Abstract
Crit Care Sci. 2023;35(4):345-354
DOI 10.5935/2965-2774.20230162-pt
The optimal target for blood glucose concentration in critically ill patients is unclear. We will perform a systematic review and meta-analysis with aggregated and individual patient data from randomized controlled trials, comparing intensive glucose control with liberal glucose control in critically ill adults.
MEDLINE®, Embase, the Cochrane Central Register of Clinical Trials, and clinical trials registries (World Health Organization, clinical trials.gov). The authors of eligible trials will be invited to provide individual patient data. Published trial-level data from eligible trials that are not at high risk of bias will be included in an aggregated data meta-analysis if individual patient data are not available.
Inclusion criteria: randomized controlled trials that recruited adult patients, targeting a blood glucose of ≤ 120mg/dL (≤ 6.6mmol/L) compared to a higher blood glucose concentration target using intravenous insulin in both groups. Excluded studies: those with an upper limit blood glucose target in the intervention group of > 120mg/dL (> 6.6mmol/L), or where intensive glucose control was only performed in the intraoperative period, and those where loss to follow-up exceeded 10% by hospital discharge.
In-hospital mortality during index hospital admission. Secondary endpoints: mortality and survival at other timepoints, duration of invasive mechanical ventilation, vasoactive agents, and renal replacement therapy. A random effect Bayesian meta-analysis and hierarchical Bayesian models for individual patient data will be used.
This systematic review with aggregate and individual patient data will address the clinical question, ‘what is the best blood glucose target for critically ill patients overall?’
Abstract
Rev Bras Ter Intensiva. 2010;22(3):229-235
DOI 10.1590/S0103-507X2010000300003
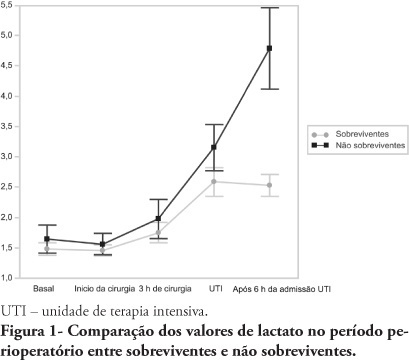
OBJECTIVES: An increased lactate level is classically considered a marker for poorer prognosis, however little information is available on intraoperative lactate's kinetics and its connection with prognosis. This study aimed to evaluate the time when perioperative lactate is most relevant for prognosis. METHODS: This was an observational prospective study conducted in a tertiary hospital. Patients with requested intensive care unit postoperative stay, aged > 18 years, undergoing major surgery were included. Palliative surgery patients and those with heart and/or severe liver failure were excluded. Arterial lactate levels were measured immediately before the surgery start (T0), after anesthesia induction (T1), 3 hours after the surgery start (T2), intensive care unit admission (T3) and 6 hours after the intensive care unit admission (T4). RESULTS: Sixty seven patients were included. The mean lactate values for the patients' T0, T1, T2 and T4 were 1.5 ± 0.8 mmol/L, 1.5 ± 0.7 mmol/L, 1.8 ± 1.2 mmol/L, 2.7 ± 1.7 mmol/L and 3.1 ± 2.0 mmol/L, respectively. The hospital mortality rate was 25.8%, and surviving and non-surviving patients lactate values in the intensive care unit were 2.5 ± 1. and 4.8 ± 2.8 mmol/L (P < 0.0001), respectively. The other times measurements showed no statistically significant differences between the groups. CONCLUSIONS: In surgical patients, intraoperative arterial lactate levels failed to show a predictive value; however during the postoperative period, this assessment was shown to be useful for hospital mortality prediction.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)