Abstract
Rev Bras Ter Intensiva. 2019;31(3):386-392
DOI 10.5935/0103-507X.20190051
The improvement in cardiopulmonary resuscitation quality has reduced the mortality of individuals treated for cardiac arrest. However, survivors have a high risk of severe brain damage in cases of return of spontaneous circulation. Data suggest that cases of cardiac arrest in critically ill patients with non-shockable rhythms have only a 6% chance of returning of spontaneous circulation, and of these, only one-third recover their autonomy. Should we, therefore, opt for a procedure in which the chance of survival is minimal and the risk of hospital death or severe and definitive brain damage is approximately 70%? Is it worth discussing patient resuscitation in cases of cardiac arrest? Would this discussion bring any benefit to the patients and their family members? Advanced discussions on do-not-resuscitate are based on the ethical principle of respect for patient autonomy, as the wishes of family members and physicians often do not match those of patients. In addition to the issue of autonomy, advanced discussions can help the medical and care team anticipate future problems and, thus, better plan patient care. Our opinion is that discussions regarding the resuscitation of critically ill patients should be performed for all patients within the first 24 to 48 hours after admission to the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):427-435
DOI 10.5935/0103-507X.20160076
The objective of this study was to analyze the clinical profile of patients with in-hospital cardiac arrest using the Utstein style.
