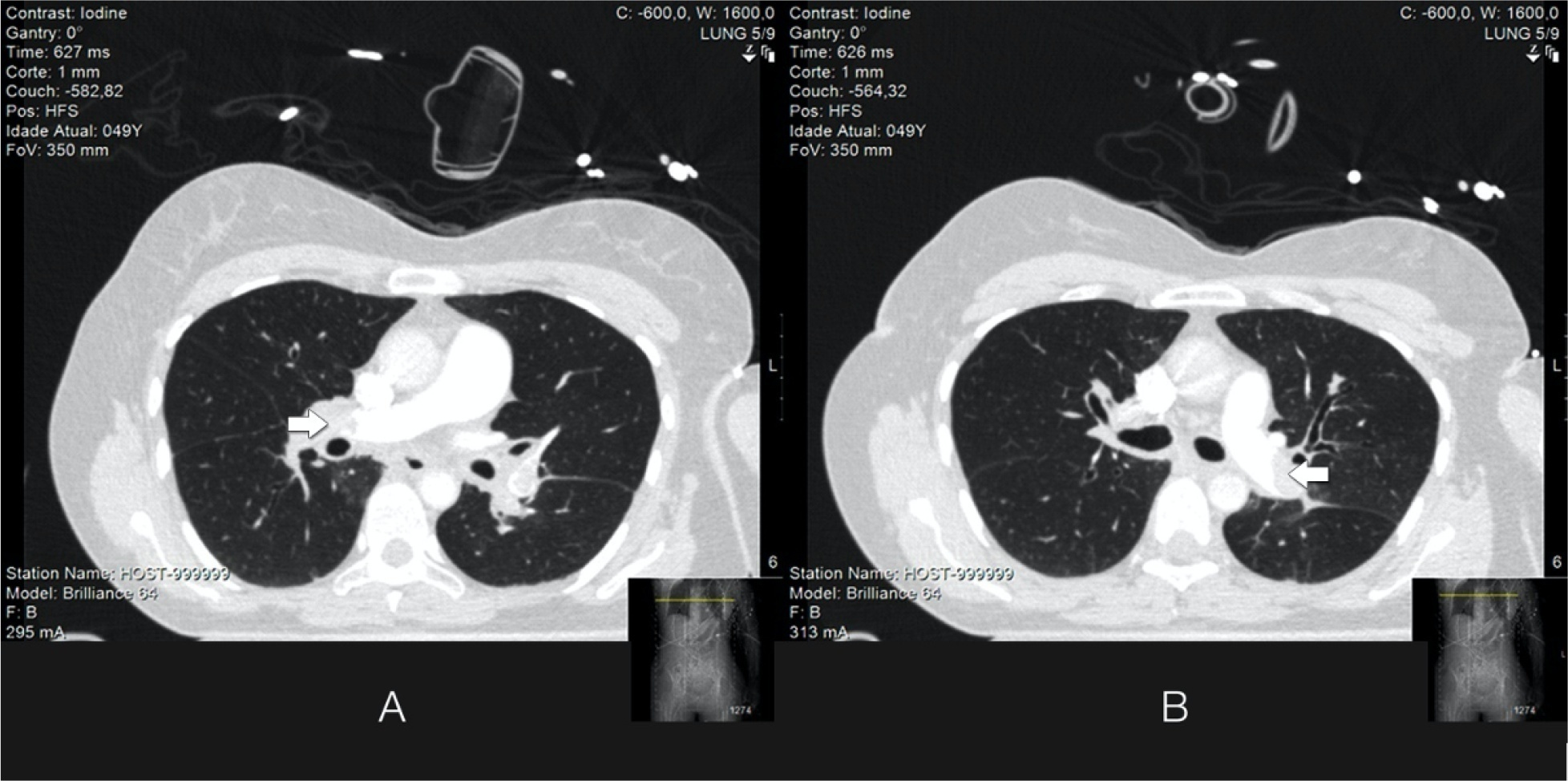
Acute massive pulmonary embolism is the most serious presentation of venous thromboembolism that can ultimately cause obstructive shock, leading to cardiac arrest and death. In this case report, the authors present a case of a 49-year-old female who successfully recovered from a massive pulmonary embolism with the combined use of venoarterial extracorporeal membrane oxygenation and pulmonary aspiration thrombectomy, with no complications from these procedures. Although evidence of benefit from mechanical support has not been established for patients with massive pulmonary embolism, the implementation of extracorporeal cardiocirculatory support during resuscitation may allow improvement of systemic organ perfusion and better chance of survival. Recent guidelines from the European Society of Cardiology state that venoarterial extracorporeal membrane oxygenation in combination with catheter-directed treatment may be considered for patients presenting with massive pulmonary embolism and refractory cardiac arrest. The use of extracorporeal membrane oxygenation as a stand-alone technique with anticoagulation remains controversial, and additional therapies, such as surgical or percutaneous embolectomy, must be considered. Since this intervention is not supported by high-quality studies, we believe it is important to report real-world successful cases. With this case report, we illustrate the benefit derived from resuscitation assisted by extracorporeal mechanical support and early aspiration thrombectomy in patients with massive pulmonary embolism. Additionally, it emphasizes the synergy that derives from integrated multidisciplinary systems for providing complex interventions, of which extracorporeal membrane oxygenation and Interventional Cardiology are clear examples.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):251-260
DOI 10.5935/0103-507X.20210032
To identify predictors of coronary artery disease in survivors of cardiac arrest, to define the best timing for coronary angiography and to establish the relationship between coronary artery disease and mortality.
