Abstract
Rev Bras Ter Intensiva. 2021;33(1):96-101
DOI 10.5935/0103-507X.20210010
To evaluate changes in the characteristics of in-hospital cardiac arrest after the implementation of a Rapid Response Team.
This was a prospective observational study of in-hospital cardiac arrest that occurred from January 2013 to December 2017. The exclusion criterion was in-hospital cardiac arrest in the intensive care unit, emergency room or operating room. The Rapid Response Team was implemented in July 2014 in the study hospital. Patients were classified into two groups: a Pre-Rapid Response Team (in-hospital cardiac arrest before Rapid Response Team implementation) and a Post-Rapid Response Team (in-hospital cardiac arrest after Rapid Response Team implementation). Patients were followed until hospital discharge or death.
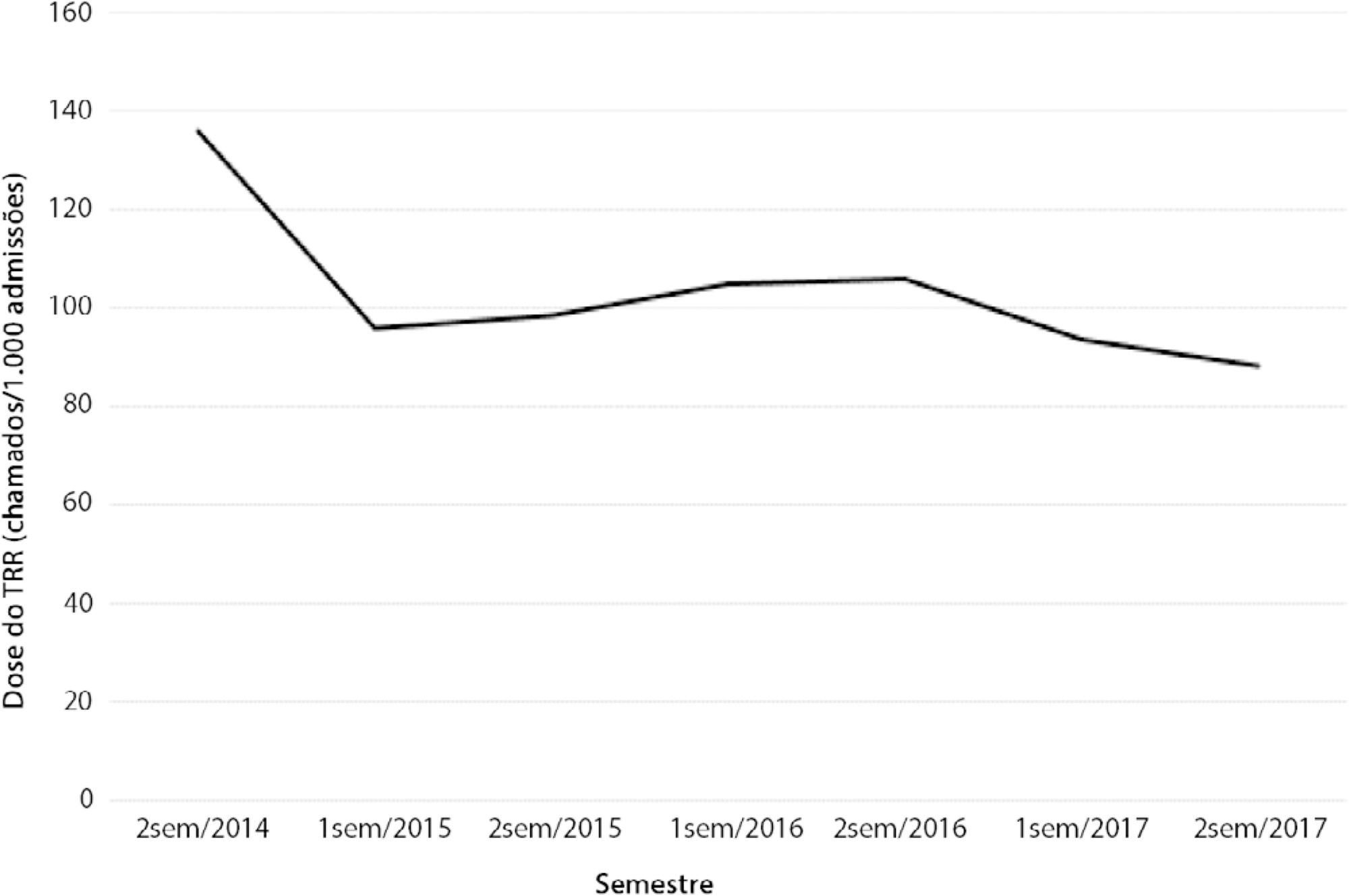
We had a total of 308 cardiac arrests (64.6 ± 15.2 years, 60.3% men, 13.9% with initial shockable rhythm). There was a decrease from 4.2 to 2.5 in-hospital cardiac arrest/1000 admissions after implementation of the Rapid Response Team, and we had approximately 124 calls/1000 admissions. Pre-Rapid Response Team cardiac arrest was associated with more hypoxia (29.4 versus 14.3%; p = 0.006) and an altered respiratory rate (14.7 versus 4.2%; p = 0.004) compared with post-Rapid Response Team cardiac arrest. Cardiac arrest due to hypoxia was more common before Rapid Response Team implementation (61.2 versus 38.1%, p < 0.001). In multivariate analysis, return of spontaneous circulation was associated with shockable rhythm (OR 2.97; IC95% 1.04 - 8.43) and witnessed cardiac arrest (OR 2.52; IC95% 1.39 - 4.59) but not with Rapid Response Team implementation (OR 1.40; IC95% 0.70 - 2.81) or premonitory signs (OR 0.71; IC95% 0.39 - 1.28). In multivariate analysis, in-hospital mortality was associated with non-shockable rhythm (OR 5.34; IC95% 2.28 - 12.53) and age (OR 1.03; IC95% 1.01 - 1.05) but not with Rapid Response Team implementation (OR 0.89; IC95% 0.40 - 2.02).
