Abstract
Rev Bras Ter Intensiva. 2010;22(2):153-158
DOI 10.1590/S0103-507X2010000200009
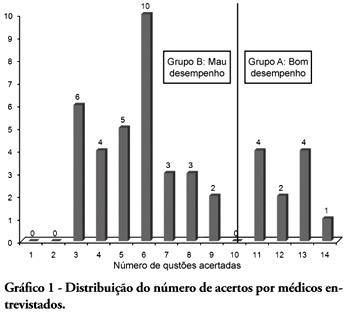
BACKGROUND: The main causes of cardiopulmonary arrest are endemic, and require constant medical improvement on cardiopulmonary resuscitation techniques. Training and continued education are essential to skilled management of cardiopulmonary resuscitation. OBJECTIVE: This study aimed to evaluate the physicians' theoretical knowledge on diagnosis and treatment of cardiopulmonary arrest. METHODS: This was a cross-sectional descriptive research conducted in a general hospital in Roraima, Brazil. The study population consisted of physicians who worked in the emergency department and intensive care units. The data were collected using a questionnaire addressing the subject. RESULTS: Forty four physicians answered the questionnaire. The mean score was 50% right answers. Most (88.5%) respondents committed "fatal errors". Half of the sample was never trained in advanced life support skills. No correlation was found between the number of right answers and attendance to advanced life support training courses. An inverse correlation was found between performance and age, but no statistically significant correlation was seen regarding performance and time from medical graduation. CONCLUSION: The physicians' theoretical knowledge on this field is worrisome. The results point to the importance of professional advanced life support training in order to assure quality standards for cardiac arrest management in this general hospital.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):196-205
DOI 10.1590/S0103-507X2010000200015
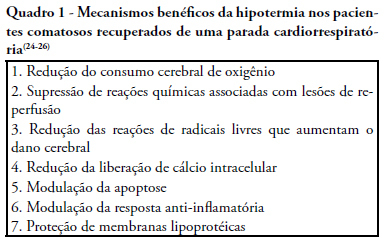
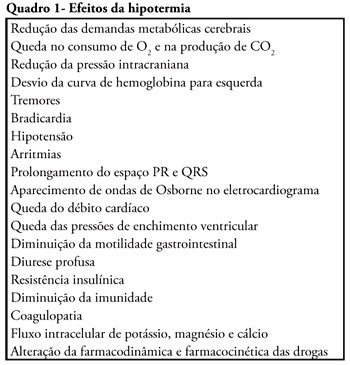
Cardiac arrest is a high mortality event and the associated brain ischemia frequently causes severe neurological damage and persistent vegetative state. Therapeutic hypothermia is an important tool for the treatment of post-anoxic coma after cardiopulmonary resuscitation. It has been shown to reduce mortality and to improve neurological outcomes after cardiac arrest. Nevertheless, hypothermia is underused in critical care units. This manuscript aims to review the hypothermia mechanism of action in cardiac arrest survivors and to propose a simple protocol, feasible to be implemented in any critical care unit.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):369-375
DOI 10.1590/S0103-507X2009000400006
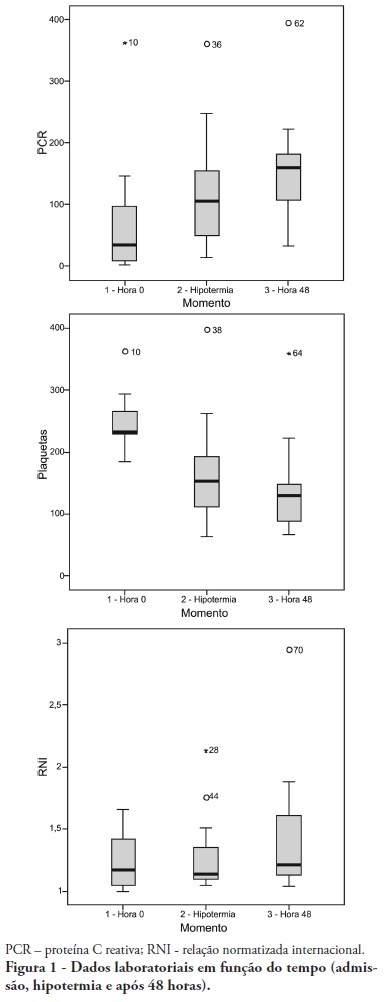
OBJECTIVE: To determine the characteristics of patients undergoing standard institutional protocol for management of resuscitated patients after a cardiac arrest episode, including therapeutic hypothermia. METHODS: This was a retrospective analysis of 26 consecutive patients admitted following cardiac arrest, between January 2007 and November 2008. RESULTS: All cases underwent therapeutic hypothermia. Average age was 63 years, and the patients were predominantly male. Cardiac arrest event was out-of-hospital in 8 cases, in the emergency room in 3 cases, in the wards in 13 cases and in the operation room in 2 cases. The cardiac arrest rhythm was ventricular fibrillation in seven patients, asystolia in 11, pulseless electrical activity in 5 cases, and was undetermined in 3 patients. The interval between the cardiac arrest and return of spontaneous circulation was 12 minutes (SD ± 5 