Abstract
Rev Bras Ter Intensiva. 2022;34(3):351-359
DOI 10.5935/0103-507X.20220383-en
To develop a simple, robust, safe and efficient invasive mechanical ventilator that can be used in remote areas of the world or war zones where the practical utility of more sophisticated equipment is limited by considerations of maintainability, availability of parts, transportation and/or cost.
The device implements the pressure-controlled continuous mandatory ventilation mode, complemented by a simple assist-control mode. Continuous positive airway pressure is also possible. The consumption of compressed gases is minimized by avoiding a continuous flow of oxygen or air. Respiratory rates and inspiration/expiration time ratios are electronically determined, and an apnea/power loss alarm is provided.
The pressure profiles were measured for a range of conditions and found to be adjustable within a ± 2.5cmH2O error margin and stable well within this range over a 41-hour period. Respiratory cycle timing parameters were precise within a few percentage points over the same period. The device was tested for durability for an equivalent period of four months. Chemical and biological tests failed to identify any contamination of the gas by volatile organic compounds or microorganisms. A ventilation test on a large animal, in comparison with a well established ventilator, showed that the animal could be adequately ventilated over a period of 60 minutes, without any noticeable negative aftereffects during the subsequent 24-hour period.
This ventilator design may be viable, after further animal tests and formal approval by the competent authorities, for clinical application in the abovementioned atypical circumstances.

Abstract
Rev Bras Ter Intensiva. 2020;32(2):319-325
DOI 10.5935/0103-507X.20200032