Even though Rapid Response Team implementation is associated with a reduction in in-hospital cardiac arrest, it was not associated with the mortality of in-hospital cardiac arrest victims. A significant decrease in cardiac arrests due to respiratory causes was noted after Rapid Response Team implementation.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):606-610
DOI 10.5935/0103-507X.20200099
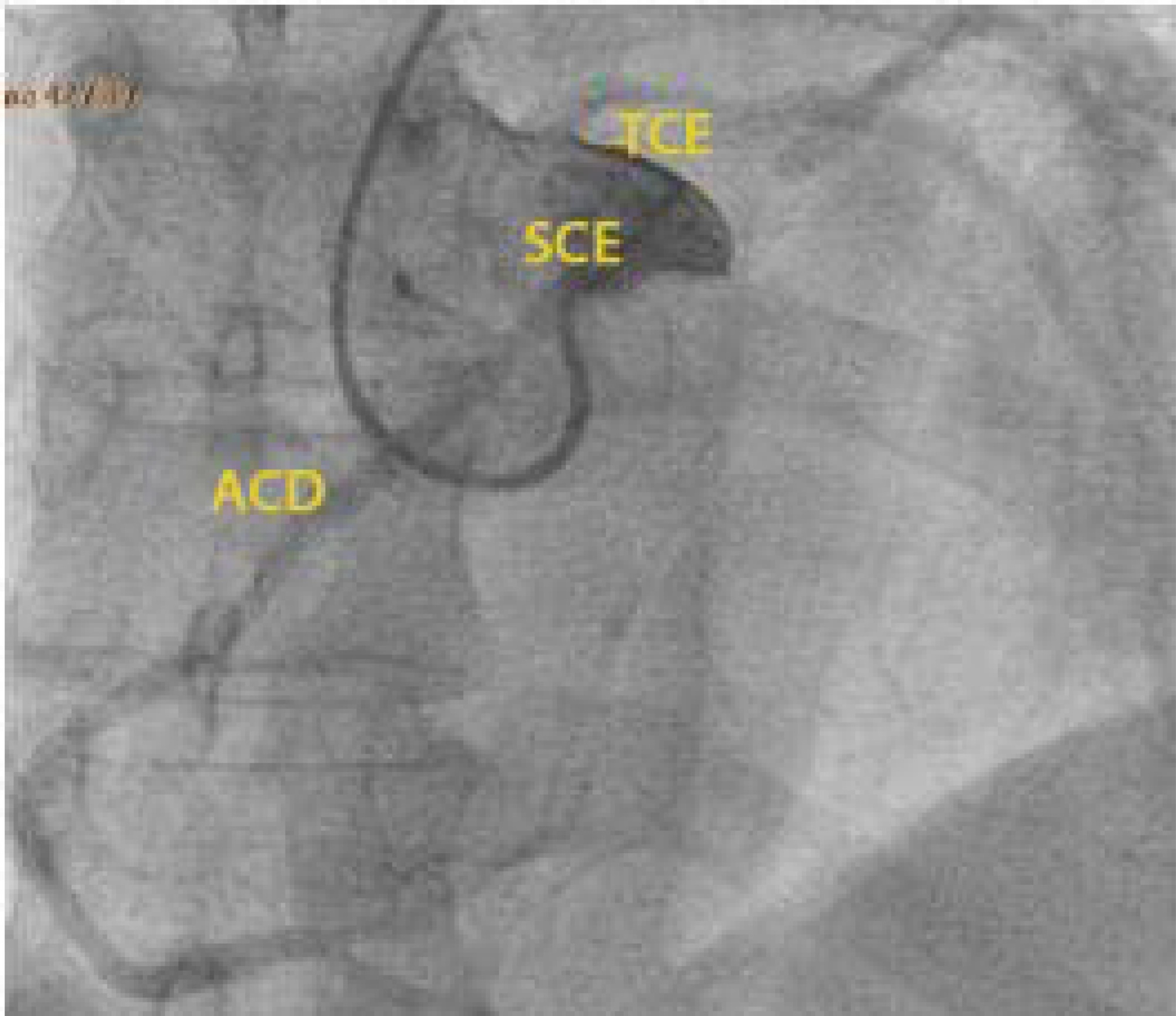
The authors report a rare case of successful Advanced Life Support in the context of cardiac arrest due to the presence of an anomalous aortic origin of the right coronary artery in a 49-year-old patient. The patient was admitted due to chest pain and dyspnea, with rapid evolution of pulseless ventricular tachycardia and cardiopulmonary arrest. Acute myocardial infarction was considered, and in the absence of a hemodynamic laboratory in the hospital, thrombolysis was performed. Subsequently, coronary angiography revealed no angiographic lesions in the coronary arteries and an anomalous right coronary artery originating from the opposite sinus of Valsalva. Coronary computed tomography angiography confirmed this finding and determined the course between the pulmonary artery and the aorta. The patient underwent cardiac surgery with a bypass graft to the right coronary artery, with no recurrent episodes of arrythmia.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):282-288
DOI 10.5935/0103-507X.20190053