This study is an observational, prospective, longitudinal study of patients with cardiac arrest treated in intensive care units over a period of 1 year.
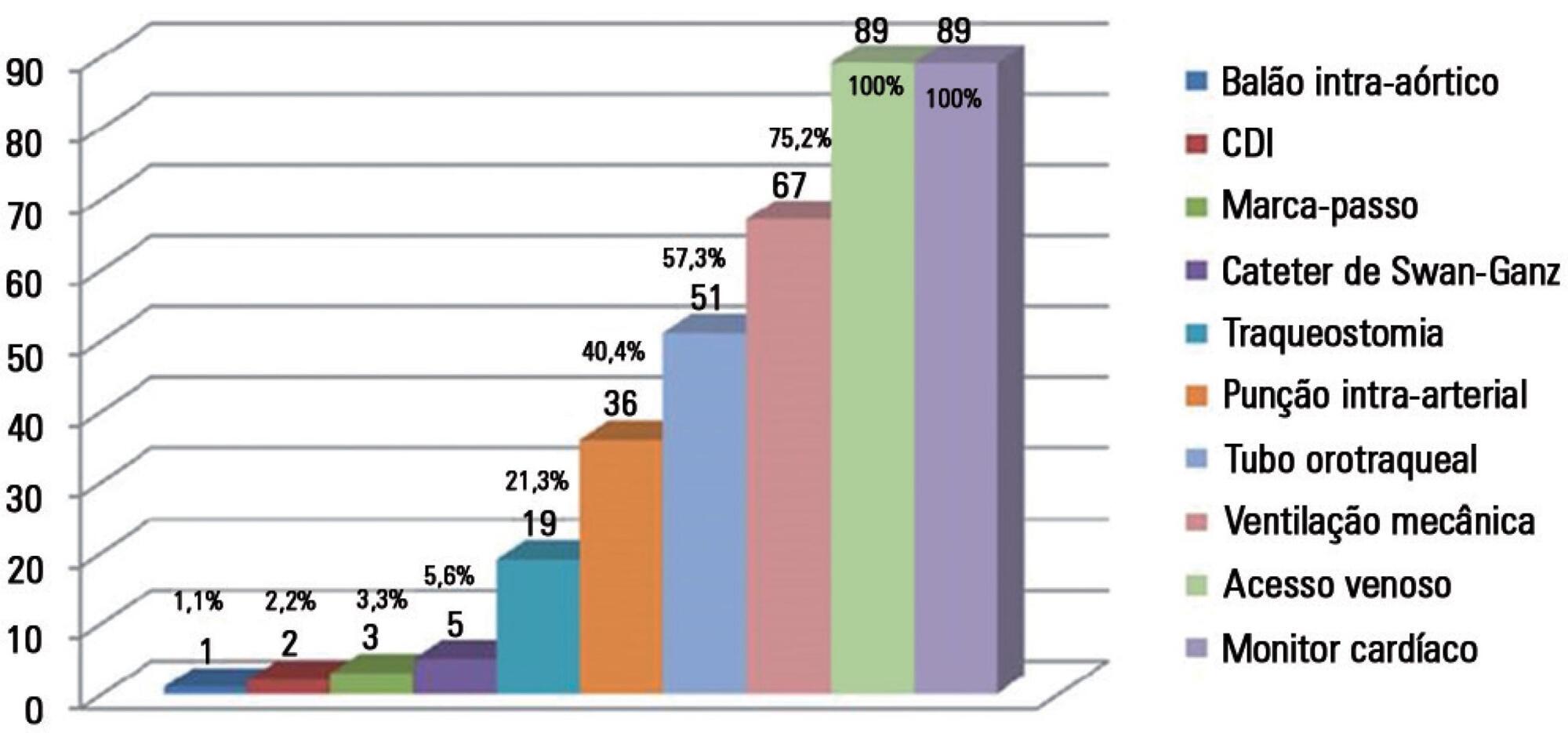
The study included 89 patients who underwent cardiopulmonary resuscitation maneuvers. The cohort was 51.6% male with a mean age 59.0 years. The episodes occurred during the daytime in 64.6% of cases. Asystole/bradyarrhythmia was the most frequent initial rhythm (42.7%). Most patients who exhibited a spontaneous return of circulation experienced recurrent cardiac arrest, especially within the first 24 hours (61.4%). The mean time elapsed between hospital admission and the occurrence of cardiac arrest was 10.3 days, the mean time between cardiac arrest and cardiopulmonary resuscitation was 0.68 min, the mean time between cardiac arrest and defibrillation was 7.1 min, and the mean duration of cardiopulmonary resuscitation was 16.3 min. Associations between gender and the duration of cardiopulmonary resuscitation (19.2 min in women versus 13.5 min in men, p = 0.02), the duration of cardiopulmonary resuscitation and the return of spontaneous circulation (10.8 min versus 30.7 min, p < 0.001) and heart disease and age (60.6 years versus 53.6, p < 0.001) were identified. The immediate survival rates after cardiac arrest, until hospital discharge and 6 months after discharge were 71%, 9% and 6%, respectively.
The main initial rhythm detected was asystole/bradyarrhythmia; the interval between cardiac arrest and cardiopulmonary resuscitation was short, but defibrillation was delayed. Women received cardiopulmonary resuscitation for longer periods than men. The in-hospital survival rate was low.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):322-332
