Abstract
Rev Bras Ter Intensiva. 2022;34(4):477-483
DOI 10.5935/0103-507X.20220280-en
To create and validate a model for predicting septic or hypovolemic shock from easily obtainable variables collected from patients at admission to an intensive care unit.
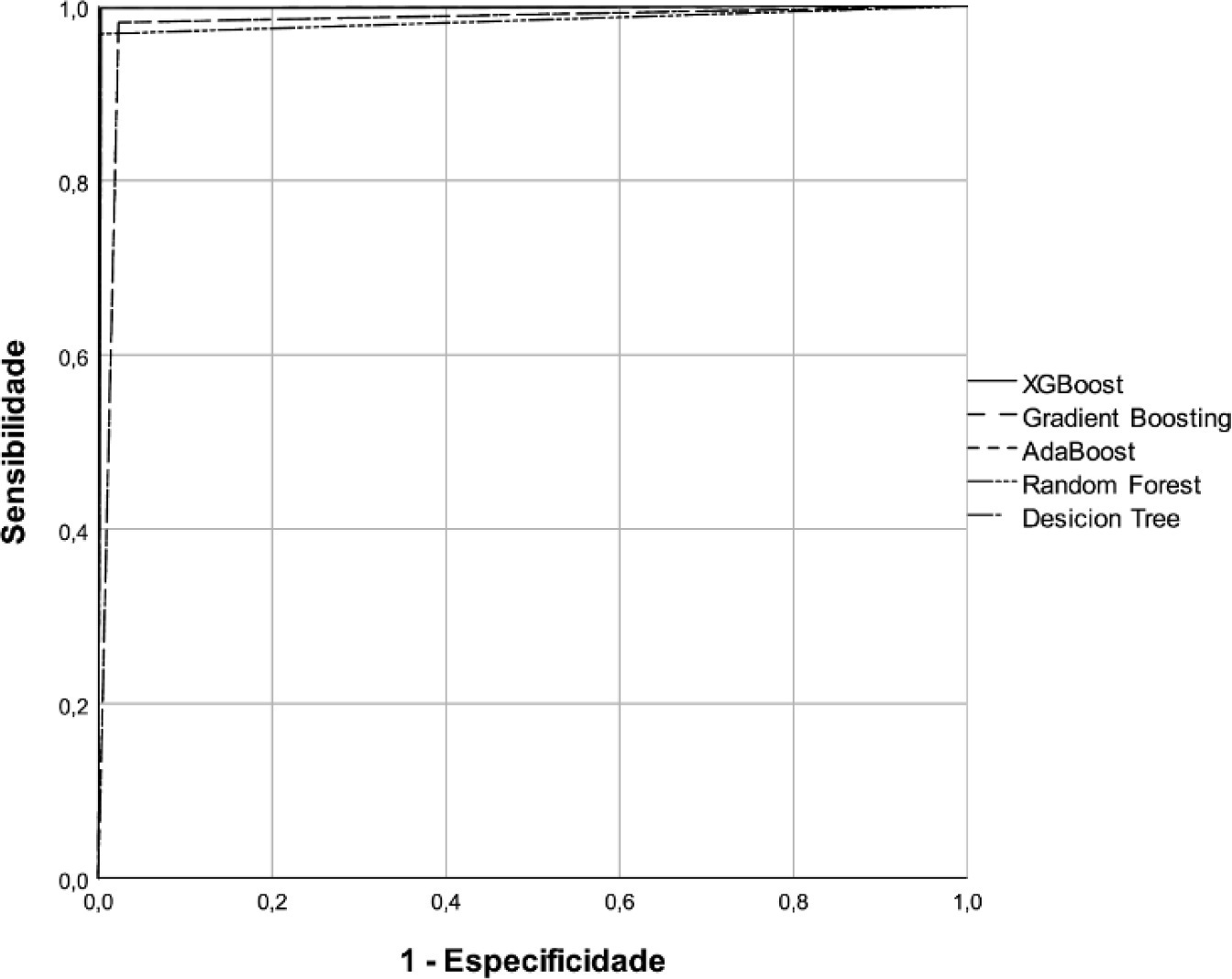
A predictive modeling study with concurrent cohort data was conducted in a hospital in the interior of northeastern Brazil. Patients aged 18 years or older who were not using vasoactive drugs on the day of admission and were hospitalized from November 2020 to July 2021 were included. The Decision Tree, Random Forest, AdaBoost, Gradient Boosting and XGBoost classification algorithms were tested for use in building the model. The validation method used was k-fold cross validation. The evaluation metrics used were recall, precision and area under the Receiver Operating Characteristic curve.
A total of 720 patients were used to create and validate the model. The models showed high predictive capacity with areas under the Receiver Operating Characteristic curve of 0.979; 0.999; 0.980; 0.998 and 1.00 for the Decision Tree, Random Forest, AdaBoost, Gradient Boosting and XGBoost algorithms, respectively.
