Abstract
Rev Bras Ter Intensiva. 2022;34(3):351-359
DOI 10.5935/0103-507X.20220383-en
To develop a simple, robust, safe and efficient invasive mechanical ventilator that can be used in remote areas of the world or war zones where the practical utility of more sophisticated equipment is limited by considerations of maintainability, availability of parts, transportation and/or cost.
The device implements the pressure-controlled continuous mandatory ventilation mode, complemented by a simple assist-control mode. Continuous positive airway pressure is also possible. The consumption of compressed gases is minimized by avoiding a continuous flow of oxygen or air. Respiratory rates and inspiration/expiration time ratios are electronically determined, and an apnea/power loss alarm is provided.
The pressure profiles were measured for a range of conditions and found to be adjustable within a ± 2.5cmH2O error margin and stable well within this range over a 41-hour period. Respiratory cycle timing parameters were precise within a few percentage points over the same period. The device was tested for durability for an equivalent period of four months. Chemical and biological tests failed to identify any contamination of the gas by volatile organic compounds or microorganisms. A ventilation test on a large animal, in comparison with a well established ventilator, showed that the animal could be adequately ventilated over a period of 60 minutes, without any noticeable negative aftereffects during the subsequent 24-hour period.
This ventilator design may be viable, after further animal tests and formal approval by the competent authorities, for clinical application in the abovementioned atypical circumstances.

Abstract
Rev Bras Ter Intensiva. 2022;34(1):185-196
DOI 10.5935/0103-507X.20220013-en
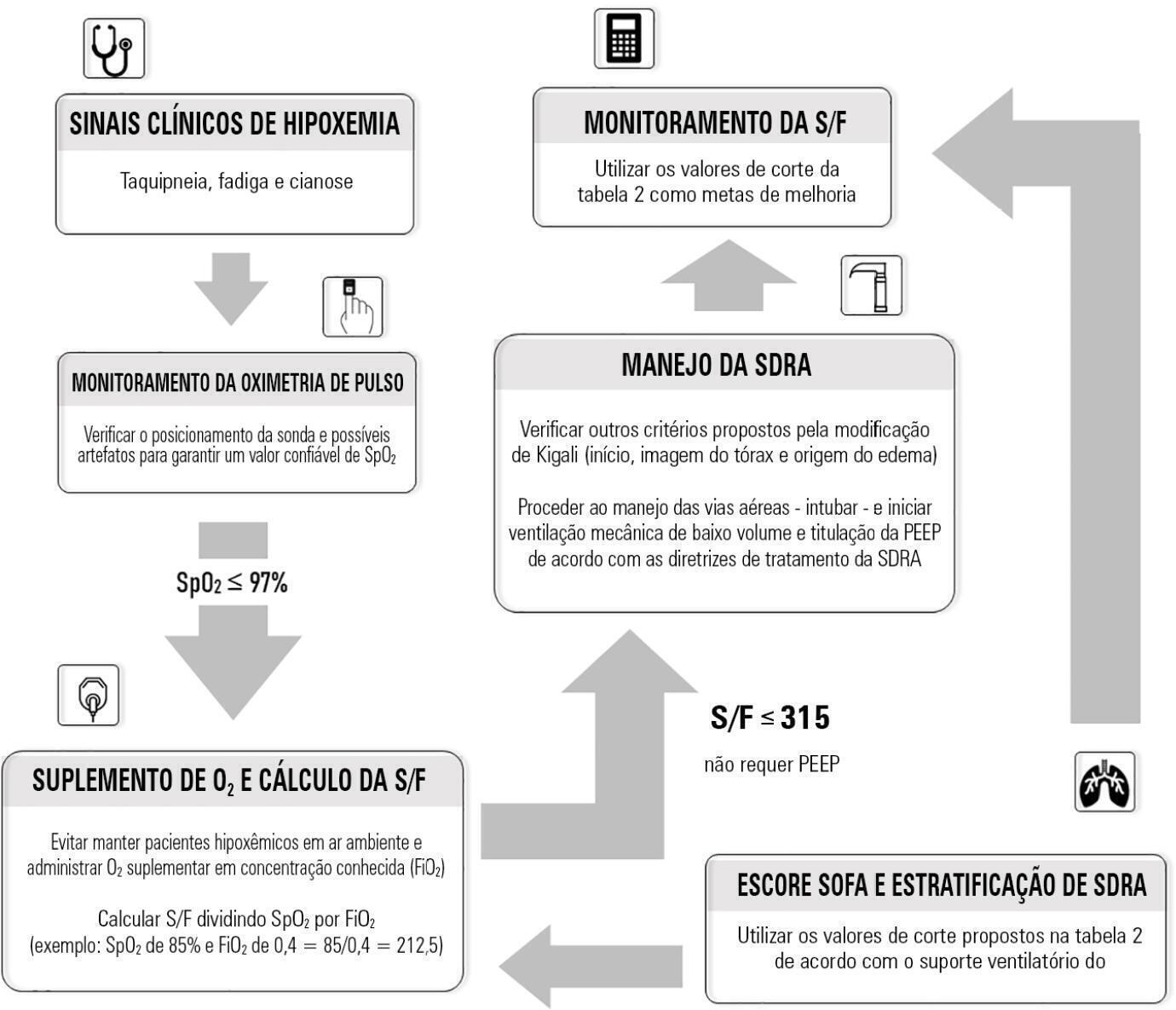
Although the PaO 2/FiO 2 derived from arterial blood gas analysis remains the gold standard for the diagnosis of acute respiratory failure, the SpO2/FiO2 has been investigated as a potential substitute. The current narrative review presents the state of the preclinical and clinical literature on the SpO2/FiO2 as a possible substitute for PaO2/FiO2 and for use as a diagnostic and prognostic marker; provides an overview