To describe the epidemiological profile of victims of cardiac arrest assisted using a nontransporting emergency medical service vehicle and to determine whether these patients met the criteria for the use of extracorporeal membrane oxygenation.
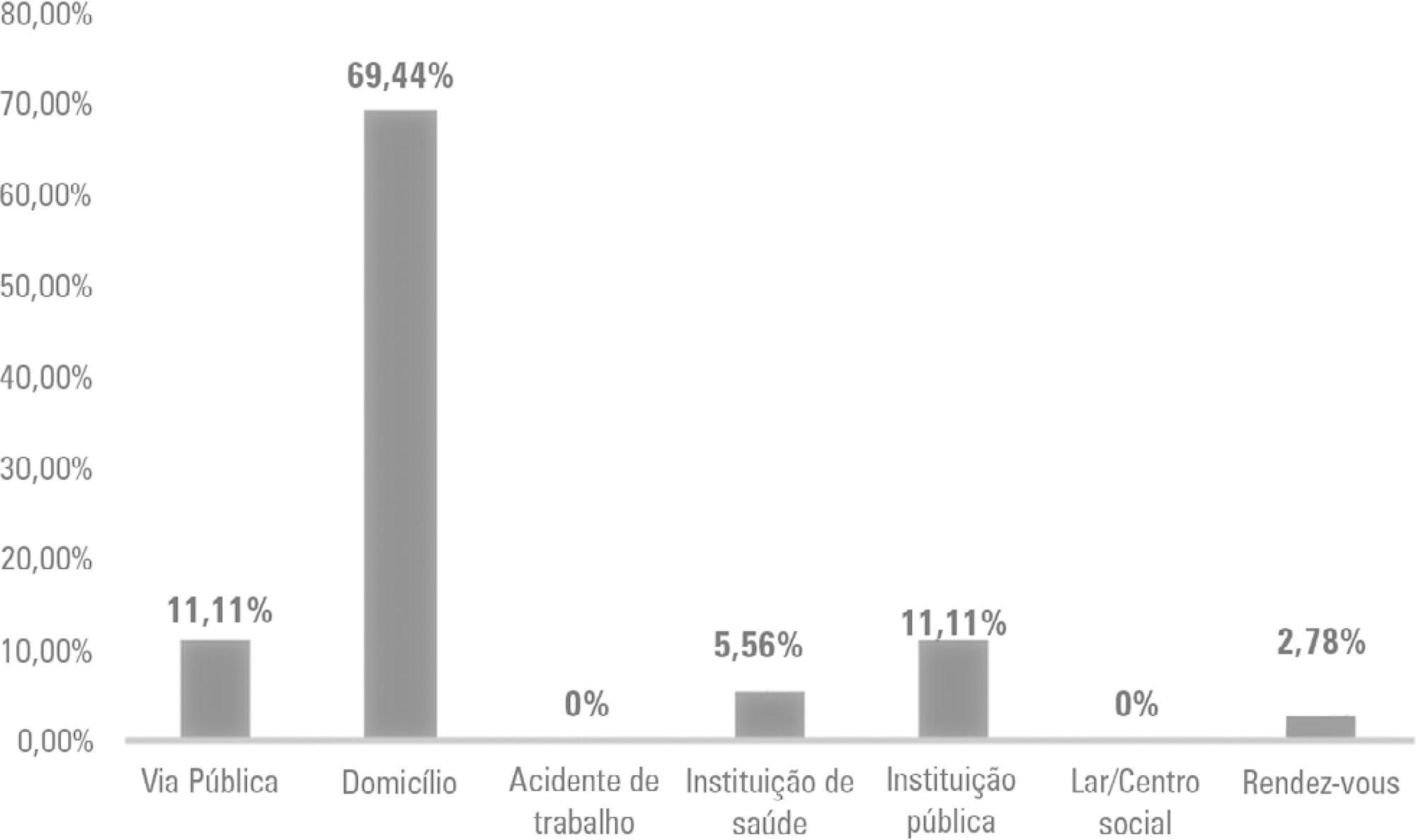
This study employed a retrospective, cohort, descriptive, and exploratory design. Data were collected in January 2018 in northern Portugal by consulting the records of nontransporting emergency medical service vehicles that provided assistance between 2012 and 2016. An observation grid was prepared that was supported by the instrument used for collecting data from the national registry of out-ofhospital cardiac arrests.
After applying the inclusion criteria, the sample consisted of 36 victims. Extracorporeal membrane oxygenation could have been applied to 24 victims during the period analyzed, which might have increased the odds for transplantation, survival, or both, for either the victim or other individuals.
Nontransporting emergency medical service vehicles have the potential for inclusion in the extracorporeal membrane oxygenation network of the study area.
Abstract
Rev Bras Ter Intensiva. 2018;30(3):366-375
DOI 10.5935/0103-507X.20180049
To evaluate the effectiveness of rapid response teams using early identification of clinical deterioration in reducing the occurrence of in-hospital mortality and cardiorespiratory arrest.
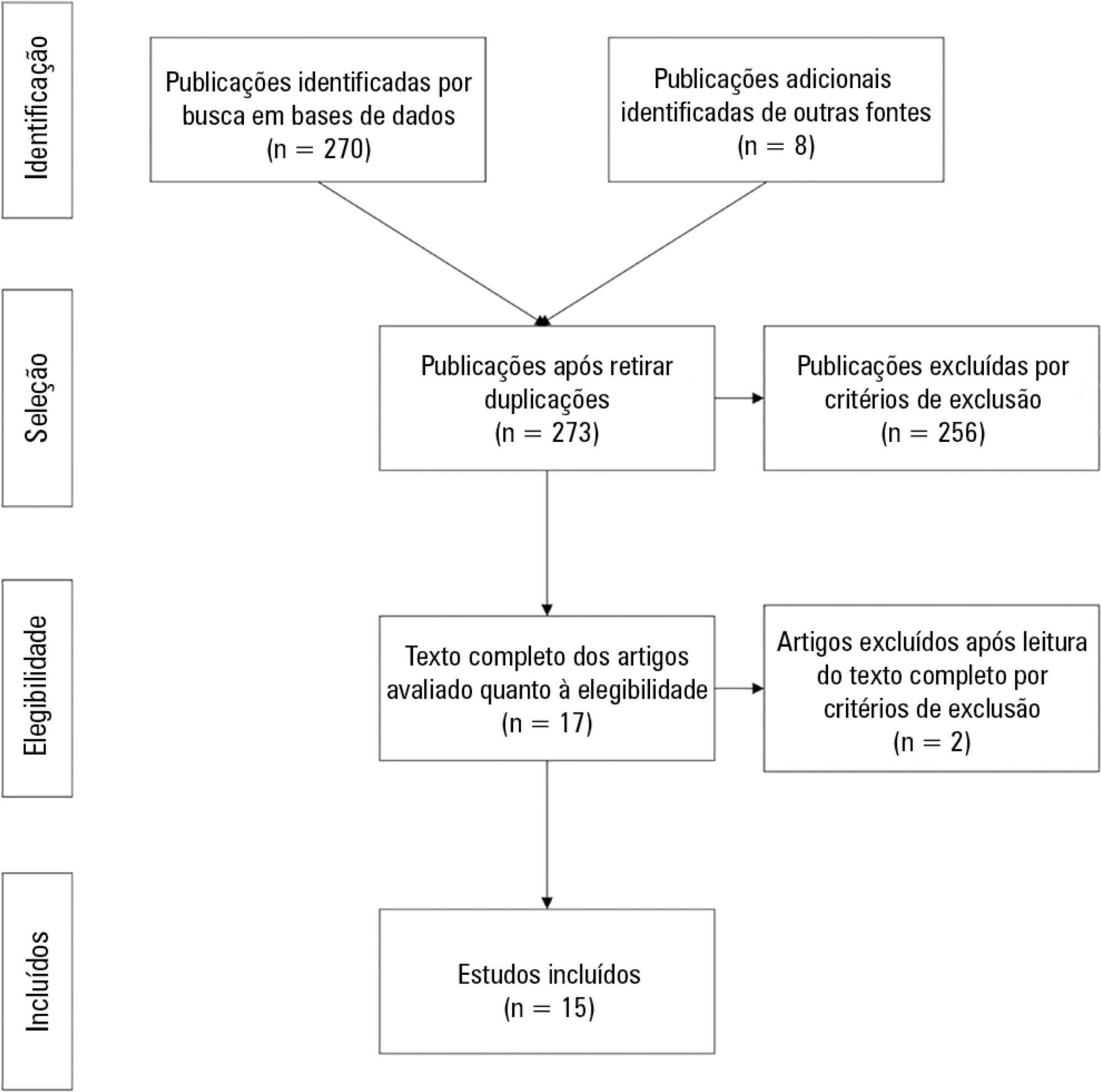
The MEDLINE, LILACS, Cochrane Library, Center for Reviews and Dissemination databases were searched.
We included studies that evaluated the effectiveness of rapid response teams in adult hospital units, published in English, Portuguese, or Spanish, from 2000 to 2016; systematic reviews, clinical trials, cohort studies, and prepost ecological studies were eligible for inclusion. The quality of studies was independently assessed by two researchers using the Newcastle-Ottawa, modified Jadad, and Assessment of Multiple Systematic Reviews scales.