This was a single-center retrospective study including consecutive patients who underwent coronary angiography after cardiac arrest.
A total of 117 patients (63 ± 13 years, 77% men) were included. Most cardiac arrest incidents occurred with shockable rhythms (70.1%), and the median duration until the return of spontaneous circulation was 10 minutes. Significant coronary artery disease was found in 68.4% of patients, of whom 75% underwent percutaneous coronary intervention. ST-segment elevation (OR 6.5, 95%CI 2.2 - 19.6; p = 0.001), the presence of wall motion abnormalities (OR 22.0, 95%CI 5.7 - 84.6; p < 0.001), an left ventricular ejection fraction ≤ 40% (OR 6.2, 95%CI 1.8 - 21.8; p = 0.005) and elevated high sensitivity troponin T (OR 3.04, 95%CI 1.3 - 6.9; p = 0.008) were predictors of coronary artery disease; the latter had poor accuracy (area under the curve 0.64; p = 0.004), with an optimal cutoff of 170ng/L. Only ST-segment elevation and the presence of wall motion abnormalities were independent predictors of coronary artery disease. The duration of cardiac arrest (OR 1.015, 95%CI 1.0 - 1.05; p = 0.048) was an independent predictor of death, and shockable rhythm (OR 0.4, 95%CI 0.4 - 0.9; p = 0.031) was an independent predictor of survival. The presence of coronary artery disease and the performance of percutaneous coronary intervention had no impact on survival; it was not possible to establish the best cutoff for coronary angiography timing.
In patients with cardiac arrest, ST-segment elevation, wall motion abnormalities, left ventricular dysfunction and elevated high sensitivity troponin T were predictive of coronary artery disease. Neither coronary artery disease nor percutaneous coronary intervention significantly impacted survival.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):405-412
DOI 10.5935/0103-507X.20160065
To compare patients without previously diagnosed cardiovascular risk factors) and patients with one or more risk factors admitted with acute coronary syndrome.
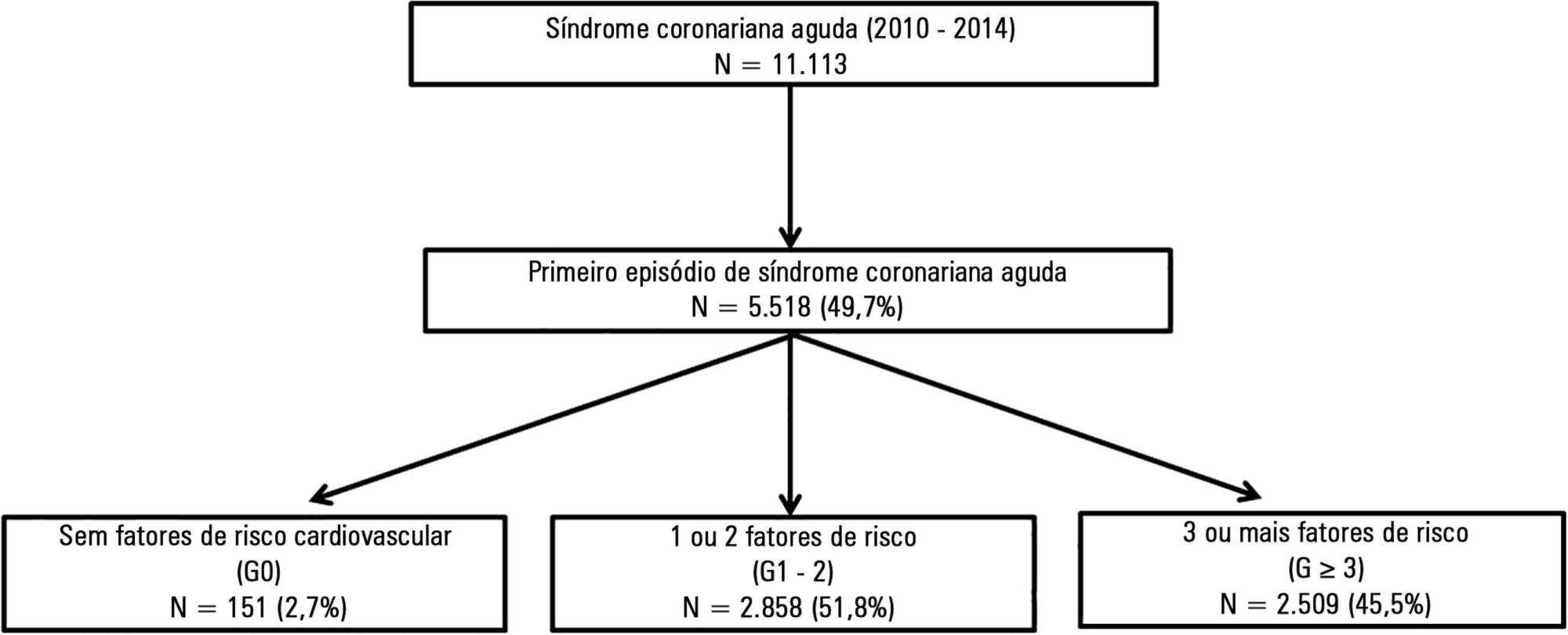
This was a retrospective analysis of patients admitted with first episode of acute coronary syndrome without previous heart disease, who were included in a national acute coronary syndrome registry. The patients were divided according to the number of risk factors, as follows: 0 risk factor (G0), 1 or 2 risk factors (G1 - 2) and 3 or more risk factors (G ≥ 3). Comparative analysis was performed between the three groups, and independent predictors of cardiac arrest and death were studied.