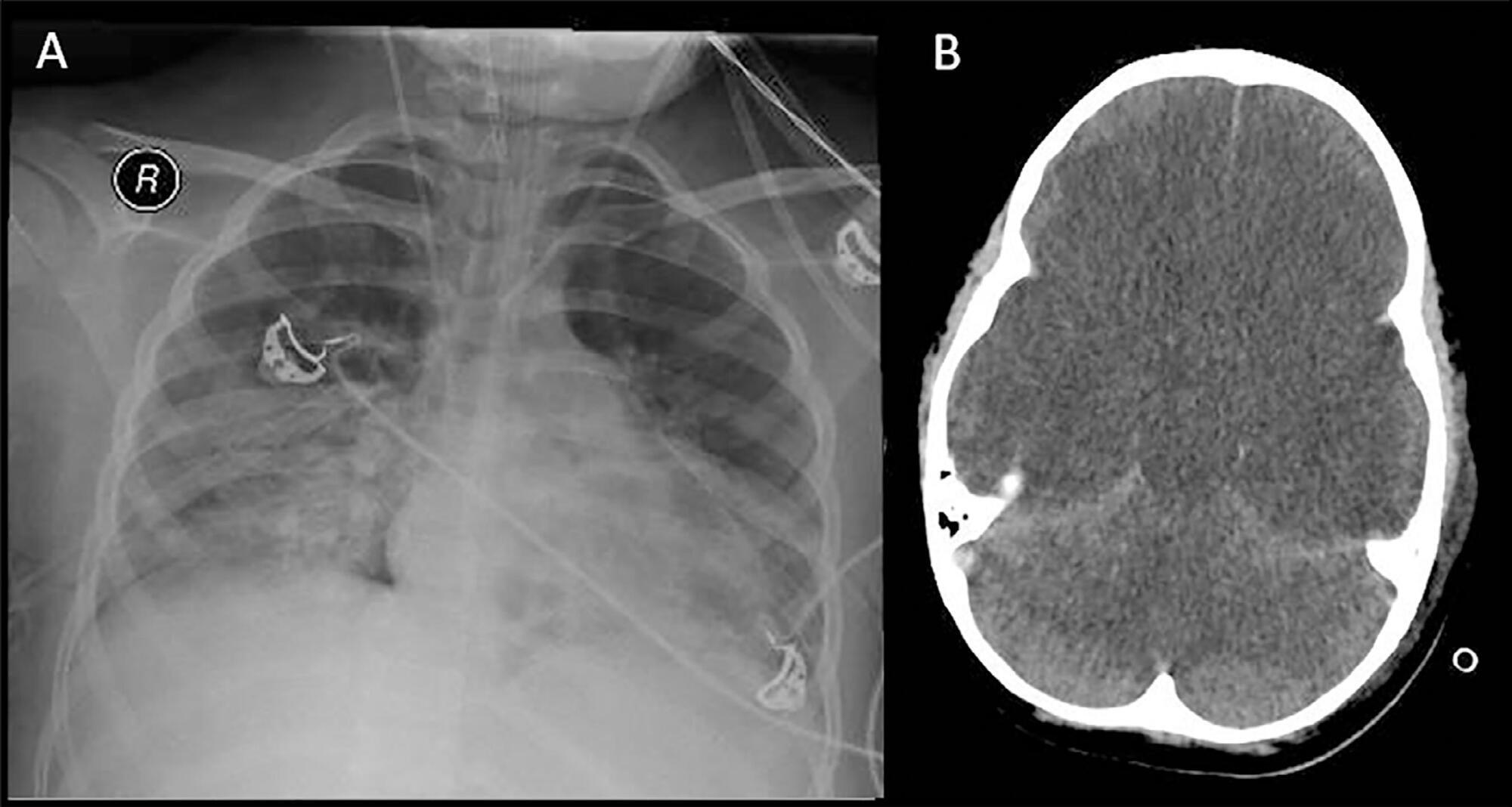
The apnea test, which involves disconnection from the mechanical ventilator, presents risks during the determination of brain death, especially in hypoxemic patients. We describe the performance of the apnea test without disconnection from the mechanical ventilator in two patients. The first case involved an 8-year-old boy admitted with severe hypoxemia due to pneumonia. He presented with cardiorespiratory arrest, followed by unresponsive coma due to hypoxic-ischemic encephalopathy. Two clinical exams revealed the absence of brainstem reflexes, and transcranial Doppler ultrasound revealed brain circulatory arrest. Three attempts were made to perform the apnea test, which were interrupted by hypoxemia; therefore, the apnea test was performed without disconnection from the mechanical ventilator, adjusting the continuous airway pressure to 10cmH2O and the inspired fraction of oxygen to 100%. The oxygen saturation was maintained at 100% for 10 minutes. Posttest blood gas analysis results were as follows: pH, 6.90; partial pressure of oxygen, 284.0mmHg; partial pressure of carbon dioxide, 94.0mmHg; and oxygen saturation, 100%. The second case involved a 43-year-old woman admitted with subarachnoid hemorrhage (Hunt-Hess V and Fisher IV). Two clinical exams revealed unresponsive coma and absence of all brainstem reflexes. Brain scintigraphy showed no radioisotope uptake into the brain parenchyma. The first attempt at the apnea test was stopped after 5 minutes due to hypothermia (34.9°C). After rewarming, the apnea test was repeated without disconnection from the mechanical ventilator, showing maintenance of the functional residual volume with electrical bioimpedance. Posttest blood gas analysis results were as follows: pH, 7.01; partial pressure of oxygen, 232.0mmHg; partial pressure