You searched for:"Joana Silvestre"
We found (4) results for your search.-
Original Article
suPAR in the assessment of post intensive care unit prognosis: a pilot study
Rev Bras Ter Intensiva. 2018;30(4):453-459
Abstract
Original ArticlesuPAR in the assessment of post intensive care unit prognosis: a pilot study
Rev Bras Ter Intensiva. 2018;30(4):453-459
DOI 10.5935/0103-507X.20180062
Views0See moreABSTRACT
Objective:
To determine the performance of soluble urokinase-type plasminogen activator receptor upon intensive care unit discharge to predict post intensive care unit mortality.
Methods:
A prospective observational cohort study was conducted during a 24-month period in an 8-bed polyvalent intensive care unit. APACHE II, SOFA, C-reactive protein, white cell count and soluble urokinase-type plasminogen activator receptor on the day of intensive care unit discharge were collected from patients who survived intensive care unit admission.
Results:
Two hundred and two patients were included in this study, 29 patients (18.6%) of whom died after intensive care unit discharge. Nonsurvivors were older and more seriously ill upon intensive care unit admission with higher severity scores, and nonsurvivors required extended use of vasopressors than did survivors. The area under the receiver operating characteristics curves of SOFA, APACHE II, C-reactive protein, white cell count, and soluble urokinase-type plasminogen activator receptor at intensive care unit discharge as prognostic markers of hospital death were 0.78 (95%CI 0.70 – 0.86); 0.70 (95%CI 0.61 – 0.79); 0.54 (95%CI 0.42 – 0.65); 0.48 (95%CI 0.36 – 0.58); and 0.68 (95%CI 0.58 – 0.78), respectively. SOFA was independently associated with a higher risk of in-hospital mortality (OR 1.673; 95%CI 1.252 – 2.234), 28-day mortality (OR 1.861; 95%CI 1.856 – 2.555) and 90-day mortality (OR 1.584; 95%CI 1.241 – 2.022).
Conclusion:
At intensive care unit discharge, soluble urokinase-type plasminogen activator receptor is a poor predictor of post intensive care unit prognosis.
-
Case Reports
Heliox in the treatment of status asthmaticus: case reports
Rev Bras Ter Intensiva. 2016;28(1):87-91
Abstract
Case ReportsHeliox in the treatment of status asthmaticus: case reports
Rev Bras Ter Intensiva. 2016;28(1):87-91
DOI 10.5935/0103-507X.20160005
Views0See moreABSTRACT
Helium was discovered in 1868 by the French astronomer Pierre-Jules-César Janssen and was first used as a therapeutic treatment for airway obstruction by Barach almost 70 years later, in 1934. Heliox is characterized by its low density, which makes it more fluid under conditions of turbulence, thus minimizing airway pressure and facilitating the occurrence of laminar flow. The present article describes two clinical cases of patients with status asthmaticus subjected to mechanical ventilation and refractory to treatment in whom heliox was used, which allowed optimization of the efficacy of conventional pharmacological treatments. Although heliox is still used sporadically and its true efficacy has not been well demonstrated, the unique physical properties of helium and the theoretical improvement of the airflow in obstructed airways have produced scientific interest and stimulated research. Heliox can be used simultaneously with conventional therapies in cases of serious and refractory exacerbations of severe obstructive disease.

-
Original Articles – Clinical Research
The neuroprotective role of therapeutic hypothermia after cardiac arrest
Rev Bras Ter Intensiva. 2011;23(4):455-461
Abstract
Original Articles – Clinical ResearchThe neuroprotective role of therapeutic hypothermia after cardiac arrest
Rev Bras Ter Intensiva. 2011;23(4):455-461
DOI 10.1590/S0103-507X2011000400010
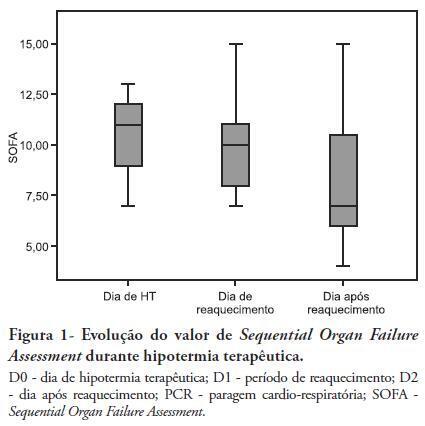
Views0See moreOBJECTIVES: Therapeutic hypothermia following cardiorespiratory arrest has been demonstrated to have cardio- and neuroprotective effects, resulting in improved survival and better neurological outcomes. The objective of this study was to assess the outcomes of patients undergoing therapeutic hypothermia following cardiorespiratory arrest. METHODS: A prospective, 10-month observational study of patients admitted to an intensive care unit and undergoing therapeutic hypothermia after cardiorespiratory arrest was undertaken. Therapeutic hypothermia was induced by cold fluid administration and body surface cooling in patients admitted no more than 12 hours after resuscitation from cardiorespiratory arrest. A target temperature of 33ºC was maintained for 24 hours. RESULTS: Overall, 12 patients were included (median age 64 years, 58% male). Half of the cardiorespiratory arrests were in-hospital. The median first-day Charlson Index, Sequential Organ Failure Assessment (SOFA) and Acute Physiology and Chronic Health Evaluation II scores were of 2.9, 11 and 24.5, respectively. The intensive care unit mortality rate was 42% (N=5). Five of the 7 surviving patients recovered their pre-cardiorespiratory arrest neurological status. Hypothermia was initiated 120 min (median) after recovery of spontaneous circulation. Most patients (75%) required vasopressor support. During the first 3 days after cardiorespiratory arrest and therapeutic hypothermia, a progressive SOFA score decrease (median 11 on day 0, 10 on day 1 and 7 on day 2) was observed. DISCUSSION: In this study, therapeutic hypothermia was applied to all post-cardiorespiratory arrest patients and demonstrated good neurological outcome in surviving patients.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