The results were synthesized and tabulated. When risk measures were reported by the authors of the included studies, we estimated effectiveness as 1-RR or 1-OR. In pre-post studies, we estimated effectiveness as the percent decrease in rates following the intervention.
Overall, 278 studies were identified, 256 of which were excluded after abstract evaluation, and two of which were excluded after full text evaluation. In the meta-analysis of the studies reporting mortality data, we calculated a risk ratio of 0.85 (95%CI 0.76 - 0.94); and for studies reporting cardiac arrest data the estimated risk ratio was 0.65 (95%CI 0.49 - 0.87). Evidence was assessed as low quality due to the high heterogeneity and risk of bias in primary studies.
We conclude that rapid response teams may reduce in-hospital mortality and cardiac arrests, although the quality of evidence for both outcomes is low.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):427-435
DOI 10.5935/0103-507X.20160076
The objective of this study was to analyze the clinical profile of patients with in-hospital cardiac arrest using the Utstein style.
This study is an observational, prospective, longitudinal study of patients with cardiac arrest treated in intensive care units over a period of 1 year.
The study included 89 patients who underwent cardiopulmonary resuscitation maneuvers. The cohort was 51.6% male with a mean age 59.0 years. The episodes occurred during the daytime in 64.6% of cases. Asystole/bradyarrhythmia was the most frequent initial rhythm (42.7%). Most patients who exhibited a