A total of 5,518 patients were studied, of which 72.2% were male and the mean age was 64 ± 14 years. G0 had a greater incidence of ST-segment elevation myocardial infarction, with the left anterior descending artery being the most frequently involved vessel, and a lower prevalence of multivessel disease. Even though G0 had a lower Killip class (96% in Killip I; p < 0.001) and higher ejection fraction (G0 56 ± 10% versus G1 - 2 and G ≥ 3 53 ± 12%; p = 0.024) on admission, there was a significant higher incidence of cardiac arrest. Multivariate analysis identified the absence of risk factors as an independent predictor of cardiac arrest (OR 2.78; p = 0.019). Hospital mortality was slightly higher in G0, although this difference was not significant. By Cox regression analysis, the number of risk factors was found not to be associated with mortality. Predictors of death at 1 year follow up included age (OR 1.05; p < 0.001), ST-segment elevation myocardial infarction (OR 1.94; p = 0.003) and ejection fraction < 50% (OR 2.34; p < 0.001).
Even though the group without risk factors was composed of younger patients with fewer comorbidities, better left ventricular function and less extensive coronary disease, the absence of risk factors was an independent predictor of cardiac arrest.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):190-196
DOI 10.1590/S0103-507X2008000200013
BACKGROUND AND OBJECTIVES: Out-of-hospital cardiac arrest is a major cause of death with survival rates as low as 5% to 35%. A large number of patients who survive resuscitation will face significant neurological damage, as a result of the ischemia that occurs both during cardiac arrest and reperfusion. However understanding of the mechanisms responsible for brain damage has not resulted in prognostic improvement. Therapeutic hypothermia after resuscitation may be a valid option associated to reduction of neurological damage. The purpose of this study was to review scientific evidence related to a therapy for patients resuscitated from cardiac arrest. CONTENTS: Description and analysis of the main risk factors associated with neurological damage after resuscitation from cardiac arrest as well as prognostic criteria was carried out. A non-systematic search was conducted in the PubMed data base for papers on a therapeutic approach for patients resuscitated from cardiac arrest. Bibliographic references of reviewed papers were also analyzed. Practical rules were drafted for such an approach. CONCLUSIONS: Patients resuscitated from cardiac arrest face a high level of risk of neurological damage. Therapeutic hypothermia and control of physiological parameters to optimise brain perfusion, may improve prognosis.