DOI 10.5935/0103-507X.20150056
The determination of coma patient prognosis after cardiac arrest has clinical, ethical and social implications. Neurological examination, imaging and biochemical markers are helpful tools accepted as reliable in predicting recovery. With the advent of therapeutic hypothermia, these data need to be reconfirmed. In this study, we attempted to determine the validity of different markers, which can be used in the detection of patients with poor prognosis under hypothermia.
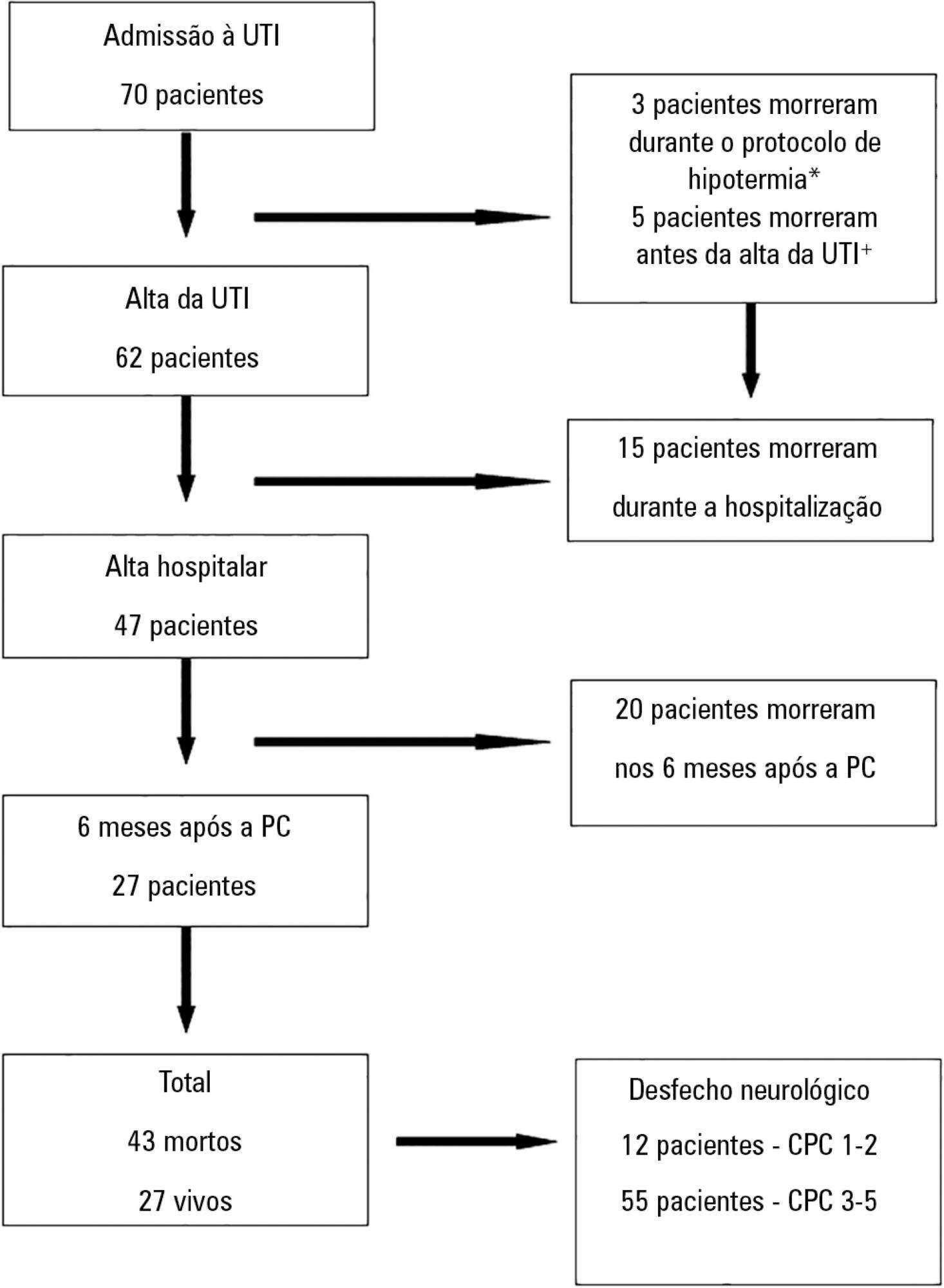
Data from adult patients admitted to our intensive care unit for a hypothermia protocol after cardiac arrest were recorded prospectively to generate a descriptive and analytical study analyzing the relationship between clinical, neurophysiological, imaging and biochemical parameters with 6-month outcomes defined according to the Cerebral Performance Categories scale (good 1-2, poor 3-5). Neuron-specific enolase was collected at 72 hours. Imaging and neurophysiologic exams were carried out in the 24 hours after the rewarming period.
Sixty-seven patients were included in the study, of which 12 had good neurological outcomes. Ventricular fibrillation and electroencephalographic theta activity were associated with increased likelihood of survival and improved neurological outcomes. Patients who had more rapid cooling (mean time of 163 versus 312 minutes), hypoxic-ischemic brain injury on magnetic resonance imaging or neuron-specific enolase > 58ng/mL had poor neurological outcomes (p < 0.05).
