Abstract
Rev Bras Ter Intensiva. 2020;32(1):72-80
DOI 10.5935/0103-507X.20200012
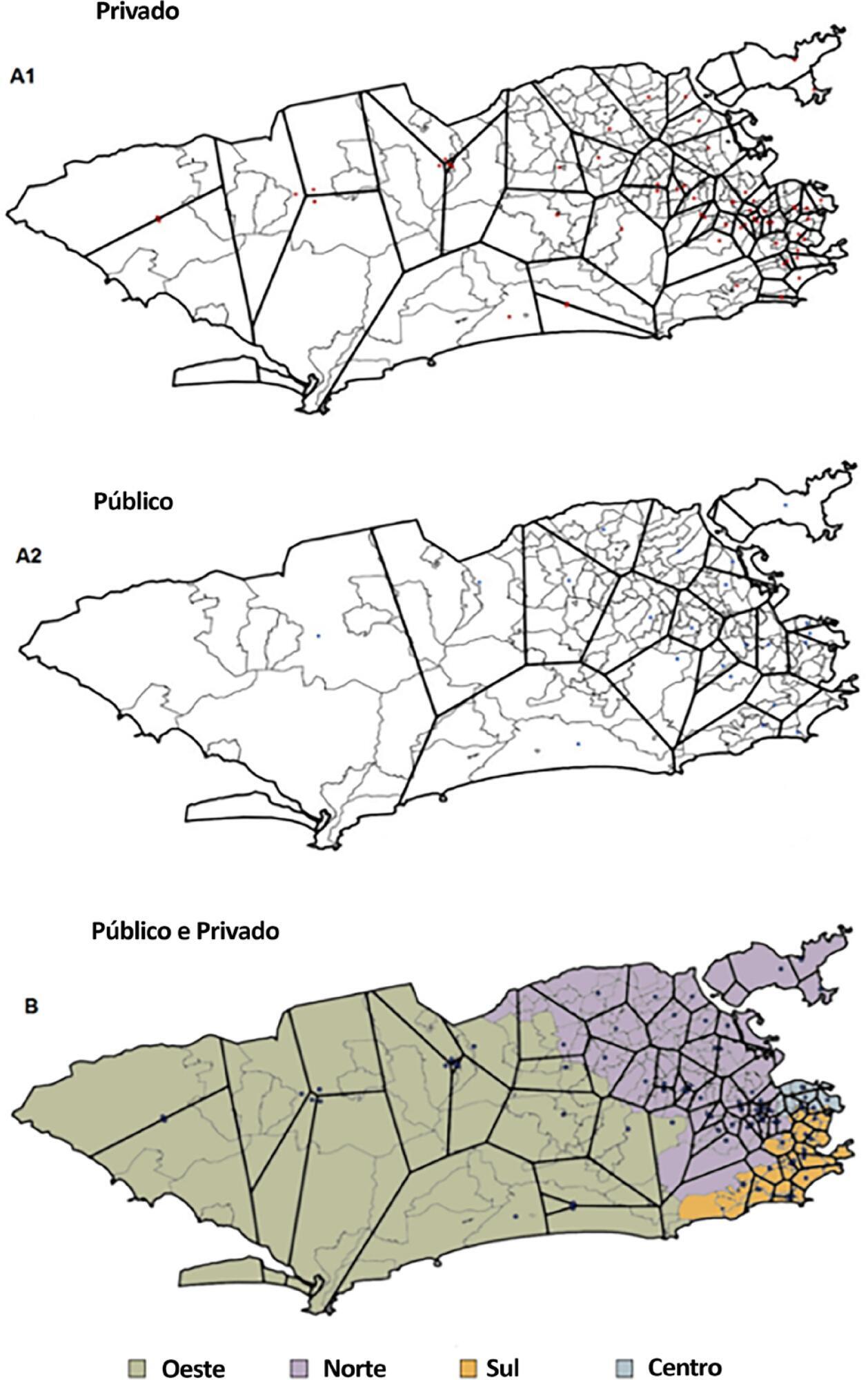
To analyze the distribution of adult intensive care units according to geographic region and health sector in Rio de Janeiro and to investigate severe acute respiratory infection mortality in the public sector and its association with critical care capacity in the public sector.