spontaneous return of circulation experienced recurrent cardiac arrest, especially within the first 24 hours (61.4%). The mean time elapsed between hospital admission and the occurrence of cardiac arrest was 10.3 days, the mean time between cardiac arrest and cardiopulmonary resuscitation was 0.68 min, the mean time between cardiac arrest and defibrillation was 7.1 min, and the mean duration of cardiopulmonary resuscitation was 16.3 min. Associations between gender and the duration of cardiopulmonary resuscitation (19.2 min in women versus 13.5 min in men, p = 0.02), the duration of cardiopulmonary resuscitation and the return of spontaneous circulation (10.8 min versus 30.7 min, p < 0.001) and heart disease and age (60.6 years versus 53.6, p < 0.001) were identified. The immediate survival rates after cardiac arrest, until hospital discharge and 6 months after discharge were 71%, 9% and 6%, respectively.
The main initial rhythm detected was asystole/bradyarrhythmia; the interval between cardiac arrest and cardiopulmonary resuscitation was short, but defibrillation was delayed. Women received cardiopulmonary resuscitation for longer periods than men. The in-hospital survival rate was low.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):322-332
DOI 10.5935/0103-507X.20150056
The determination of coma patient prognosis after cardiac arrest has clinical, ethical and social implications. Neurological examination, imaging and biochemical markers are helpful tools accepted as reliable in predicting recovery. With the advent of therapeutic hypothermia, these data need to be reconfirmed. In this study, we attempted to determine the validity of different markers, which can be used in the detection of patients with poor prognosis under hypothermia.