of pulse oximetry and its limitations, and assesses the utility of SpO2/ FiO2 as a surrogate for PaO2/FiO2 in COVID-19 patients. Overall, 49 studies comparing SpO2/FiO2 and PaO2/FiO2 were found according to a minimal search strategy. Most were conducted on neonates, some were conducted on adults with acute respiratory distress syndrome, and a few were conducted in other clinical scenarios (including a very few on COVID-19 patients). There is some evidence that the SpO2/ FiO2 criteria can be a surrogate for PaO2/FiO2 in different clinical scenarios. This is reinforced by the fact that unnecessary invasive procedures should be avoided in patients with acute respiratory failure. It is undeniable that pulse oximeters are becoming increasingly widespread and can provide costless monitoring. Hence, replacing PaO2/FiO2 with SpO2/FiO2may allow resourcelimited facilities to objectively diagnose acute respiratory failure.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):168-174
DOI 10.5935/0103-507X.20130029
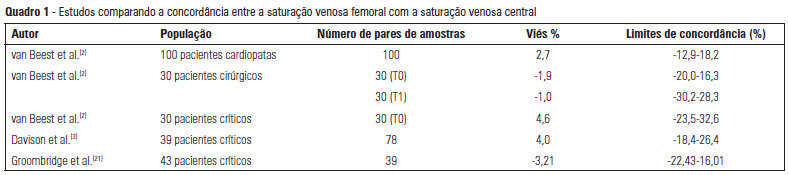
The use of central venous oxygen saturation (SvcO2) and arterial lactate in the diagnosis of severe tissue hypoperfusion is well established, and the optimization of these parameters is currently under investigation, particularly in patients with severe sepsis/septic shock. However, the only place for deep venous puncture or the first choice for puncture is often the femoral vein. Although venous saturation obtained from blood sampling from this catheter, instead of SvcO2, has already been used in the diagnosis of severe tissue hypoperfusion, little is known about the accuracy of the results. The venous lactate in place of arterial puncture has also been used to guide therapeutic decisions. We conducted this literature review to seek evidence on the correlation and concordance of parameters obtained by collecting femoral venous blood gases in relation to SvcO2 and arterial lactate. Few studies in the literature have evaluated the use of femoral venous oxygen saturation (SvfO2) or venous lactate. The results obtained thus far demonstrate no adequate agreement between SvfO2 and SvcO2, which limits the clinical use of SvfO2. However, the apparent strong correlation between arterial and peripheral and central venous lactate values suggests that venous lactate obtained from the femoral vein could eventually be used instead of arterial lactate, although there is insufficient evidence on which to base this procedure at this time.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):283-290