We evaluated the variation in intensive care availability and severe acute respiratory infection mortality in the public sector across different areas of the city in 2014. We utilized databases from the National Registry of Health Establishments, the Brazilian Institute of Geography and Statistics, the National Mortality Information System and the Hospital Admission Information System.
There is a wide range of intensive care unit beds per capita (from 4.0 intensive care unit beds per 100,000 people in public hospitals in the West Zone to 133.6 intensive care unit beds per 100,000 people in private hospitals in the Center Zone) in the city of Rio de Janeiro. The private sector accounts for almost 75% of the intensive care unit bed supply. The more developed areas of the city concentrate most of the intensive care unit services. Map-based spatial analysis shows a lack of intensive care unit beds in vast territorial extensions in the less developed regions of the city. There is an inverse correlation (r = -0.829; 95%CI -0.946 to -0.675) between public intensive care unit beds per capita in different health planning areas of the city and severe acute respiratory infection mortality in public hospitals.
Our results show a disproportionate intensive care unit bed provision across the city of Rio de Janeiro and the need for a rational distribution of intensive care.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):217-226
DOI 10.5935/0103-507X.20190036
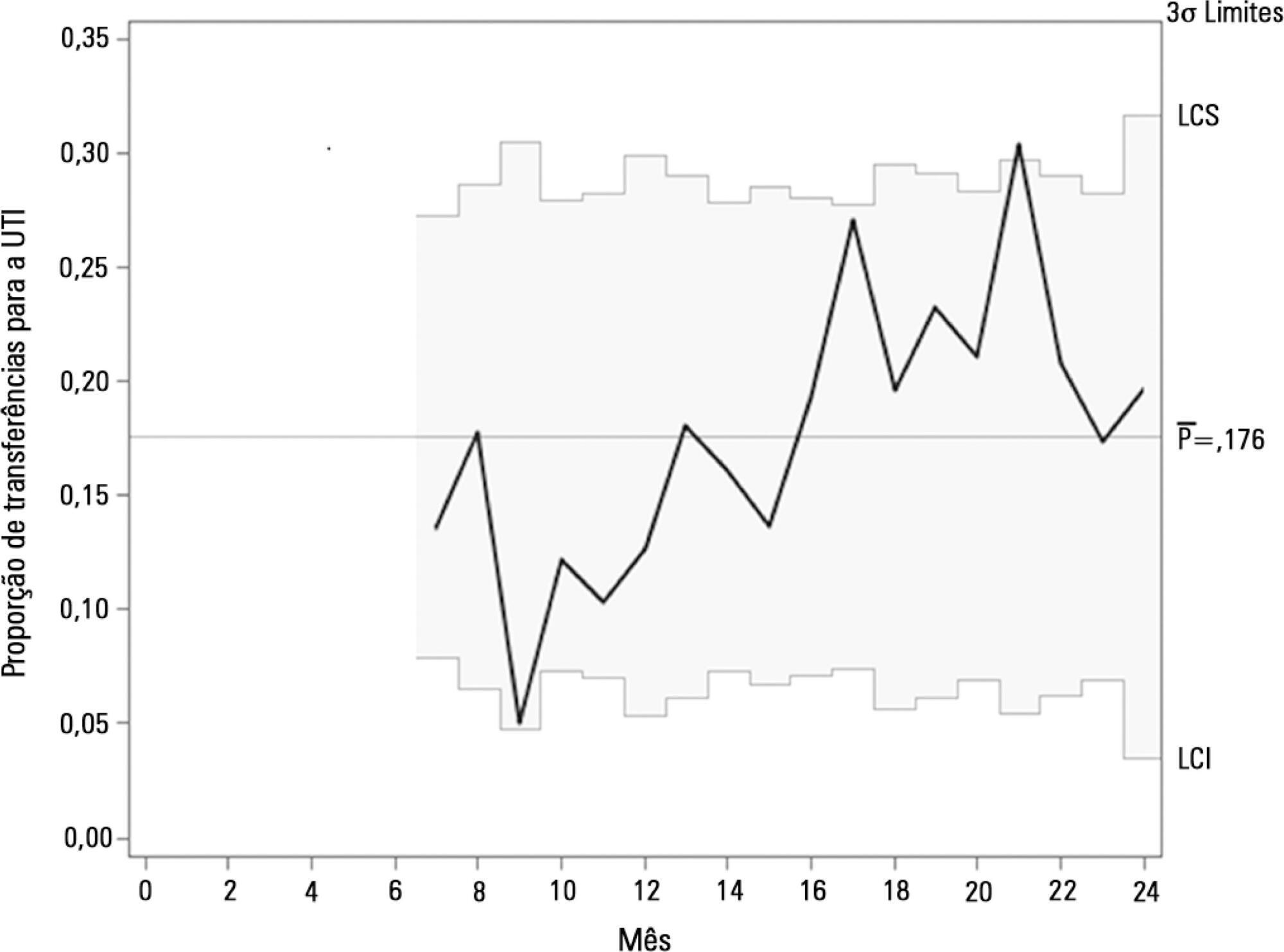
To describe the implementation of a rapid response team in a large nonprofit hospital, indicating relevant issues for other initiatives in similar contexts, particularly in Latin America.
In general terms, the intervention consisted of three major components: (1) a tool to detect aggravation of clinical conditions in general wards; (2) the structuring of a rapid response team to attend to all patients at risk; and (3) the monitoring of indicators regarding the intervention. This work employed four half-year Plan-Do-Study-Act cycles to test and adjust the intervention from January 2013 to December 2014.