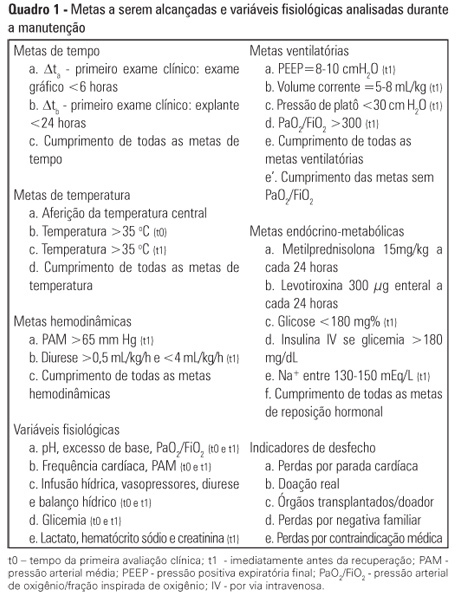
Data from adult patients admitted to our intensive care unit for a hypothermia protocol after cardiac arrest were recorded prospectively to generate a descriptive and analytical study analyzing the relationship between clinical, neurophysiological, imaging and biochemical parameters with 6-month outcomes defined according to the Cerebral Performance Categories scale (good 1-2, poor 3-5). Neuron-specific enolase was collected at 72 hours. Imaging and neurophysiologic exams were carried out in the 24 hours after the rewarming period.
Sixty-seven patients were included in the study, of which 12 had good neurological outcomes. Ventricular fibrillation and electroencephalographic theta activity were associated with increased likelihood of survival and improved neurological outcomes. Patients who had more rapid cooling (mean time of 163 versus 312 minutes), hypoxic-ischemic brain injury on magnetic resonance imaging or neuron-specific enolase > 58ng/mL had poor neurological outcomes (p < 0.05).
Hypoxic-ischemic brain injury on magnetic resonance imaging and neuron-specific enolase were strong predictors of poor neurological outcomes. Although there is the belief that early achievement of target temperature improves neurological prognoses, in our study, there were increased mortality and worse neurological outcomes with earlier target-temperature achievement.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):334-340
DOI 10.1590/S0103-507X2012000400007
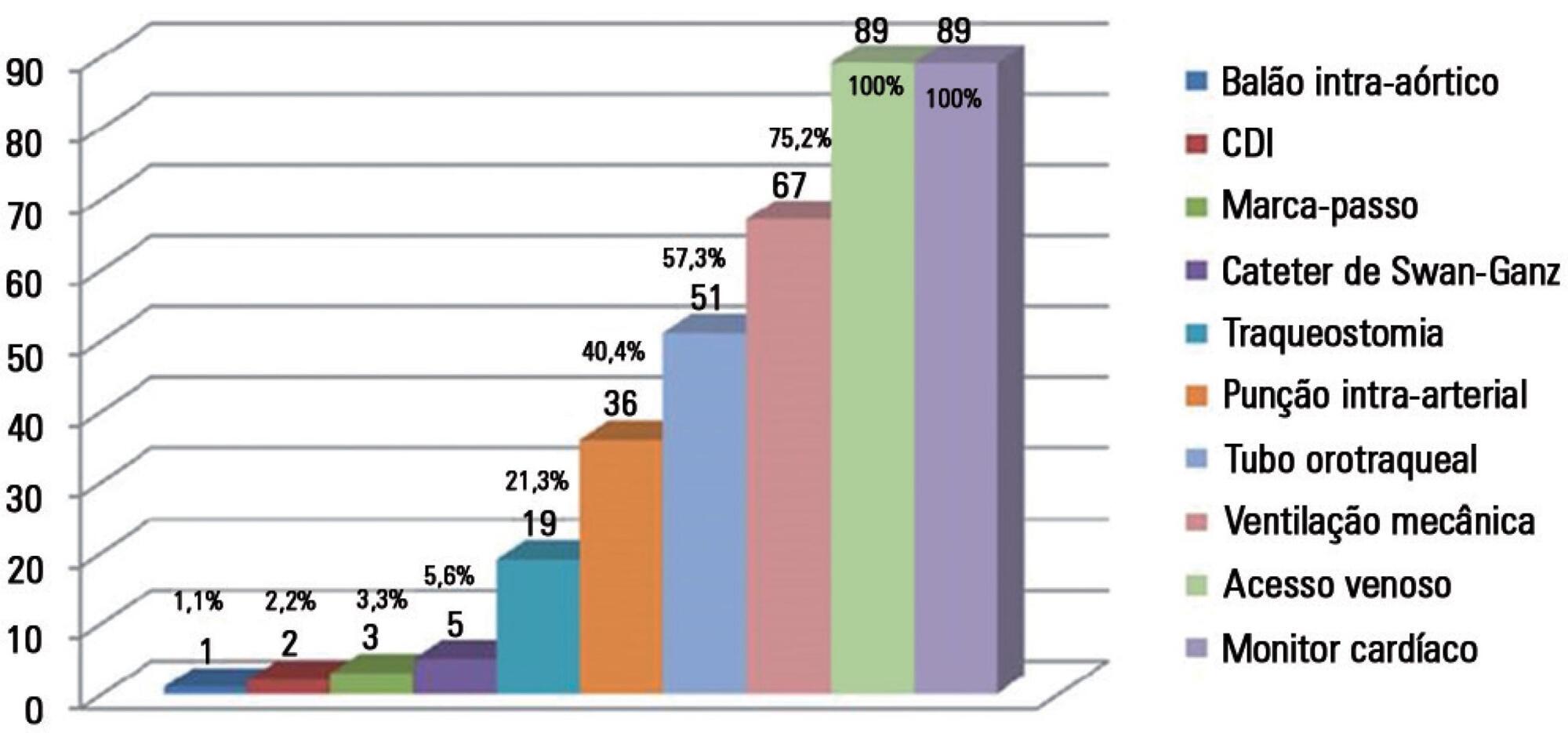
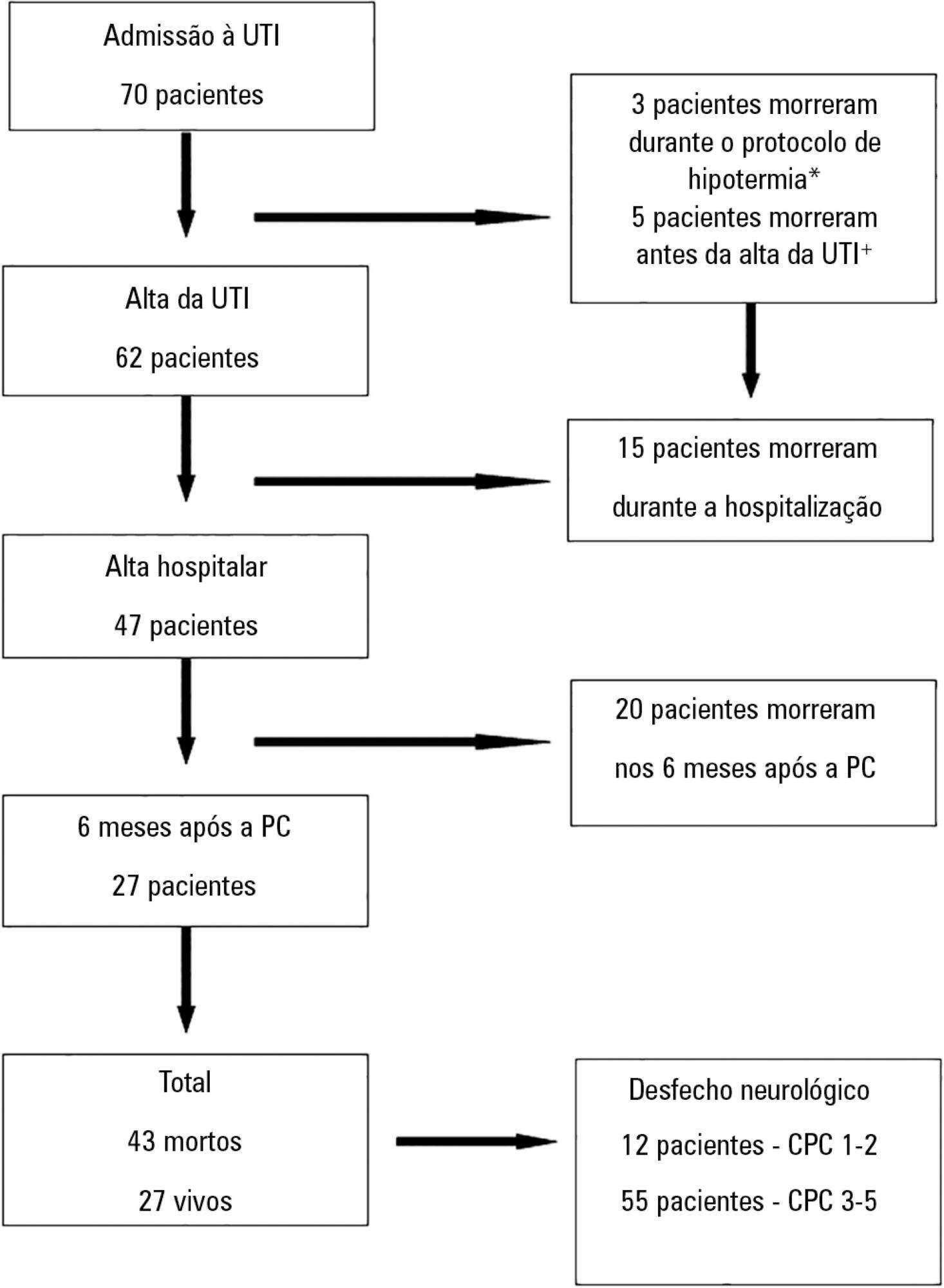
