Abstract
Crit Care Sci. 2023;35(4):345-354
DOI 10.5935/2965-2774.20230162-pt
The optimal target for blood glucose concentration in critically ill patients is unclear. We will perform a systematic review and meta-analysis with aggregated and individual patient data from randomized controlled trials, comparing intensive glucose control with liberal glucose control in critically ill adults.
MEDLINE®, Embase, the Cochrane Central Register of Clinical Trials, and clinical trials registries (World Health Organization, clinical trials.gov). The authors of eligible trials will be invited to provide individual patient data. Published trial-level data from eligible trials that are not at high risk of bias will be included in an aggregated data meta-analysis if individual patient data are not available.
Inclusion criteria: randomized controlled trials that recruited adult patients, targeting a blood glucose of ≤ 120mg/dL (≤ 6.6mmol/L) compared to a higher blood glucose concentration target using intravenous insulin in both groups. Excluded studies: those with an upper limit blood glucose target in the intervention group of > 120mg/dL (> 6.6mmol/L), or where intensive glucose control was only performed in the intraoperative period, and those where loss to follow-up exceeded 10% by hospital discharge.
In-hospital mortality during index hospital admission. Secondary endpoints: mortality and survival at other timepoints, duration of invasive mechanical ventilation, vasoactive agents, and renal replacement therapy. A random effect Bayesian meta-analysis and hierarchical Bayesian models for individual patient data will be used.
This systematic review with aggregate and individual patient data will address the clinical question, ‘what is the best blood glucose target for critically ill patients overall?’
Abstract
Crit Care Sci. 2023;35(2):147-155