Hypoxic-ischemic brain injury on magnetic resonance imaging and neuron-specific enolase were strong predictors of poor neurological outcomes. Although there is the belief that early achievement of target temperature improves neurological prognoses, in our study, there were increased mortality and worse neurological outcomes with earlier target-temperature achievement.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):153-158
DOI 10.1590/S0103-507X2010000200009
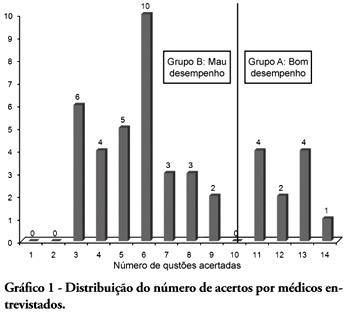
BACKGROUND: The main causes of cardiopulmonary arrest are endemic, and require constant medical improvement on cardiopulmonary resuscitation techniques. Training and continued education are essential to skilled management of cardiopulmonary resuscitation. OBJECTIVE: This study aimed to evaluate the physicians' theoretical knowledge on diagnosis and treatment of cardiopulmonary arrest. METHODS: This was a cross-sectional descriptive research conducted in a general hospital in Roraima, Brazil. The study population consisted of physicians who worked in the emergency department and intensive care units. The data were collected using a questionnaire addressing the subject. RESULTS: Forty four physicians answered the questionnaire. The mean score was 50% right answers. Most (88.5%) respondents committed "fatal errors". Half of the sample was never trained in advanced life support skills. No correlation was found between the number of right answers and attendance to advanced life support training courses. An inverse correlation was found between performance and age, but no statistically significant correlation was seen regarding performance and time from medical graduation. CONCLUSION: The physicians' theoretical knowledge on this field is worrisome. The results point to the importance of professional advanced life support training in order to assure quality standards for cardiac arrest management in this general hospital.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):196-205
DOI 10.1590/S0103-507X2010000200015
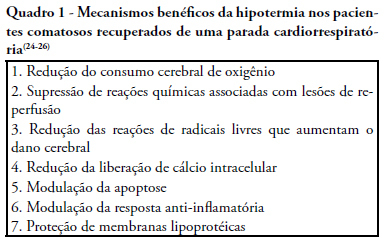
Cardiac arrest is a high mortality event and the associated brain ischemia frequently causes severe neurological damage and persistent vegetative state. Therapeutic hypothermia is an important tool for the treatment of post-anoxic coma after cardiopulmonary resuscitation. It has been shown to reduce mortality and to improve neurological outcomes after cardiac arrest. Nevertheless, hypothermia is underused in critical care units. This manuscript aims to review the hypothermia mechanism of action in cardiac arrest survivors and to propose a simple protocol, feasible to be implemented in any critical care unit.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):332-335
DOI 10.1590/S0103-507X2009000300015
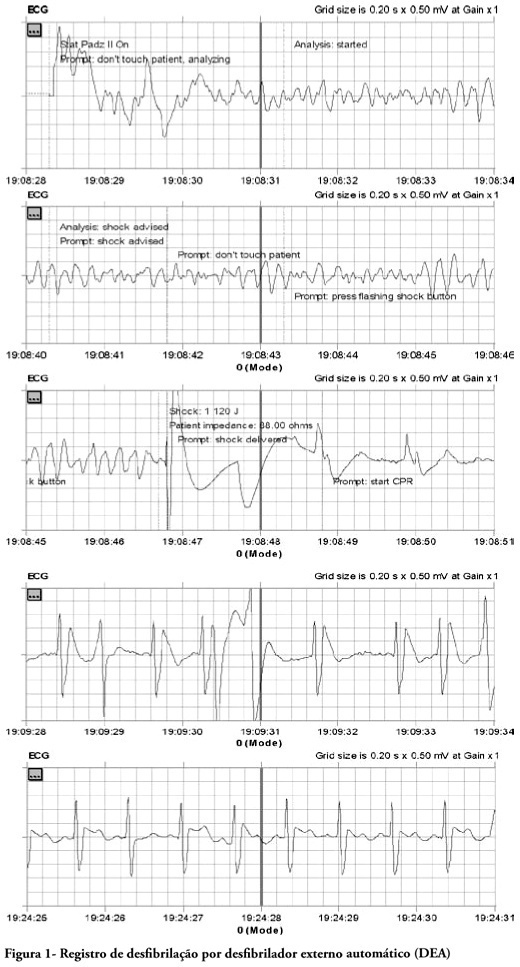
This case report relates out-of-hospital care to a patient with risk factors treated in the out-of-hospital services after cardiac arrest and ventricular fibrillation. The patient was treated according to the standards of basic life support and advanced cardiovascular life support; by applying an automated external defibrillator (AED) with favorable outcome and successful recovery of the patient from his risk of life condition. This is the first documented report with a favorable outcome in Peru, in out-of-hospital services and stresses the desirability of adopting policies for public access to early defibrillation.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):65-71