OBJECTIVE: To assess the effect of the application of a managed protocol for the maintenance care of deceased potential multiple organ donors at two hospitals. METHODS: A before (Phase 1)/after (Phase 2) study conducted at two general hospitals, which included consecutively potential donors admitted to two intensive care units. In Phase 1 (16 months), the data were collected retrospectively, and the maintenance care measures of the potential donors were instituted by the intensivists. In Phase 2 (12 months), the data collection was prospective, and a managed protocol was used for maintenance care. The two phases were compared in terms of their demographic variables, physiological variables at diagnosis of brain death and the end of the process, time to performance of brain death confirmatory test and end of the process, adherence to bundles of maintenance care essential measures, losses due to cardiac arrest, family refusal, contraindications, and the conversion rate of potential into actual donors. Student's t- and chi-square tests were used, and p-value < 0.05 was considered to be significant. RESULTS: A total of 42 potential donors were identified (18 in Phase 1 and 24 in Phase 2). The time interval between the first clinical assessment and the recovery decreased in Phase 2 (Phase 1: 35.0±15.5 hours versus Phase 2: 24.6±6.2 hours; p = 0.023). Adherence increased to 10 out of the 19 essential items of maintenance care, and losses due to cardiac arrest also decreased in Phase 2 (Phase 1: 27.8 versus 0% in Phase 2; p = 0.006), while the convertion rate increased (Phase 1: 44.4 versus 75% in Phase 2; p = 0.044). The losses due to family refusal and medical contraindication did not vary. CONCLUSION: The adoption of a managed protocol focused on the application of essential measures for the care of potential deceased donors might reduce the loss of potential donors due to cardiac arrest.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):455-461
DOI 10.1590/S0103-507X2011000400010
