Abstract
Rev Bras Ter Intensiva. 2015;27(4):340-346
DOI 10.5935/0103-507X.20150058
The purpose of this study was to test if venous blood drawn from femoral access can be used to estimate the central venous oxygen saturation and arterial lactate levels in critically ill patients.
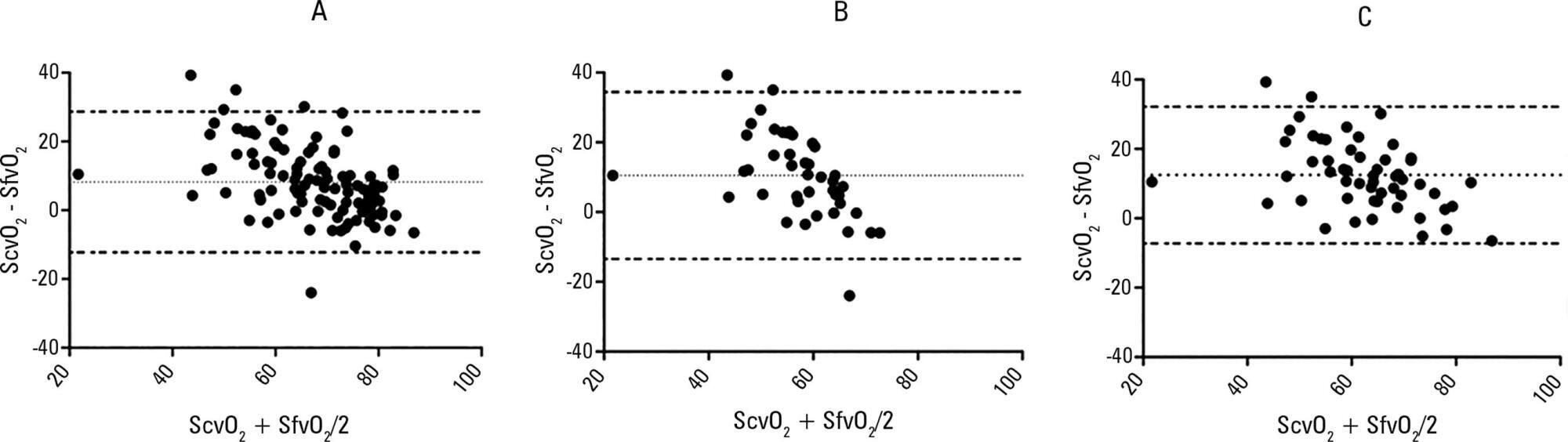
Bland-Altman analysis and Spearman correlations were used to compare the femoral venous oxygen saturation and central venous oxygen saturation as well as arterial lactate levels and femoral lactate. A pre-specified subgroup analysis was conducted in patients with signs of hypoperfusion. In addition, the clinical agreement was also investigated.
Blood samples were obtained in 26 patients. In 107 paired samples, there was a moderate correlation (r = 0.686, p < 0.0001) between the central venous oxygen saturation and femoral venous oxygen saturation with a bias of 8.24 ± 10.44 (95% limits of agreement: -12.23 to 28.70). In 102 paired samples, there was a strong correlation between the arterial lactate levels and femoral lactate levels (r = 0.972, p < 0.001) with a bias of -2.71 ± 9.86 (95% limits of agreement: -22.03 to 16.61). The presence of hypoperfusion did not significantly change these results. The clinical agreement for venous saturation was inadequate, with different therapeutic decisions in 22.4% of the situation; for lactate, this was the case only in 5.2% of the situations.