DOI 10.5935/2965-2774.20230422-pt
To assess factors associated with long-term neuropsychiatric outcomes, including biomarkers measured after discharge from the intensive care unit.
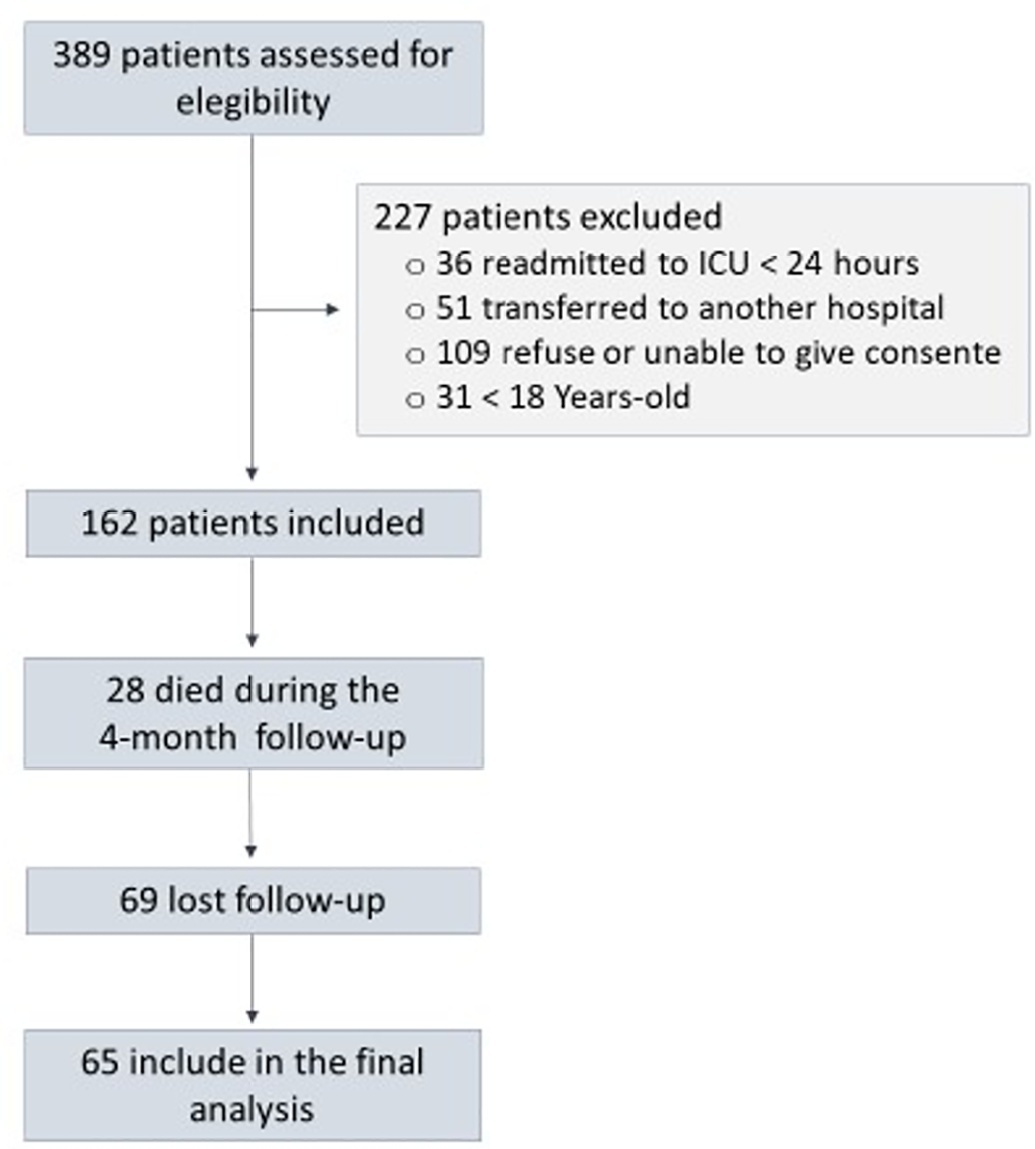
A prospective cohort study was performed with 65 intensive care unit survivors. The cognitive evaluation was performed through the Mini-Mental State Examination, the symptoms of anxiety and depression were evaluated using the Hospital Anxiety and Depression Scale, and posttraumatic stress disorder was evaluated using the Impact of Event Scale-6. Plasma levels of amyloid-beta (1-42) [Aβ (1-42)], Aβ (1-40), interleukin (IL)-10, IL-6, IL-33, IL-4, IL-5, tumor necrosis factor alpha, C-reactive protein, and brain-derived neurotrophic factor were measured at intensive care unit discharge.
Of the variables associated with intensive care, only delirium was independently related to the occurrence of long-term cognitive impairment. In addition, higher levels of IL-10 and IL-6 were associated with cognitive dysfunction. Only IL-6 was independently associated with depression. Mechanical ventilation, IL-33 levels, and C-reactive protein levels were independently associated with anxiety. No variables were independently associated with posttraumatic stress disorder.
Cognitive dysfunction, as well as symptoms of depression, anxiety, and posttraumatic stress disorder, are present in patients who survive a critical illness, and some of these outcomes are associated with the levels of inflammatory biomarkers measured at discharge from the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2022;34(1):141-146
DOI 10.5935/0103-507X.20220008-en
To assess early postdischarge health-related quality of life and disability of all survivors of critical COVID-19 admitted for more than 24 hours to na intensive care unit..