Between 2013 and 2014, the rapid response team attended to 2,296 patients. This study showed a nonsignificant reduction in mortality from 8.3% in cycle 1 to 5.0% in cycle 4; however, death rates remained stable in cycles 3 and 4, with frequencies of 5.2% and 5.0%, respectively. Regarding patient flow and continuum of critical care, which is a premise of the rapid response system, there was a reduction in waiting time for intensive care unit beds with a decrease from 45.9% to 19.0% in the frequency of inpatients who could not be admitted immediately after indication (p < 0.001), representing improved patient flow in the hospital. In addition, an increase in the recognition of palliative care patients from 2.8% to 10.3% was noted (p = 0.005).
Implementing a rapid response team in contexts where there are structural restrictions, such as lack of intensive care unit beds, may be very beneficial, but a strategy of adjustment is needed.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):98-111
DOI 10.5935/0103-507X.20180016
The follow-up of patients who are discharged from intensive care units follows distinct flows in different parts of the world. Outpatient clinics or post-intensive care clinics represent one of the forms of follow-up, with more than 20 years of experience in some countries. Qualitative studies that followed up patients in these outpatient clinics suggest more encouraging results than quantitative studies, demonstrating improvements in intermediate outcomes, such as patient and family satisfaction. More important results, such as mortality and improvement in the quality of life of patients and their families, have not yet been demonstrated. In addition, which patients should be indicated for these outpatient clinics? How long should they be followed up? Can we expect an improvement of clinical outcomes in these followed-up patients? Are outpatient clinics cost-effective? These are only some of the questions that arise from this form of follow-up of the survivors of intensive care units. This article aims to review all aspects relating to the organization and performance of post-intensive care outpatient clinics and to provide an overview of studies that evaluated clinical outcomes related to this practice.