DOI 10.1590/S0103-507X2011000300005
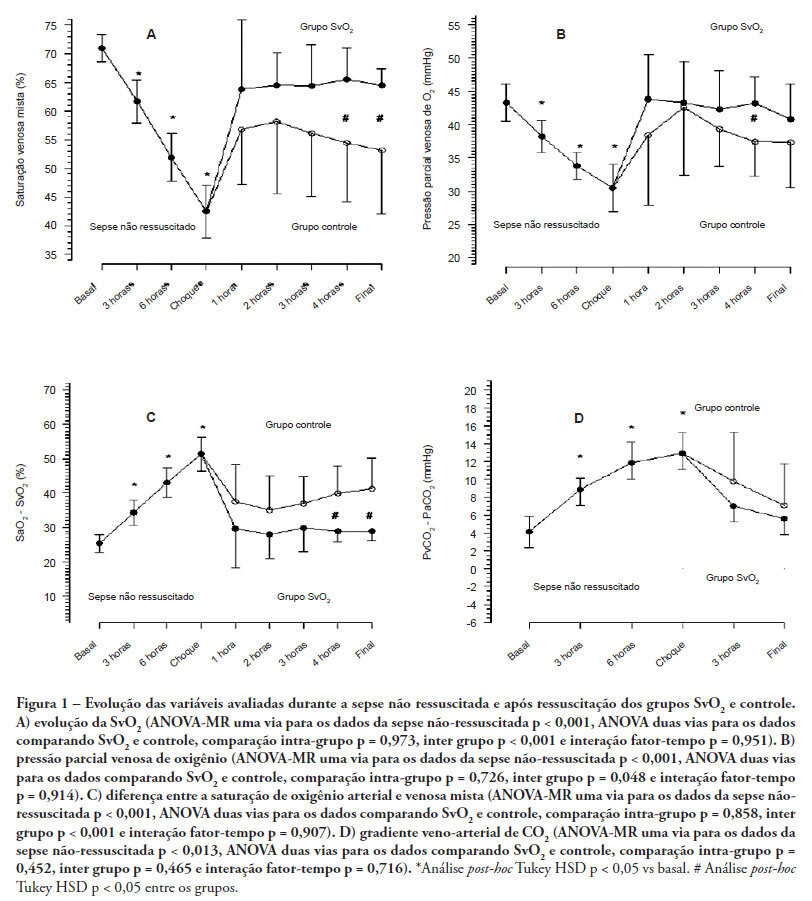
OBJECTIVES: Although fluid resuscitation guided by central venous oxygen saturation (SvcO2) is currently considered the gold standard in sepsis therapy, few studies have described hemodynamic and perfusion parameters during this procedure. This study aims to describe these parameters during septic shock without resuscitation and after 12 hours of goal-directed resuscitation. METHODS: Thirteen anesthetized pigs (35-45 kg) had peritonitis caused by fecal inoculation (0.75 g/kg). After developing persistent hypotension, both groups were given antibiotics and randomized either to the control group (n=7) or the experimental group (n=6). In the control group, hemodynamic control was optimized to maintain a central venous pressure of 8-12 mmHg, a urinary output above 0.5 mL/kg/hour and a mean arterial blood pressure above 65 mmHg. The experimental group received the above target therapy in addition to maintaining a SvO2 above 65%. The interventions included lactated Ringer's solution and norepinephrine for both groups and dobutamine in the SvO2 group. The animals were treated for 12 hours or until death. RESULTS: Untreated sepsis was associated with significant reductions in SvO2, PvO2, cardiac output and central venous pressure in addition to increased arteriovenous oxygen saturation and veno-arterial CO2 differences. Following resuscitation, these parameters were corrected in both groups. Goal-directed resuscitation was associated with a better hemodynamic profile, characterized by higher SvO2, cardiac output and central venous pressure. CONCLUSIONS: Non-resuscitated sepsis showed a hemodynamic profile suggesting hypovolemia, with worsened perfusion and hemodynamics, which is reversed upon fluid resuscitation. Goal-directed resuscitation is associated with significantly improved hemodynamic and perfusion parameters
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)