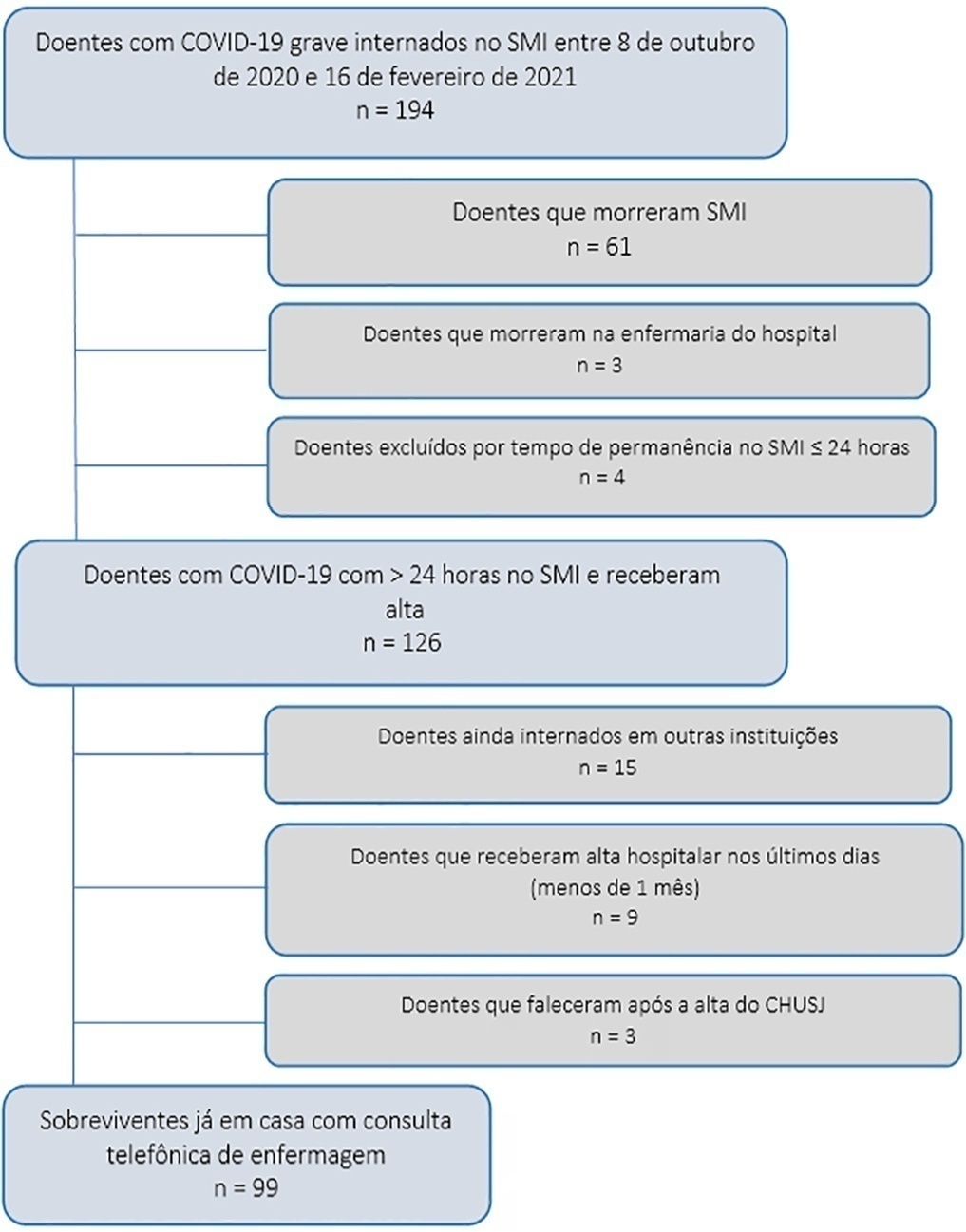
Study carried out at the Intensive Care Medicine Department of Centro Hospitalar Universitário São João from 8th October 2020 to 16th February 2021. Approximately 1 month after hospital discharge, an intensive care-trained nurse performed a telephone consultation with 99 survivors already at home applying the EuroQol Five-Dimensional Five-Level questionnaire and the 12-item World Health Organization Disability Assessment Schedule 2.0.
The mean age of the population studied was 63 ± 12 years, and 32.5% were submitted to invasive mechanical ventilation. Their mean Simplified Acute Physiologic Score was 35 ± 14, and the Charlson Comorbidity Index was 3 ± 2. Intensive care medicine and hospital lengths of stay were 13 ± 22 and 22 ± 25 days, respectively. The mean EuroQol Visual Analog Scale was 65% (± 21), and only 35.3% had no or slight problems performing their usual activities, most having some degree of pain/discomfort and anxiety/depression. The 12-item World Health Organization Disability Assessment Schedule 2.0 showed marked impairments in terms of reassuring usual work or community activities and mobility. The use of both tools suggested that their health status was worse than their perception of it.
This early identification of sequelae may help define flows and priorities for rehabilitation and reinsertion after critical COVID-19.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):426-432
DOI 10.5935/0103-507X.20200072
To evaluate the association between the incidence of delirium in the intensive care unit and quality of life 1 month after hospital discharge.