Abstract
Rev Bras Ter Intensiva. 2006;18(2):177-185
DOI 10.1590/S0103-507X2006000200011
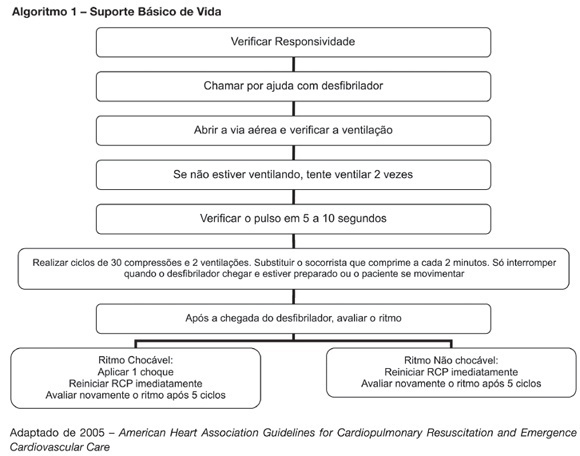
BACKGROUND AND OBJECTIVES: New resuscitation guidelines contain significant changes intended to improve resuscitation practice and survival from cardiac arrest. This article provides an overview of the key changes on resuscitation for healthcare provider. CONTENTS: There are several new recommendations on cardiopulmonary resuscitation (CPR), the major are intended to provide good circulation during cardiac arrest. The most important change is the emphasis on high-quality chest compressions with minimal interruptions. The universal 30:2 ratio is recommended to simplify training, to achieve optimal compression rates and to reduce the frequency of interruptions. Only one shock is delivered when indicated, followed immediately by CPR. This shock should be of 120-200J on a biphasic wave or 360J on a monophasic wave. Rescuers should not interrupt chest compressions to check rhythm until after about 5 cycles or approximately 2 minutes of CPR. After this period, if an organized rhythm is present, the healthcare provider should check for a pulse. There are several little changes about the drugs administrated during CPR according to the rhythm. Given the lack of documented effect of drug therapy in improving long-term outcome from cardiac arrest, the sequence for CPR deemphasizes drug administration and reemphasizes basic life support. CONCLUSIONS: The update on the new resuscitation guidelines is important to improve the quality of resuscitation and achieve better survival rates from our critical care patients.
Abstract
Rev Bras Ter Intensiva. 2006;18(4):374-379
DOI 10.1590/S0103-507X2006000400009
BACKGROUND AND OBJECTIVES: New resuscitation guidelines contain significant changes intended to improve resuscitation practice and survival from cardiac arrest. The objective of this study was to evaluate the theoretical knowledge about cardiac arrest (CA) and cardiac and pulmonary resuscitation (CPR) among doctors after five years of the graduation. METHODS: The questionnaire survey was conducted in an Emergency Hospital in the State of Alagoas. The population was composed of doctors with five years after your graduation. The data was collected with a questionnaire with questions about the theme. The results were analyzed based on bibliographies about CA and CPR. RESULTS: Thirty-nine professionals answered the questionnaire. The CA diagnostic was correct in 76.9% and increased to 82.7 when the case report was included. Questions about sodium bicarbonate and vasopressin were correctly answered by 30.8% and 15.4% of the participants. CONCLUSIONS: The greatest difficulty reported in this study was on the CA arrest Most of the participants of the survey are not aware of the correct indications of vasopressin and sodium bicarbonate in the CPR. According to this study, a continuing medical education program on CPR for physicians with more than five years of graduations warranted.
Abstract
Rev Bras Ter Intensiva. 2006;18(4):396-401
DOI 10.1590/S0103-507X2006000400013
BACKGROUND AND OBJECTIVES: Cardiac arrest is a state of severe cerebral perfusion deficit. Patients recovering from a cardiopulmonary resuscitation are at great risk of subsequent death or incapacitating neurologic injury, including persistent vegetative state. The early definition of prognosis for these patients has ethical and economic implications. The main purpose of this manuscript was to review the prognostic value of serum Neuron-Specific Enolase (NSE) in predicting outcomes in patients early after a cardiac arrest. CONTENTS: Severe neurologic disability is the most feared complication after a cardiac arrest. Many studies are trying to find prognostic markers that can be associated with outcomes in patients surviving a cardiac arrest. Biochemical markers of neuronal injury seem to be promising in this scenario. Therefore, NSE levels have been studied in patients after a cardiac arrest and high enzyme levels suggest more extensive brain damage and are associated with unfavorable clinical outcomes. CONCLUSIONS: Outcome after a cardiac arrest is mostly determined by the degree of hypoxic brain damage and early determinations of serum NSE level can be a valuable ancillary method for assessing outcome in these patients.