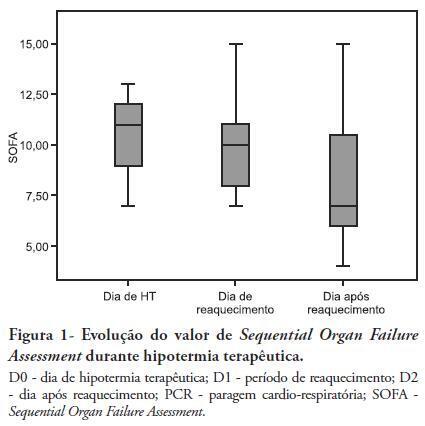
OBJECTIVES: Therapeutic hypothermia following cardiorespiratory arrest has been demonstrated to have cardio- and neuroprotective effects, resulting in improved survival and better neurological outcomes. The objective of this study was to assess the outcomes of patients undergoing therapeutic hypothermia following cardiorespiratory arrest. METHODS: A prospective, 10-month observational study of patients admitted to an intensive care unit and undergoing therapeutic hypothermia after cardiorespiratory arrest was undertaken. Therapeutic hypothermia was induced by cold fluid administration and body surface cooling in patients admitted no more than 12 hours after resuscitation from cardiorespiratory arrest. A target temperature of 33ºC was maintained for 24 hours. RESULTS: Overall, 12 patients were included (median age 64 years, 58% male). Half of the cardiorespiratory arrests were in-hospital. The median first-day Charlson Index, Sequential Organ Failure Assessment (SOFA) and Acute Physiology and Chronic Health Evaluation II scores were of 2.9, 11 and 24.5, respectively. The intensive care unit mortality rate was 42% (N=5). Five of the 7 surviving patients recovered their pre-cardiorespiratory arrest neurological status. Hypothermia was initiated 120 min (median) after recovery of spontaneous circulation. Most patients (75%) required vasopressor support. During the first 3 days after cardiorespiratory arrest and therapeutic hypothermia, a progressive SOFA score decrease (median 11 on day 0, 10 on day 1 and 7 on day 2) was observed. DISCUSSION: In this study, therapeutic hypothermia was applied to all post-cardiorespiratory arrest patients and demonstrated good neurological outcome in surviving patients.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)