Abstract
Rev Bras Ter Intensiva. 2018;30(3):366-375
DOI 10.5935/0103-507X.20180049
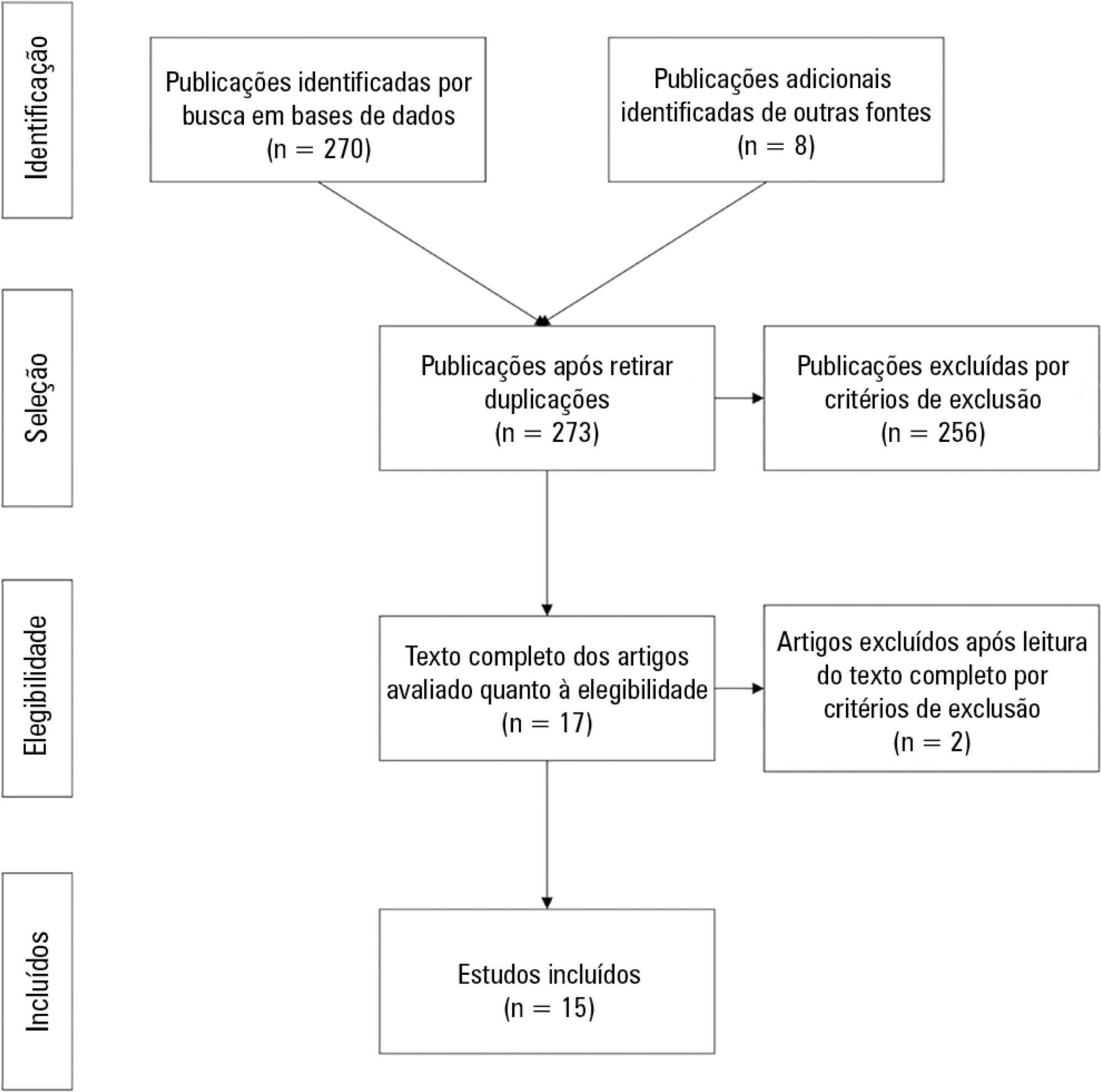
To evaluate the effectiveness of rapid response teams using early identification of clinical deterioration in reducing the occurrence of in-hospital mortality and cardiorespiratory arrest.