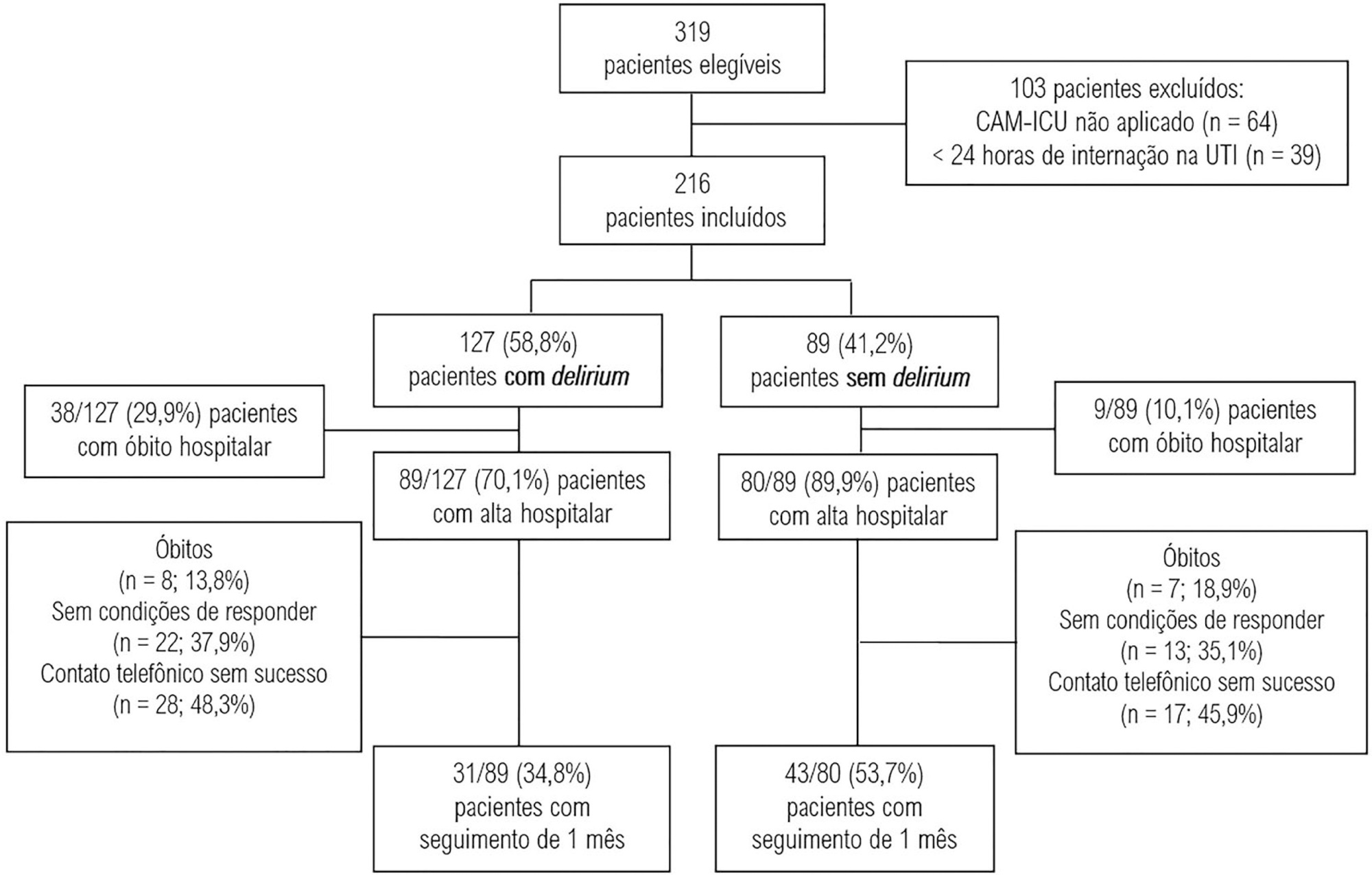
This was a prospective cohort study conducted in the intensive care units of two medium-complexity hospitals from December 2015 to December 2016. Delirium was identified using the Confusion Assessment Method for the Intensive Care Unit scale. At the time of hospital discharge, functional capacity and cognition were assessed with the Barthel index and the Mini Mental State Examination, respectively. Thirty days after patient discharge, the World Health Organization Quality of Life-BREF questionnaire was administered by telephone.
