Abstract
Rev Bras Ter Intensiva. 2019;31(1):86-92
DOI 10.5935/0103-507X.20190009
To examine the association between donor plasma cytokine levels and the development of primary graft dysfunction of organs transplanted from deceased donors.
Seventeen deceased donors and the respective 47 transplant recipients were prospectively included in the study. Recipients were divided into two groups: group 1, patients who developed primary graft dysfunction; and group 2, patients who did not develop primary graft dysfunction. Donor plasma levels of TNF, IL-6, IL-1β, and IFN-γ assessed by ELISA were compared between groups.
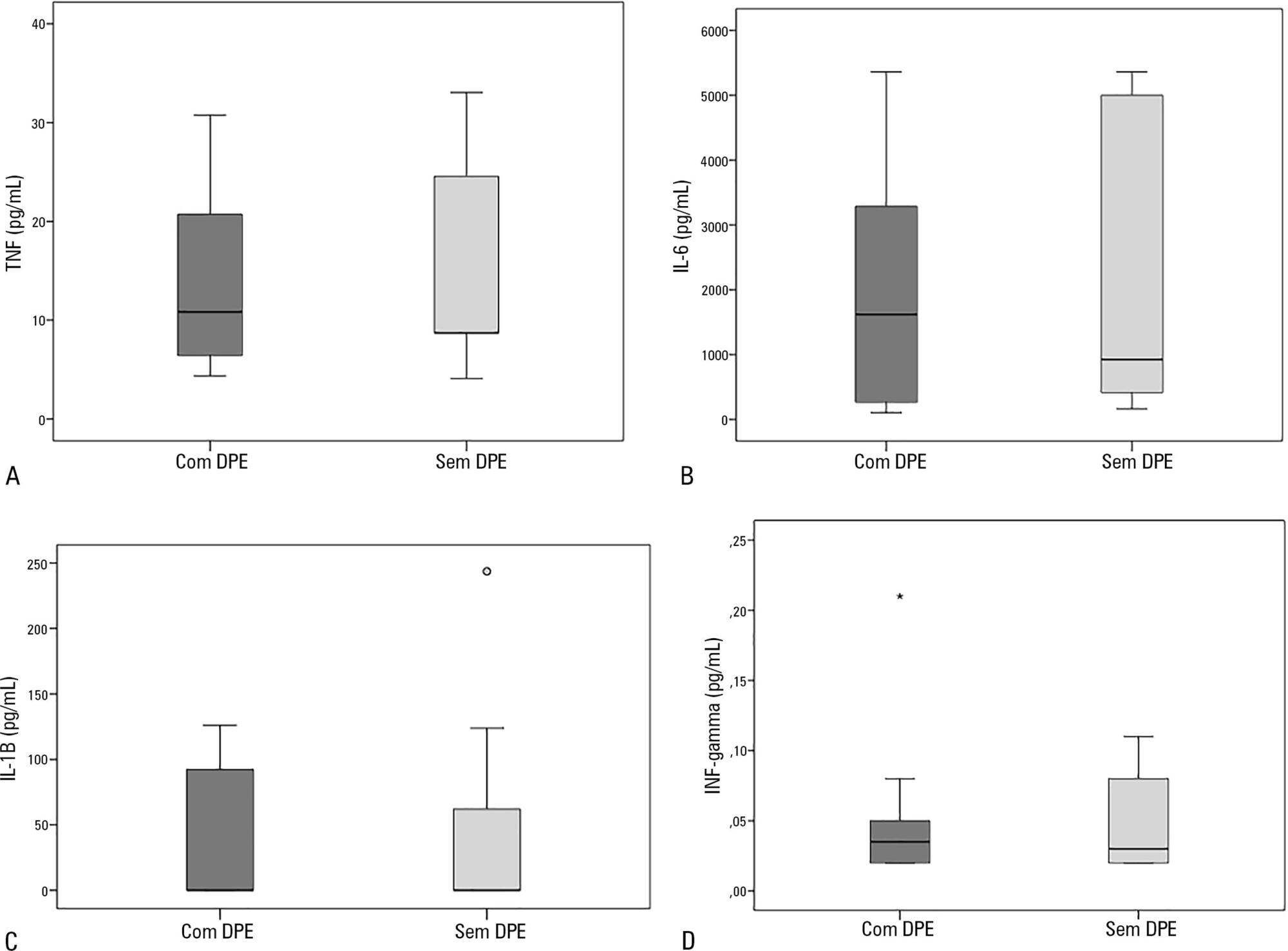
Sixty-nine organs were retrieved, and 48 transplants were performed. Donor plasma cytokine levels did not differ between groups (in pg/mL): TNF, group 1: 10.8 (4.3 - 30.8) versus group 2: 8.7 (4.1 - 33.1), p = 0.63; IL-6, group 1: 1617.8 (106.7 - 5361.7) versus group 2: 922.9 (161.7 - 5361.7), p = 0.56; IL-1β, group 1: 0.1 (0.1 - 126.1) versus group 2: 0.1 (0.1 - 243.6), p = 0.60; and IFN-γ, group 1: 0.03 (0.02 - 0.2) versus group 2: 0.03 (0.02 - 0.1), p = 0.93). Similar findings were obtained when kidney transplants were analyzed separately.
