You searched for:"Djillali Annane"
We found (2) results for your search.-
Special Article
Intensive glucose control in critically ill adults: a protocol for a systematic review and individual patient data meta-analysis
Crit Care Sci. 2023;35(4):345-354
Abstract
Special ArticleIntensive glucose control in critically ill adults: a protocol for a systematic review and individual patient data meta-analysis
Crit Care Sci. 2023;35(4):345-354
DOI 10.5935/2965-2774.20230162-pt
Views19ABSTRACT
Objective:
The optimal target for blood glucose concentration in critically ill patients is unclear. We will perform a systematic review and meta-analysis with aggregated and individual patient data from randomized controlled trials, comparing intensive glucose control with liberal glucose control in critically ill adults.
Data sources:
MEDLINE®, Embase, the Cochrane Central Register of Clinical Trials, and clinical trials registries (World Health Organization, clinical trials.gov). The authors of eligible trials will be invited to provide individual patient data. Published trial-level data from eligible trials that are not at high risk of bias will be included in an aggregated data meta-analysis if individual patient data are not available.
Methods:
Inclusion criteria: randomized controlled trials that recruited adult patients, targeting a blood glucose of ≤ 120mg/dL (≤ 6.6mmol/L) compared to a higher blood glucose concentration target using intravenous insulin in both groups. Excluded studies: those with an upper limit blood glucose target in the intervention group of > 120mg/dL (> 6.6mmol/L), or where intensive glucose control was only performed in the intraoperative period, and those where loss to follow-up exceeded 10% by hospital discharge.
Primary endpoint:
In-hospital mortality during index hospital admission. Secondary endpoints: mortality and survival at other timepoints, duration of invasive mechanical ventilation, vasoactive agents, and renal replacement therapy. A random effect Bayesian meta-analysis and hierarchical Bayesian models for individual patient data will be used.
Discussion:
This systematic review with aggregate and individual patient data will address the clinical question, ‘what is the best blood glucose target for critically ill patients overall?’
Keywords:Blood glucoseCritical illnessGlycemic controlinsulinIntraoperative periodMortalityPatient dischargeRegistriesSee more -
Adrenal insufficiency in sepsis
Rev Bras Ter Intensiva. 2006;18(1):86-94
Abstract
Adrenal insufficiency in sepsis
Rev Bras Ter Intensiva. 2006;18(1):86-94
DOI 10.1590/S0103-507X2006000100014
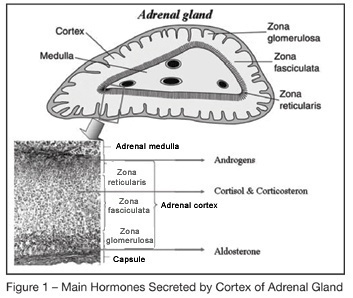
Views0See moreBACKGROUND AND OBJECTIVES: Corticosteroids were introduced in the treatment of severe infection as early as in the nineteen forties. Several ” negative” randomized controlled trials of high-dose of glucocorticoids given for a short period of time in the early course of severe sepsis or acute respiratory distress syndrome raised serious doubts on the benefit of this treatment. Recently, a link between septic shock and adrenal insufficiency, or systemic inflammation induced glucocorticoids receptor resistance had been established. This finding prompted renewed interest of a replacement therapy with low doses of corticosteroids during longer periods. The goal of this article is to review the key role of corticosteroids in the host response to stress and will update the reader with the new validated indications of corticosteroids treatment in the ICU. CONTENTS: Extensive review of the adrenal physiology and its pathophysiological derangements and clinical implications in critically ill patients. CONCLUSIONS: During sepsis, hemodynamic instability and perpetuation of inflammatory state may result from adrenal insufficiency (AI). Thus, an ACTH test should be performed as soon as possible to identify non overt AI. It should be immediately followed by a replacement therapy with iv bolus of 50 mg of hydrocortisone every 6 hours combined to 50 µg of fludrocortisone once daily. When the results of the ACTH test are available, treatment should be continued for 7 days in the non responders to ACTH and withdraw in the responders. Whether responders to ACTH with high baseline cortisol levels (> 34 µg/dL) have tissue resistance to cortisol and also should receive exogenous hormones remains to be evaluated in clinical trials.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