A total of 216 patients were included. Delirium was identified in 127 (58.8%) of them. Patients with delirium exhibited greater functional dependence (median Barthel index 50.0 [21.2 - 70.0] versus 80.0 [60.0 - 95.0]; p < 0.001) and lower cognition (Mini Mental State Examination score 12.9 ± 7.5 versus 20.7 ± 9.8; p < 0.001) at hospital discharge. There was no difference in any of the quality-of-life domains evaluated 1 month after hospital discharge between patients with and without delirium.
Our findings suggest that patients with delirium in the intensive care unit do not have worse quality of life 1 month after hospital discharge, despite presenting greater cognitive impairment and functional disability at the time of hospital discharge.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):529-535
DOI 10.5935/0103-507X.20190066
To measure and compare the functionality of patients after discharge from the intensive care unit and at the time of hospital discharge.
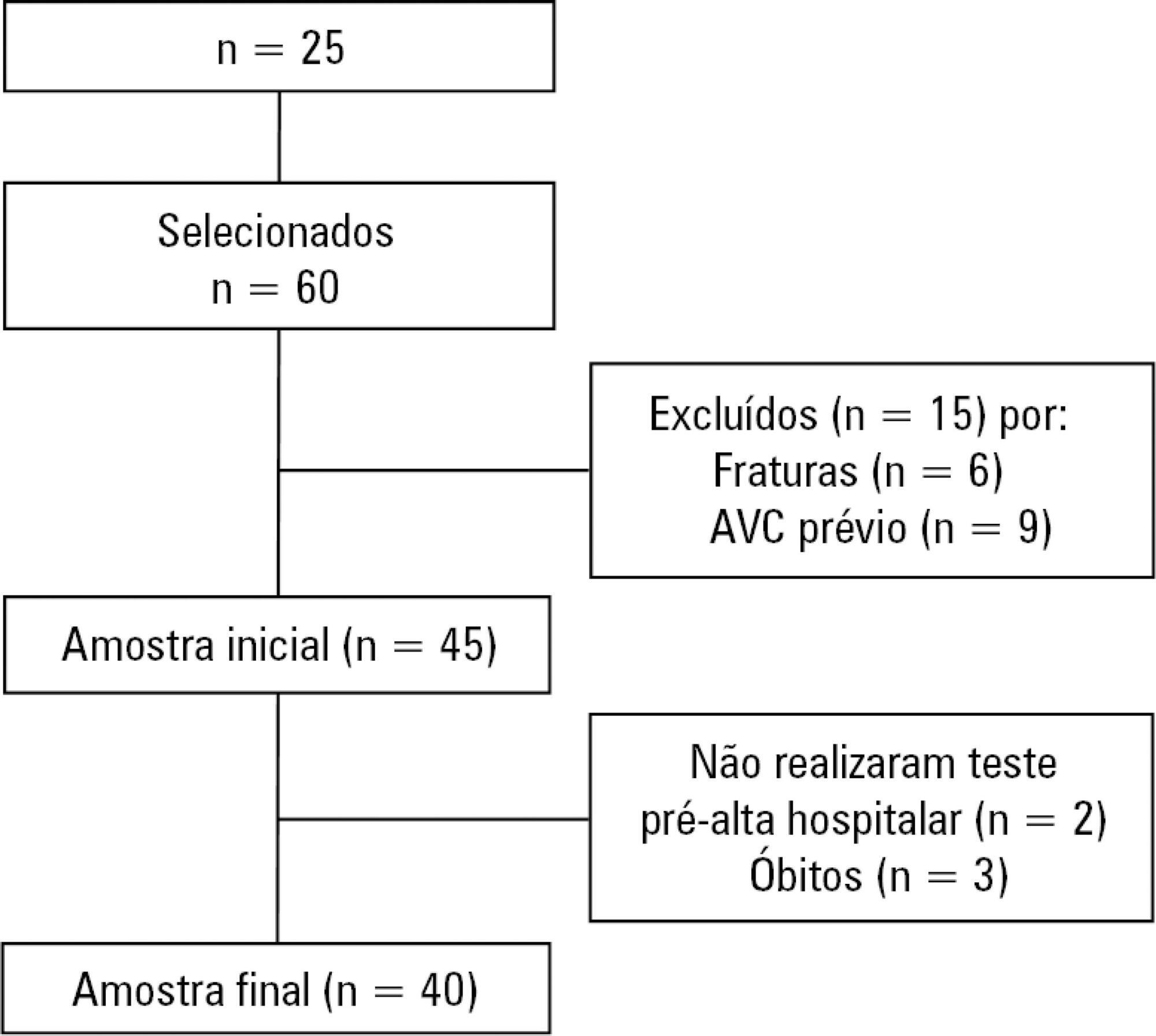
Quantitative study of a prospective cohort performed between August of 2016 and December of 2017 at a university hospital. A 10-meter walk test was performed at 2 timepoints: after discharge from the