The MEDLINE, LILACS, Cochrane Library, Center for Reviews and Dissemination databases were searched.
We included studies that evaluated the effectiveness of rapid response teams in adult hospital units, published in English, Portuguese, or Spanish, from 2000 to 2016; systematic reviews, clinical trials, cohort studies, and prepost ecological studies were eligible for inclusion. The quality of studies was independently assessed by two researchers using the Newcastle-Ottawa, modified Jadad, and Assessment of Multiple Systematic Reviews scales.
The results were synthesized and tabulated. When risk measures were reported by the authors of the included studies, we estimated effectiveness as 1-RR or 1-OR. In pre-post studies, we estimated effectiveness as the percent decrease in rates following the intervention.
Overall, 278 studies were identified, 256 of which were excluded after abstract evaluation, and two of which were excluded after full text evaluation. In the meta-analysis of the studies reporting mortality data, we calculated a risk ratio of 0.85 (95%CI 0.76 - 0.94); and for studies reporting cardiac arrest data the estimated risk ratio was 0.65 (95%CI 0.49 - 0.87). Evidence was assessed as low quality due to the high heterogeneity and risk of bias in primary studies.
We conclude that rapid response teams may reduce in-hospital mortality and cardiac arrests, although the quality of evidence for both outcomes is low.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):188-194
DOI 10.5935/0103-507X.20170018
This study aims to identify the satisfaction levels of the family members of patients in intensive care units.
This is a cross-sectional analytical study. General intensive care units offer a variety of services to clinical and surgical patients. For the purpose of this study, a trained interviewer communicated with the families of patients, either before or after visiting hours.
The study included 208 participants: 119 (57.2%) males and 89 (42.8%) females. Seventy-three (35.1%) of the patients attended a private hospital, and 135 (64.9%) attended a public hospital in the city of Al Madinah Al- Munawarah. All of the participants were either family members or friends of patients admitted to the intensive care units at the hospitals. The responses of both groups yielded low scores on the satisfaction index. However, a relatively high score was noted in response to questions 2, 6, and 10, which concerned the care that was extended by the hospital staff to their patients, the courteous attitude of intensive care unit staff members towards patients, and patients' satisfaction with the medical care provided, respectively. A very low score was obtained for item 11, which was related to the possibility for improvements to the medical care that the patients received. Overall, greater satisfaction with the services offered by the public intensive care units was reported compared to the satisfaction with the services offered by the private intensive care units.
An overall low score on the satisfaction index was obtained, and further studies are recommended to assess the current situation and improve the satisfaction and quality of care provided by intensive care units.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):32-38
DOI 10.1590/S0103-507X2013000100007
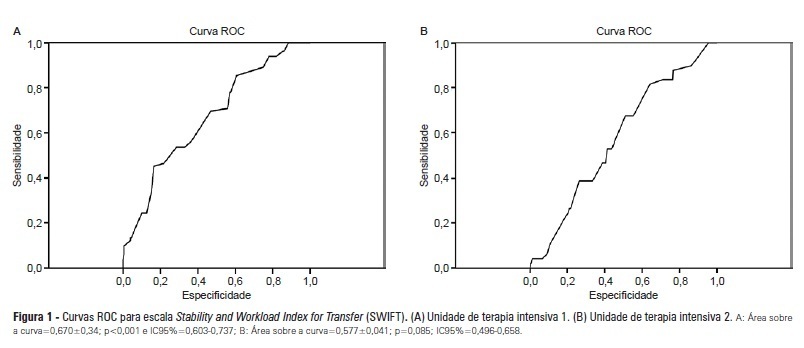