min). The time to reach the target temperature was 5 ± 4 hours, the hypothermia time was 22 ± 6 hours and time to rewarming 9 ± 5.9 hours. Fourteen patients died in the intensive care unit, a 54% mortality, and three patients died during the in-hospital stay, a 66% in-hospital mortality. There was statistically significant reduction in hemoglobin (p<0.001), leukocytes (p=0.001), platelets (p<0.001), lactate (p<0.001) and potassium (p=0.009), values and increased C reactive protein (p=0.001) and INR (p=0.004) after hypothermia. CONCLUSIONS: The creation of a standard operative protocol for therapeutic hypothermia in post cardiac arrest patients management resulted in a high use of therapeutic hypothermia. The clinical results of this protocol adapted from randomized studies are similar to the literature.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):437-445
DOI 10.1590/S0103-507X2009000400015
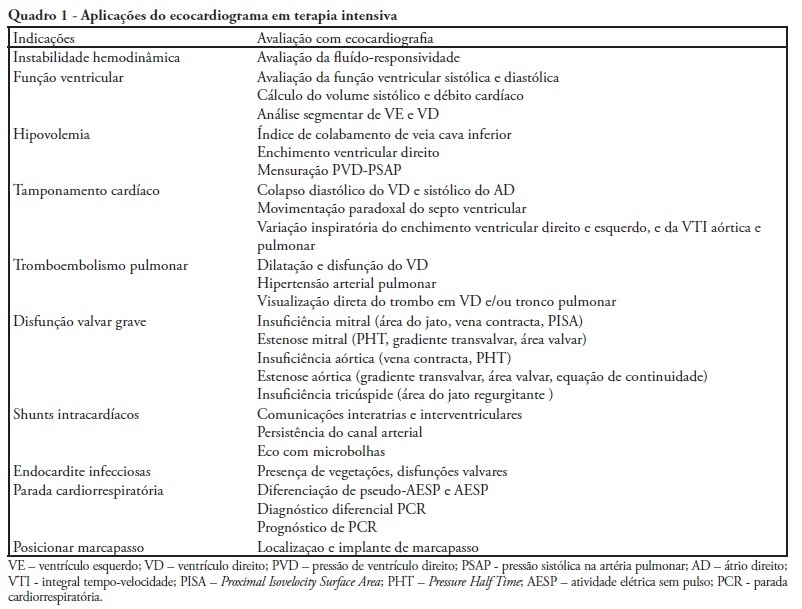
During the last few years, technological development and acquired experience advanced and the echocardiogram has become an important and useful tool in intensive care unit environment. Data obtained from semi quantitative Doppler echocardiography (transthoracic and transesophageal) evaluation has contributed to an appropriate patient monitoring and management. Echocardiography as a diagnostic, prognostic and monitoring method for fluid responsiveness assessment has become available nowadays since hand-carried ultrasound devices are portable and cheaper. Adequate training and development of appropriateness criteria for use of echocardiography in intensive care unit may lead to a standard use as a bedside tool.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):65-71
DOI 10.1590/S0103-507X2009000100010
Cardiac arrest survivors frequently suffer from ischemic brain injury associated with poor neurological outcome and death. Therapeutic hypothermia improves outcomes in comatose survivors after resuscitation from out-of-hospital cardiac arrest. Considering its formal recommendation as a therapy, post-return of spontaneous circulation after cardiac arrest, the objective of this study was to review the clinical aspects of therapeutic hypothermia. Non-systematic review of articles using the keywords "cardiac arrest, cardiopulmonary resuscitation, cooling, hypothermia, post resuscitation syndrome" in the Med-Line database was performed. References of these articles were also reviewed. Unconscious adult patients with spontaneous circulation after out-of-hospital ventricular fibrillation or pulseless ventricular tachycardia should be cooled. Moreover, for any other rhythm or in the intra-hospital scenario, such cooling may also be beneficial. There are different ways of promoting hypothermia. The cooling system should be adjusted as soon as possible to the target temperature. Mild therapeutic hypothermia should be administered under close control, using neuromuscular blocking drugs to avoid shivering. The rewarming process should be slow, and reach 36º C, usually in no less then 8 hours. When temperature increases to more than 35º C, sedation, analgesia, and paralysis could be discontinued. The expected complications of hypothermia may be pneumonia, sepsis, cardiac arrhythmias, and coagulopathy. In spite of potential complications which require rigorous control, only six patients need to be treated to save one life.