intensive care unit and prior to hospital discharge. The data were analyzed using Student's t-test and Pearson or Spearman correlation. Statistical Package for Social Science (SPSS) version 21.0 was used for the analysis, and p ≤ 0.05 was adopted as the level of significance.
Forty patients, with a mean age of 57.1 ± 12.2 years and with a predominance of males (60%), were evaluated. For the post-intensive care unit test, a mean speed of 0.48m/s was observed, and for the pre-hospital discharge test, there was an increase to 0.71m/s, evidencing functional evolution during the hospital stay (p < 0.001).
There was significant improvement in walking speed at the time of hospital discharge when compared to the walking speed at the time of intensive care unit discharge.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):27-33
DOI 10.5935/0103-507X.20190006
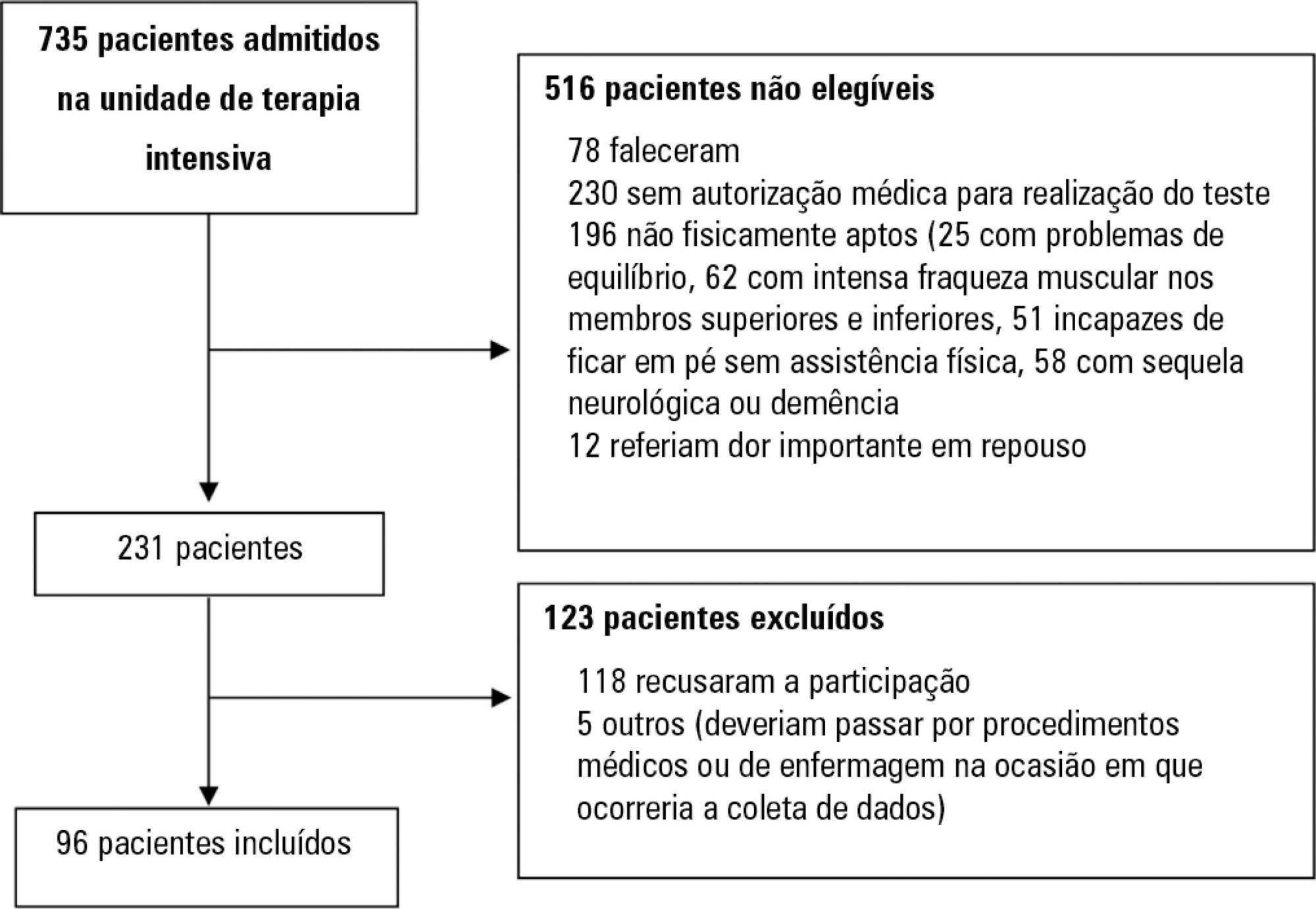
Assess the Five Times Sit-to-Stand Test safety and clinimetric properties in older patients hospitalized in an intensive care unit.
Test safety was assessed according to the incidence of adverse events and through hemodynamic and respiratory data. Additionally, reliability properties were investigated using the intraclass correlation coefficients, standard error of measurement, standard error percentage change, Altman-Bland plot and a survival agreement plot.
The overall suitability of the Five Times Sit-to-Stand Test was found to be low, with 29.8% meeting the inclusion criteria. Only 44% of the hospitalized patients who met the inclusion criteria performed the test, with no need for discontinuation in any patient. Heart rate (79.7 ± 10.2bpm/86.6 ± 9.7bpm; p = 0.001) and systolic blood pressure (118 ± 21.4mmHg/129 ± 21.5mmHg; p = 0.031) were the only variables that presented a significant statistical increase, with no evidence of exacerbated response to the test. Additionally, no adverse events were reported from participating and both test-retest and interrater reliability were high (intraclass correlation coefficient ≥ 0.99).
The Five Times Sit-to-Stand Test was proven to be safe and to have excellent reliability. Its clinical use, however, may be restricted to high-functioning older adults in hospital settings.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):28-34
DOI 10.5935/0103-507X.20180008
To investigate the longterm psychological outcome in survivors of critical illness after intensive care unit discharge.