Femoral venous oxygen saturation should not be used as a surrogate of central venous oxygen saturation. However, femoral lactate levels can be used in clinical practice, albeit with caution.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):283-290
DOI 10.1590/S0103-507X2011000300005
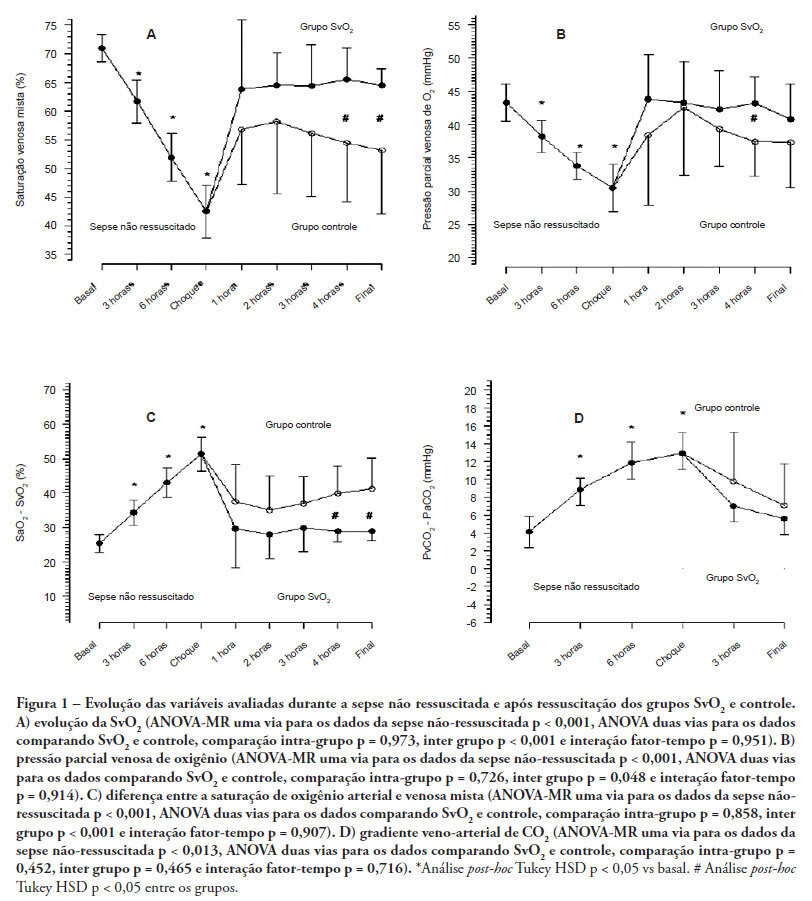
OBJECTIVES: Although fluid resuscitation guided by central venous oxygen saturation (SvcO2) is currently considered the gold standard in sepsis therapy, few studies have described hemodynamic and perfusion parameters during this procedure. This study aims to describe these parameters during septic shock without resuscitation and after 12 hours of goal-directed resuscitation. METHODS: Thirteen anesthetized pigs (35-45 kg) had peritonitis caused by fecal inoculation (0.75 g/kg). After developing persistent hypotension, both groups were given antibiotics and randomized either to the control group (n=7) or the experimental group (n=6). In the control group, hemodynamic control was optimized to maintain a central venous pressure of 8-12 mmHg, a urinary output above 0.5 mL/kg/hour and a mean arterial blood pressure above 65 mmHg. The experimental group received the above target therapy in addition to maintaining a SvO2 above 65%. The interventions included lactated Ringer's solution and norepinephrine for both groups and dobutamine in the SvO2 group. The animals were treated for 12 hours or until death. RESULTS: Untreated sepsis was associated with significant reductions in SvO2, PvO2, cardiac output and central venous pressure in addition to increased arteriovenous oxygen saturation and veno-arterial CO2 differences. Following resuscitation, these parameters were corrected in both groups. Goal-directed resuscitation was associated with a better hemodynamic profile, characterized by higher SvO2, cardiac output and central venous pressure. CONCLUSIONS: Non-resuscitated sepsis showed a hemodynamic profile suggesting hypovolemia, with worsened perfusion and hemodynamics, which is reversed upon fluid resuscitation. Goal-directed resuscitation is associated with significantly improved hemodynamic and perfusion parameters
Abstract
Rev Bras Ter Intensiva. 2010;22(3):229-235
DOI 10.1590/S0103-507X2010000300003
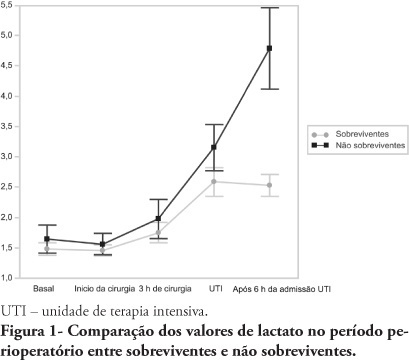
OBJECTIVES: An increased lactate level is classically considered a marker for poorer prognosis, however little information is available on intraoperative lactate's kinetics and its connection with prognosis. This study aimed to evaluate the time when perioperative lactate is most relevant for prognosis. METHODS: This was an observational prospective study conducted in a tertiary hospital. Patients with requested intensive care unit postoperative stay, aged > 18 years, undergoing major surgery were included. Palliative surgery patients and those with heart and/or severe liver failure were excluded. Arterial lactate levels were measured immediately before the surgery start (T0), after anesthesia induction (T1), 3 hours after the surgery start (T2), intensive care unit admission (T3) and 6 hours after the intensive care unit admission (T4). RESULTS: Sixty seven patients were included. The mean lactate values for the patients' T0, T1, T2 and T4 were 1.5 ± 0.8 mmol/L, 1.5 ± 0.7 mmol/L, 1.8 ± 1.2 mmol/L, 2.7 ± 1.7 mmol/L and 3.1 ± 2.0 mmol/L, respectively. The hospital mortality rate was 25.8%, and surviving and non-surviving patients lactate values in the intensive care unit were 2.5 ± 1. and 4.8 ± 2.8 mmol/L (P < 0.0001), respectively. The other times measurements showed no statistically significant differences between the groups. CONCLUSIONS: In surgical patients, intraoperative arterial lactate levels failed to show a predictive value; however during the postoperative period, this assessment was shown to be useful for hospital mortality prediction.