of carbon dioxide, 66.9mmHg; and oxygen saturation, 99.0%. The apnea test without disconnection from the mechanical ventilator allowed the preservation of oxygenation in both cases. The use of continuous airway pressure during the apnea test seems to be a safe alternative in order to maintain alveolar recruitment and oxygenation during brain death determination.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):483-489
DOI 10.5935/0103-507X.20190071
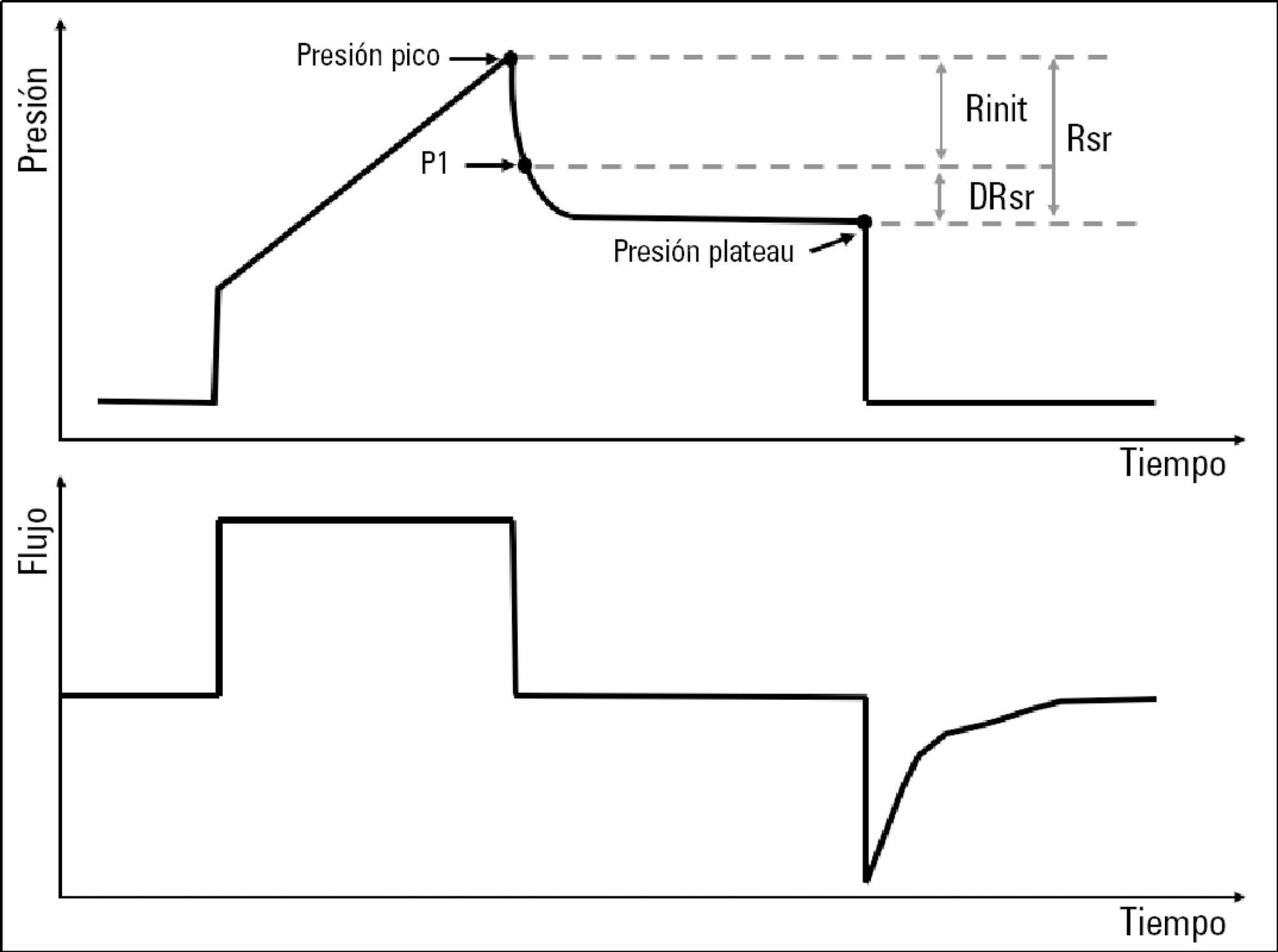
To describe the behavior of inspiratory resistance components when positive end-expiratory pressure (PEEP) increases in patients with acute respiratory distress syndrome under a protective ventilation strategy.
In volume-controlled mode, at 6mL/kg and constant flow, end-inspiratory occlusions were performed at 0, 5 10, 15 and 20cmH2O PEEP. Peak, initial and plateau pressure values were assessed, calculating the maximum, minimum and differential resistances. The results were compared by repeated measures analysis of variance (ANOVA) with post hoc Bonferroni correction, considering p < 0.05 significant.
The highest maximum resistance was observed at the lowest PEEP levels. The values for 10 and 15cmH2O PEEP significantly differed from those for 5 and 0cmH2O PEEP, whereas that for 20cmH2O PEEP only significantly differed from that for 0cmH2O PEEP (p < 0.05). The minimum resistance behaved similarly to the maximum resistance; the values for PEEP levels from 10cmH2O to 20cmH2O significantly differed from those for 0 and 5cmH2O PEEP (p < 0.05). Differential resistance showed the opposite variation to the maximum and minimum resistances. The only PEEP level that showed significant differences from 0 and 5cmH2O PEEP was 20cmH2O PEEP. Significant differences were also found between 15 and 5cmH2O PEEP (p < 0.05).
