Abstract
Rev Bras Ter Intensiva. 2018;30(4):453-459
DOI 10.5935/0103-507X.20180062
To determine the performance of soluble urokinase-type plasminogen activator receptor upon intensive care unit discharge to predict post intensive care unit mortality.
A prospective observational cohort study was conducted during a 24-month period in an 8-bed polyvalent intensive care unit. APACHE II, SOFA, C-reactive protein, white cell count and soluble urokinase-type plasminogen activator receptor on the day of intensive care unit discharge were collected from patients who survived intensive care unit admission.
Two hundred and two patients were included in this study, 29 patients (18.6%) of whom died after intensive care unit discharge. Nonsurvivors were older and more seriously ill upon intensive care unit admission with higher severity scores, and nonsurvivors required extended use of vasopressors than did survivors. The area under the receiver operating characteristics curves of SOFA, APACHE II, C-reactive protein, white cell count, and soluble urokinase-type plasminogen activator receptor at intensive care unit discharge as prognostic markers of hospital death were 0.78 (95%CI 0.70 - 0.86); 0.70 (95%CI 0.61 - 0.79); 0.54 (95%CI 0.42 - 0.65); 0.48 (95%CI 0.36 - 0.58); and 0.68 (95%CI 0.58 - 0.78), respectively. SOFA was independently associated with a higher risk of in-hospital mortality (OR 1.673; 95%CI 1.252 - 2.234), 28-day mortality (OR 1.861; 95%CI 1.856 - 2.555) and 90-day mortality (OR 1.584; 95%CI 1.241 - 2.022).
At intensive care unit discharge, soluble urokinase-type plasminogen activator receptor is a poor predictor of post intensive care unit prognosis.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):130-136
DOI 10.5935/0103-507X.20140019
To assess the performance of central venous oxygen saturation, lactate, base deficit, and C-reactive protein levels and SOFA and SWIFT scores on the day of discharge from the intensive care unit as predictors of patient readmission to the intensive care unit.
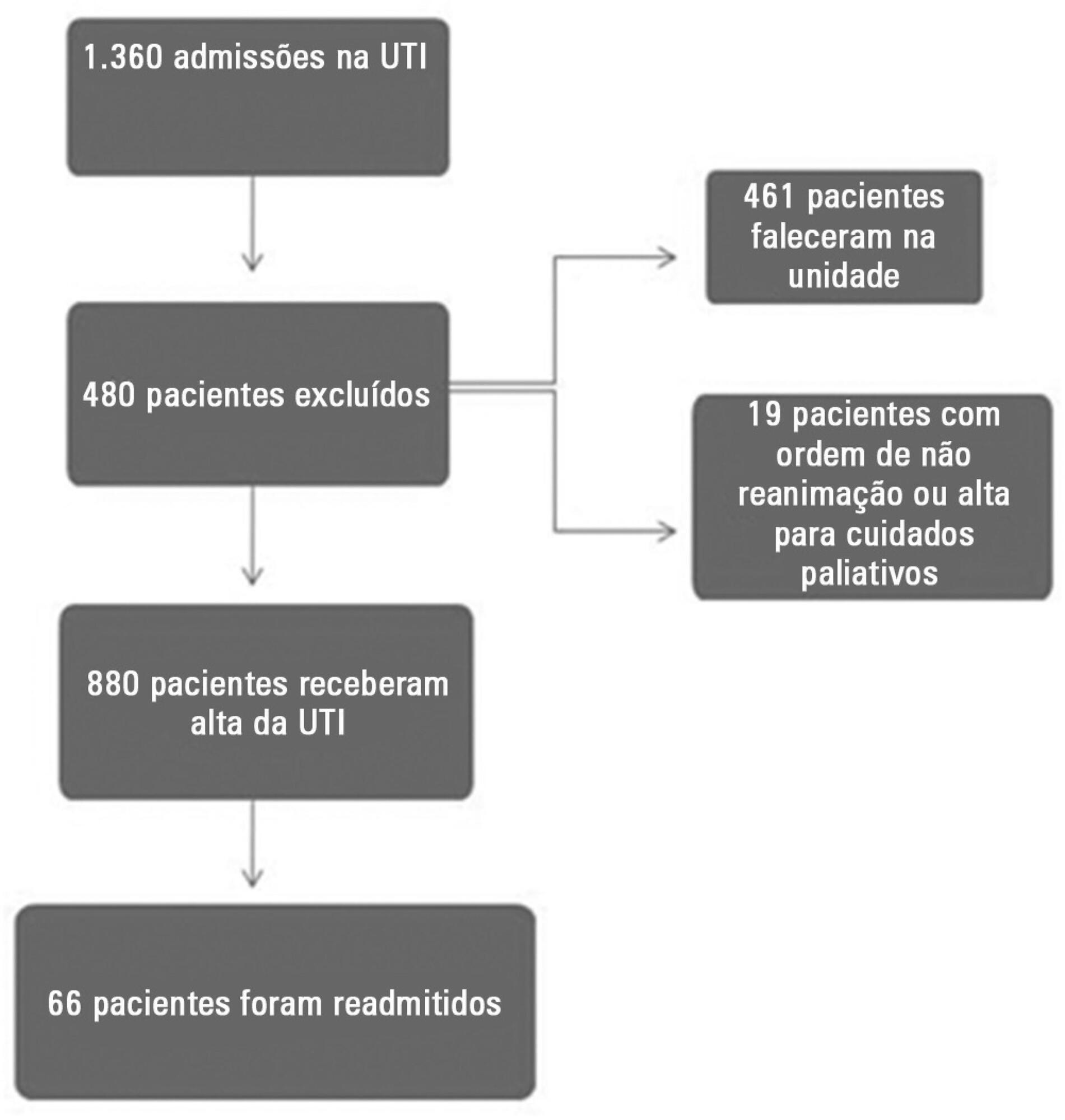
This prospective and observational study collected data from 1,360 patients who were admitted consecutively to a clinical-surgical intensive care unit from August 2011 to August 2012. The clinical characteristics and laboratory data of readmitted and non-readmitted patients after discharge from the intensive care unit were compared. Using a multivariate analysis, the risk factors independently associated with readmission were identified.