In this sample of transplant recipients, deceased donor plasma cytokines TNF, IL-6, IL-1β, and IFN-γ were not associated with the development of primary graft dysfunction.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):319-326
DOI 10.5935/0103-507X.20130054
In preterm infants, the need for intubation and mechanical ventilation is associated with ventilator-induced lung injuries and subsequent bronchopulmonary dysplasia. The aim of the present review was to improve the understanding of the mechanisms of injury that involve cytokine-mediated inflammation to contribute to the development of new preventive strategies. Relevant articles were retrieved from the PubMed database using the search terms "ventilator-induced lung injury preterm", "continuous positive airway pressure", "preterm", and "bronchopulmonary dysplasia". The resulting data and other relevant information were divided into several topics to ensure a thorough, critical view of ventilation-induced lung injury and its consequences in preterm infants. The role of pro-inflammatory cytokines (particularly interleukins 6 and 8 and tumor necrosis factor alpha) as mediators of lung injury was assessed. Evidence from studies conducted with animals and human newborns is described. This evidence shows that brief periods of mechanical ventilation is sufficient to induce the release of pro-inflammatory cytokines. Other forms of mechanical and non-invasive ventilation were also analyzed as protective alternatives to conventional mechanical ventilation. It was concluded that non-invasive ventilation, intubation followed by early surfactant administration and quick extubation for nasal continuous positive airway pressure, and strategies that regulate tidal volume and avoid volutrauma (such as volume guarantee ventilation) protect against ventilator-induced lung injury in preterm infants.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):426-433
DOI 10.1590/S0103-507X2011000400006
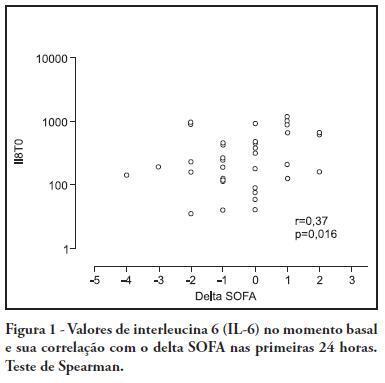
OBJECTIVE: To investigate the correlation of organ dysfunction and its progression with inflammatory response during the early phases of septic shock by assessing baseline cytokine concentrations. METHODS: This study included patients over 18 years old with septic shock within the first 48 hours after the onset of organ dysfunction. Interleukin 6 (IL-6), interleukin 8 (IL-8), interleukin 10 (IL-10) and C-reactive protein levels were assessed at inclusion and after 24 hours, and the differences between these values were calculated. The progression of organ dysfunction was assessed using the Sequential Organ Failure Assessment (SOFA) score upon admission and 24 hours later for a delta-SOFA determination and were categorized as either worsened or improved. The results were expressed as means + standard deviation or median (25-75% percentiles). Values with descriptive p values of 0.05 or less were considered significant. RESULTS: Overall, we included 41 patients with median SOFA scores of 8.0 (6.5-10.0) upon admission (T0) and 8.0 (6.0-10.0) 24 hours later (T1). Worsened, improved or unchanged SOFA scores were observed in 11 (Group 1), 17 (Group 2) and 13 (Group 3) patients, respectively. For Group 1, the baseline IL-6, IL-8 and IL-10 values were higher, and a significant increase of IL-8 levels was found after 24 hours. The change in the SOFA score after 24 hours was significantly, although weakly, correlated with baseline IL-6 and IL-8 concentrations. CONCLUSIONS: Higher baseline IL-6, IL-8 and IL-10 levels are associated with unfavorable organ dysfunction outcomes. Increased IL-8 levels within the first 24 hours are correlated with a worsening dysfunction.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):280-290
DOI 10.1590/S0103-507X2010000300011
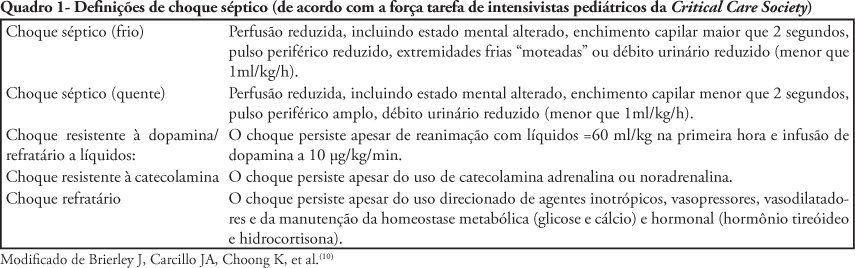
The nonspecific presentation of neonatal sepsis and systemic inflammatory response syndrome preceding septic shock delay the early diagnosis of septic shock and increase its mortality rate. Early diagnosis involves suspecting septic shock in every newborn with tachycardia, respiratory distress, difficult feeding, altered tonus and skin coloration, tachypnea and reduced perfusion, specially in case of maternal peripartum infection, chorioamnionitis or long-term membranes rupture. This article aims to review current knowledge on neonatal period peculiarities, fetal circulation dynamics, and the pregnancy age variable. Newborn septic shock is not just a small adult shock. In the newborn, the septic shock is predominantly cold and characterized by reduced cardiac output and increased systemic vascular resistance (vasoconstriction). Time is fundamental for septic shock reversion. The indexed-databases literature review provides subside for the newborn management.