DOI 10.1590/S0103-507X2009000100010
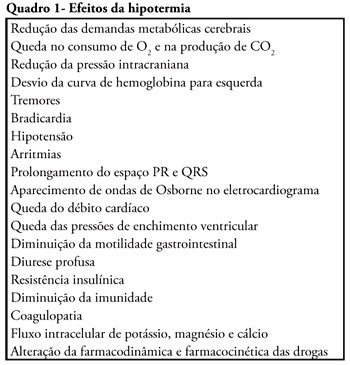
Cardiac arrest survivors frequently suffer from ischemic brain injury associated with poor neurological outcome and death. Therapeutic hypothermia improves outcomes in comatose survivors after resuscitation from out-of-hospital cardiac arrest. Considering its formal recommendation as a therapy, post-return of spontaneous circulation after cardiac arrest, the objective of this study was to review the clinical aspects of therapeutic hypothermia. Non-systematic review of articles using the keywords "cardiac arrest, cardiopulmonary resuscitation, cooling, hypothermia, post resuscitation syndrome" in the Med-Line database was performed. References of these articles were also reviewed. Unconscious adult patients with spontaneous circulation after out-of-hospital ventricular fibrillation or pulseless ventricular tachycardia should be cooled. Moreover, for any other rhythm or in the intra-hospital scenario, such cooling may also be beneficial. There are different ways of promoting hypothermia. The cooling system should be adjusted as soon as possible to the target temperature. Mild therapeutic hypothermia should be administered under close control, using neuromuscular blocking drugs to avoid shivering. The rewarming process should be slow, and reach 36º C, usually in no less then 8 hours. When temperature increases to more than 35º C, sedation, analgesia, and paralysis could be discontinued. The expected complications of hypothermia may be pneumonia, sepsis, cardiac arrhythmias, and coagulopathy. In spite of potential complications which require rigorous control, only six patients need to be treated to save one life.
Abstract
Rev Bras Ter Intensiva. 2006;18(2):177-185
DOI 10.1590/S0103-507X2006000200011
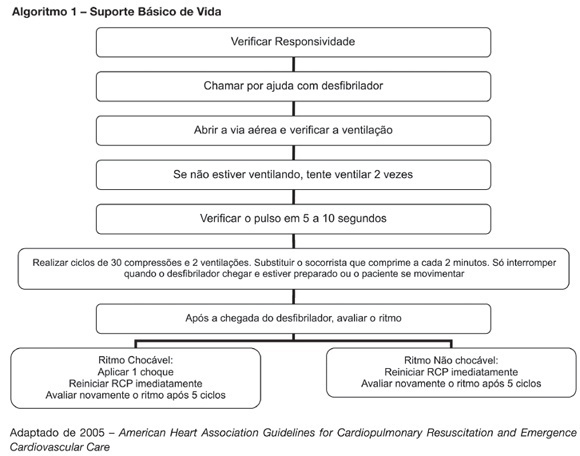
BACKGROUND AND OBJECTIVES: New resuscitation guidelines contain significant changes intended to improve resuscitation practice and survival from cardiac arrest. This article provides an overview of the key changes on resuscitation for healthcare provider. CONTENTS: There are several new recommendations on cardiopulmonary resuscitation (CPR), the major are intended to provide good circulation during cardiac arrest. The most important change is the emphasis on high-quality chest compressions with minimal interruptions. The universal 30:2 ratio is recommended to simplify training, to achieve optimal compression rates and to reduce the frequency of interruptions. Only one shock is delivered when indicated, followed immediately by CPR. This shock should be of 120-200J on a biphasic wave or 360J on a monophasic wave. Rescuers should not interrupt chest compressions to check rhythm until after about 5 cycles or approximately 2 minutes of CPR. After this period, if an organized rhythm is present, the healthcare provider should check for a pulse. There are several little changes about the drugs administrated during CPR according to the rhythm. Given the lack of documented effect of drug therapy in improving long-term outcome from cardiac arrest, the sequence for CPR deemphasizes drug administration and reemphasizes basic life support. CONCLUSIONS: The update on the new resuscitation guidelines is important to improve the quality of resuscitation and achieve better survival rates from our critical care patients.