The C-reactive protein, central venous oxygen saturation, base deficit, and lactate levels and the SWIFT and SOFA scores did not correlate with the readmission of critically ill patients. Increased age and contact isolation because of multidrug-resistant organisms were identified as risk factors that were independently associated with readmission in this study group.
Inflammatory and perfusion parameters were not associated with patient readmission. Increased age and contact isolation because of multidrug-resistant organisms were identified as predictors of readmission to the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):6-11
DOI 10.1590/S0103-507X2013000100003
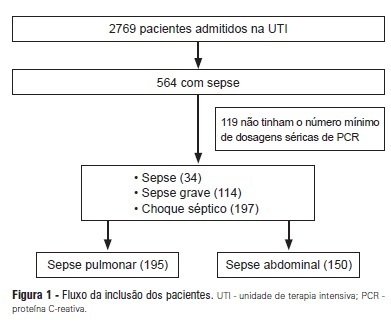
OBJECTIVES: To evaluate the C-reactive protein serum levels in patients with pulmonary and abdominal sepsis during the first five days of sepsis progression. METHODS: The present investigation was a retrospective cohort study conducted at the university hospital with 345 patients who were admitted to the intensive care unit and diagnosed with sepsis of pulmonary or abdominal origin. Serum C-reactive protein concentrations were measured by the turbidimetric immunoassay. For analysis of C-reactive protein, day 1 was defined as the day on which the patient was clinically diagnosed with sepsis. RESULTS: Thirty-four patients with sepsis (9.8%), 114 patients with severe sepsis (33.0%), and 197 patients with septic shock (57.2%) were evaluated. The age of the patients was 56.4±19.8 years. The serum C-reactive protein concentrations were higher on the day of sepsis diagnosis in the group with abdominal infection compared with the group with pulmonary sepsis (17.8±10.1 mg/dL versus 14.9±11.1 mg/dL, p=0.025) and remained significantly higher during the first five days of sepsis progression. CONCLUSION: The serum C-reactive protein concentrations were significantly higher in the patients with abdominal sepsis compared with the patients with pulmonary sepsis during the first five days of sepsis progression.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)