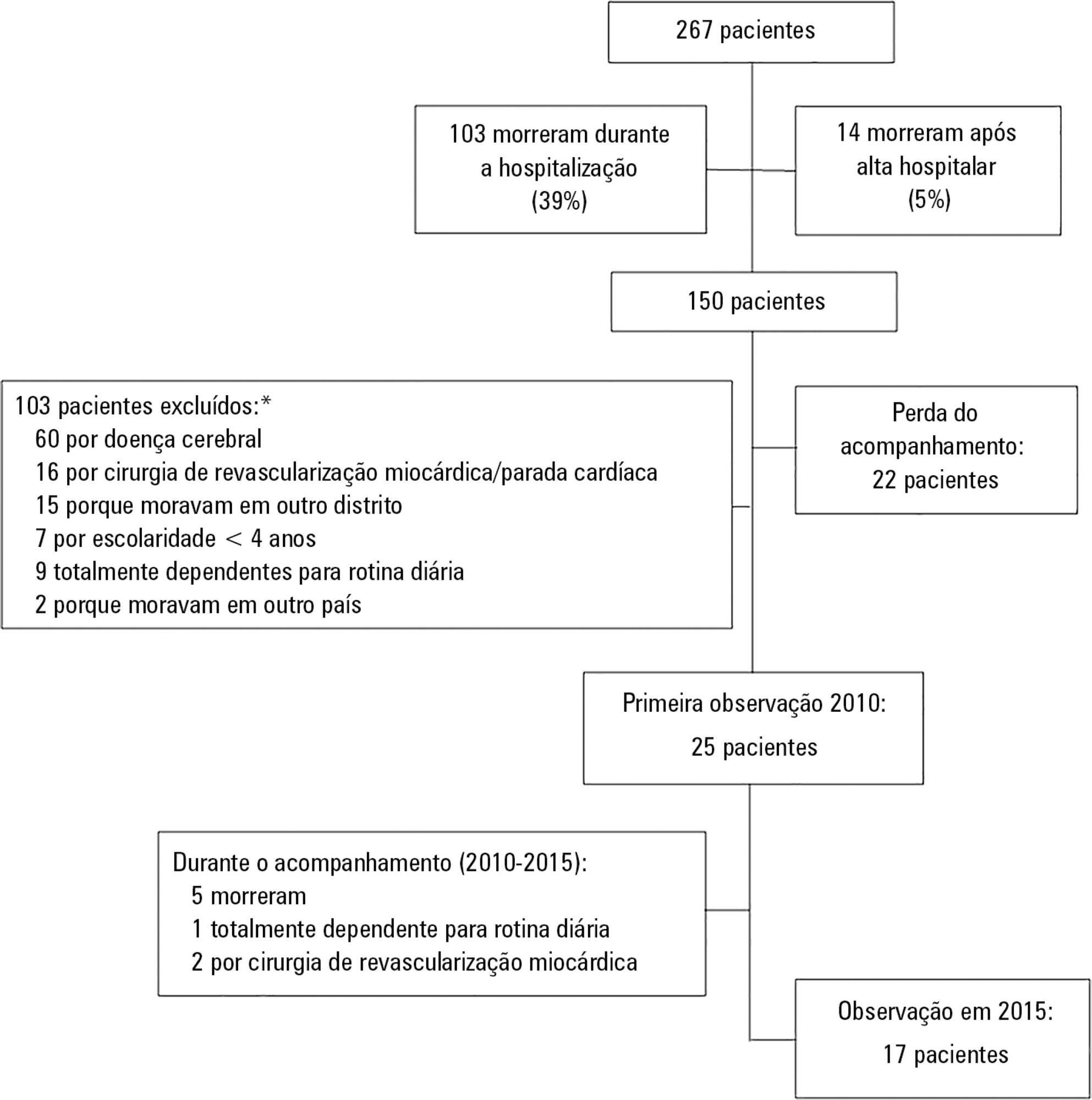
A prospective cohort of survivors admitted to a mixed intensive care unit between January and September 2010 was evaluated six months and five years after hospital discharge. The Dementia Rating Scale-2, the Hospital Anxiety and Depression Scale, the Posttraumatic stress syndrome 14-questions inventory, the Euro Quality of Life 5 Dimensions (EQ-5-D), and the Visual Analogue Scale (EQ VAS) were assessed at both follow-up periods.
Of 267 patients, 25 patients were evaluated at 6 months after discharge (62 ± 16 years); 12 (48%) presented cognitive impairment, 6 (24%) anxiety, 4 (16%) depression, and 4 (16%) post-traumatic stress disorder. Among those re-evaluated five years after discharge (n = 17; 65 ± 15 years), the frequency of cognitive impairment dropped from 8 (47%) to 3 (18%) (p = 0.063), due to improvement in these patients over time, and other patients did not acquire any dysfunction after discharge. At five years after discharge, only two patients (12%) reported anxiety, and none had depression or post-traumatic stress disorder. No differences were found between the six-month and five-year follow-ups regarding EQ-5-D and EQ VAS.
Survivors do not show a progressive decline in cognitive function or quality of life within five years after intensive care unit discharge. Psychopathological symptoms tend to decrease with time.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)