During protective ventilation in patients with acute respiratory distress syndrome, the maximum resistance of the respiratory system decreases with PEEP, reflecting the minimum resistance response, whereas differential resistance increases with PEEP.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):375-380
DOI 10.1590/S0103-507X2012000400014
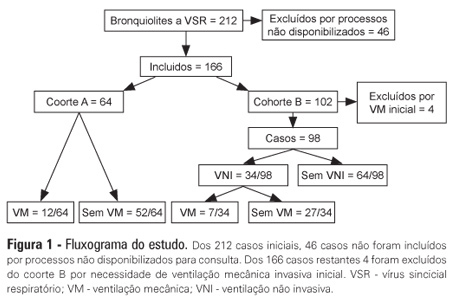
OBJECTIVES: The present study focused on respiratory syncytial virus bronchiolitis with respiratory failure. The aim of the study was to determine whether noninvasive ventilation reduces the need for endotracheal intubation or slows the clinical progression of acute respiratory syncytial virus bronchiolitis by reducing the incidence of infectious complications. METHODS: The present study was a retrospective cohort study. Cohort A was comprised of children who were admitted to the pediatric intensive and special care unit from 2003-2005 before starting noninvasive ventilation; cohort B was comprised of children who were admitted to the pediatric intensive and special care unit from 2006-2008 after starting noninvasive ventilation. With the exception of noninvasive ventilation, the therapeutic support was the same for the two groups. All children who were diagnosed with respiratory syncytial virus bronchiolitis and respiratory failure between November 2003 and March 2008 were included in the cohort. Demographic, clinical and blood gas variables were analyzed. RESULTS: A total of 162 children were included; 75% of the subjects were less than 3 months old. Group A included 64 children, and group B included 98 children. In group B, 34 of the children required noninvasive ventilation. The distributions of the variables age, preterm birth, congenital heart disease, cerebral palsy and chronic lung disease were similar between the two groups. On admission, the data for blood gas analysis and the number of apneas were not significantly different between the groups. In group B, fewer children required invasive ventilation (group A: 12/64 versus group B: 7/98; p=0.02), and there was a reduction in the number of cases of bacterial pneumonia (group A: 19/64 versus group B: 12/98; p=0.008). There was no record of mortality in either of the groups. CONCLUSION: By comparing children with the same disease both before and after noninvasive ventilation was used for ventilation support, we verified a reduction in infectious complications and cases requiring intubation.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):319-326
DOI 10.5935/0103-507X.20130054
In preterm infants, the need for intubation and mechanical ventilation is associated with ventilator-induced lung injuries and subsequent bronchopulmonary dysplasia. The aim of the present review was to improve the understanding of the mechanisms of injury that involve cytokine-mediated inflammation to contribute to the development of new preventive strategies. Relevant articles were retrieved from the PubMed database using the search terms "ventilator-induced lung injury preterm", "continuous positive airway pressure", "preterm", and "bronchopulmonary dysplasia". The resulting data and other relevant information were divided into several topics to ensure a thorough, critical view of ventilation-induced lung injury and its consequences in preterm infants. The role of pro-inflammatory cytokines (particularly interleukins 6 and 8 and tumor necrosis factor alpha) as mediators of lung injury was assessed. Evidence from studies conducted with animals and human newborns is described. This evidence shows that brief periods of mechanical ventilation is sufficient to induce the release of pro-inflammatory cytokines. Other forms of mechanical and non-invasive ventilation were also analyzed as protective alternatives to conventional mechanical ventilation. It was concluded that non-invasive ventilation, intubation followed by early surfactant administration and quick extubation for nasal continuous positive airway pressure, and strategies that regulate tidal volume and avoid volutrauma (such as volume guarantee ventilation) protect against ventilator-induced lung injury in preterm infants.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):278-283