OBJECTIVES: Identify patients at risk for intensive care unit readmission, the reasons for and rates of readmission, and mortality after their stay in the intensive care unit; describe the sensitivity and specificity of the Stability and Workload Index for Transfer scale as a criterion for discharge from the intensive care unit. METHODS: Adult, critical patients from intensive care units from two public hospitals in Porto Alegre, Brazil, comprised the sample. The patients' clinical and demographic characteristics were collected within 24 hours of admission. They were monitored until their final outcome on the intensive care unit (death or discharge) to apply the Stability and Workload Index for Transfer. The deaths during the first intensive care unit admission were disregarded, and we continued monitoring the other patients using the hospitals' electronic systems to identify the discharges, deaths, and readmissions. RESULTS: Readmission rates were 13.7% in intensive care unit 1 (medical-surgical, ICU1) and 9.3% in intensive care unit 2 (trauma and neurosurgery, ICU2). The death rate following discharge was 12.5% from ICU1 and 4.2% from ICU2. There was a statistically significant difference in Stability and Workload Index for Transfer (p<0.05) regarding the ICU1 patients' outcome, which was not found in the ICU2 patients. In ICU1, 46.5% (N=20) of patients were readmitted very early (within 48 hours of discharge). Mortality was high among those readmitted: 69.7% in ICU1 and 48.5% in ICU2. CONCLUSIONS: The Stability and Workload Index for Transfer scale showed greater efficacy in identifying patients more prone to readmission and death following discharge from a medical-surgical intensive care unit. The patients' intensive care unit readmission during the same hospitalization resulted in increased morbidity, mortality, length of stay, and total costs.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):353-358
DOI 10.1590/S0103-507X2009000400004
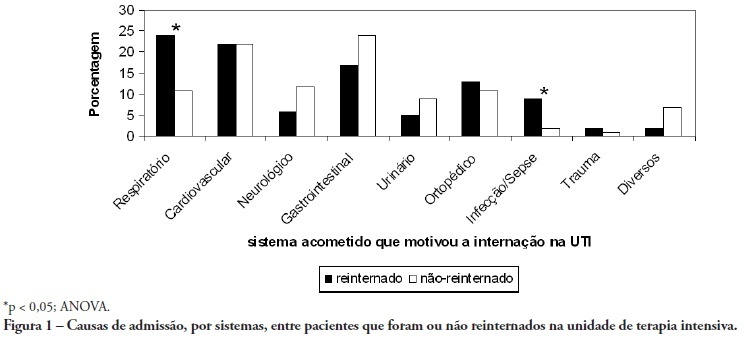
OBJECTIVE: To predict readmission in intensive care unit analyzing the first 24 hours data after intensive care unit admission. METHODS: The first intensive care unit admission of patients was analyzed from January to May 2009 in a mixed unit. Readmission to the unit was considered those during the same hospital stay or within 3 months after intensive care unit discharge. Deaths during the first admission were excluded. Demographic data, use of mechanical ventilation, and report of stay longer than 3 days were submitted to uni and multivariate analysis for readmission. RESULTS: Five hundred seventy-seven patients were included (33 excluded deaths). The readmission group had 59 patients, while 518 patients were not readmitted. The lead time between the index admission and readmission was 9 (3-28) days (18 were readmitted in less than 3 days), and 10 died. Patients readmitted at least once to the intensive care unit had the differences below in comparison to the control group: older age: 75 (67-81) versus 67 (56-78) years, P<0.01; admission for respiratory insufficiency or sepsis: 33 versus 13%, P<0.01; medical admission: 49 versus 32%, P<0.05; higher SAPS II score: 27 (21-35) versus 23 (18-29) points, P<0.01; Charlson index: 2 (1-2) versus 1 (0-2) points, P<0.01; first ICU stay longer than 3 days: 35 versus 23%, P<0.01. After logistic regression, higher age, Charlson index and admission for respiratory and sepsis were independently associated to readmissions in intensive care unit. CONCLUSION: Age, comorbidities and respiratory- and/or sepsis-related admission are associated with increased readmission risk in the studied sample.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)