DOI 10.1590/S0103-507X2012000300012
OBJECTIVE: This study analyzed acute respiratory failure caused by acute pulmonary edema, as well as chronic obstructive pulmonary disease exacerbation, that was treated with non-invasive mechanical ventilation to identify the factors that are associated with the success or failure non-invasive mechanical ventilation in urgent and emergency service. METHODS: This study was a prospective, descriptive and analytical study. We included patients of both genders aged >18 years who used non-invasive mechanical ventilation due to acute respiratory failure that was secondary to acute pulmonary edema or chronic obstructive pulmonary disease exacerbation. Patients with acute respiratory failure that was secondary to pathologies other than acute pulmonary edema and chronic obstructive pulmonary disease or who presented with contraindications for the technique were excluded. Expiratory pressures between 5 and 8 cmH2O and inspiratory pressures between 10 and 12 cmH2O were used. Supplemental oxygen maintained peripheral oxygen saturation at >90%. The primary outcome was endotracheal intubation. RESULTS: A total of 152 patients were included. The median non-invasive mechanical ventilation time was 6 hours (range 1 - 32 hours) for chronic obstructive pulmonary disease patients (n=60) and 5 hours (range 2 - 32 hours) for acute pulmonary edema patients (n=92). Most (75.7%) patients progressed successfully. However, reduced APACHE II scores and lower peripheral oxygen saturation were observed. These results were statistically significant in patients who progressed to intubation (p<0.001). BiPAP (Bi-level Positive Airway Pressure portable ventilator), as continuous positive airway pressure use increased the probability of endotracheal intubation 2.3 times (p=0.032). Patients with acute pulmonary edema and elevated GCS scores also increased the probability of success. CONCLUSION: Respiratory frequency >25 rpm, higher APACHE II scores, BiPAP use and chronic obstructive pulmonary disease diagnosis were associated with endotracheal intubation. Higher GCS and SpO2 values were associated with NIV success. Non-invasive mechanical ventilation can be used in emergency services in acute respiratory failure cases caused by acute pulmonary edema and chronic obstructive pulmonary disease exacerbation, but patients with variables related to a higher percentage of endotracheal intubation should be specially monitored.
Abstract
Rev Bras Ter Intensiva. 2009;21(2):155-161
DOI 10.1590/S0103-507X2009000200007
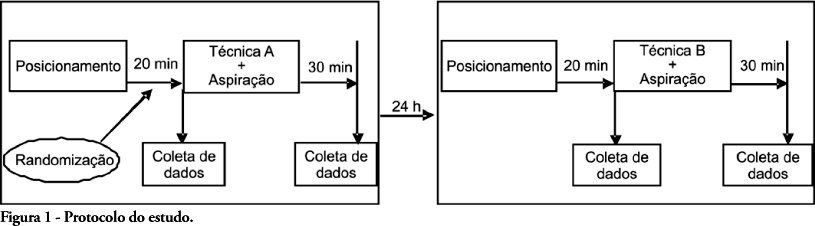
OBJECTIVES: Patients unable to perform breathing functions may be submitted to invasive mechanical ventilation. Chest physiotherapy acts directly on the treatment of these patients for the purpose of improving their lung function. The objective of this study was to evaluate the effects of manual rib-cage compression versus the positive end expiratory pressure-zero end expiratory pressure (PEEP-ZEEP) maneuver, on compliance of the respiratory system and oxygenation in patients under invasive mechanical ventilation. METHODS: A double centric, prospective, randomized and crossover study, with patients under invasive mechanical ventilation, in controlled mode for more than 48 hours was carried out. The protocols of chest physiothe-rapy were randomly applied at an interval of 24 hours. Data of respiratory system compliance and oxygenation were collected before application of the protocols and 30 minutes after. RESULTS: Twelve patients completed the study. Intragroup analysis, for both techniques showed a statistically significant difference in tidal volume (p=0.002), static compliance (p=0.002) and dynamic compliance (p=0.002). In relation to oxygenation, in the group of manual rib-cage compression, peripheral oxygen saturation increased with a significant difference (p=0.011). CONCLUSIONS: Manual rib-cage compression and PEEP-ZEEP maneuver have positive clinical effects. In relation to oxygenation we found a favorable behavior of peripheral oxygen saturation in the group of manual rib-cage compression.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)