The predictive model created and validated showed a high ability to predict septic and hypovolemic shock from the time of admission of patients to the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2021;33(1):154-166
DOI 10.5935/0103-507X.20210017
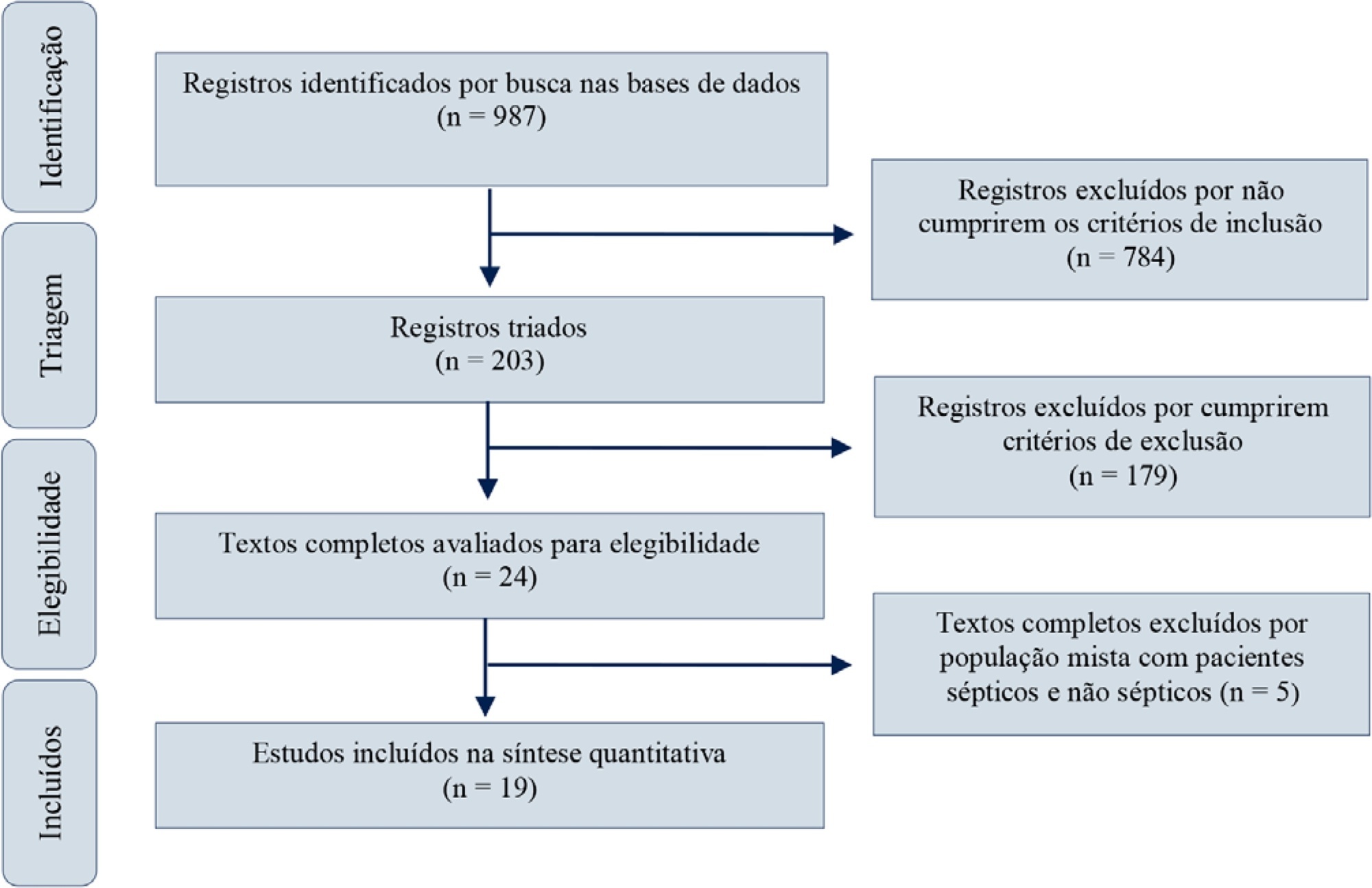
Red blood cell transfusion is thought to improve cell respiration during septic shock. Nevertheless, its acute impact on oxygen transport and metabolism in this condition remains highly debatable. The objective of this study was to evaluate the impact of red blood cell transfusion on microcirculation and oxygen metabolism in patients with sepsis and septic shock. We conducted a search in the MEDLINE®, Elsevier and Scopus databases. We included studies conducted in adult humans with sepsis and septic shock. A systematic review and meta-analysis were performed using the DerSimonian and Laird random-effects model. A p value < 0.05 was considered significant. Nineteen manuscripts with 428 patients were included in the analysis. Red blood cell transfusions were associated with an increase in the pooled mean venous oxygen saturation of 3.7% (p < 0.001), a decrease in oxygen extraction ratio of -6.98 (p < 0.001) and had no significant effect on the cardiac index (0.02L/minute; p = 0,96). Similar results were obtained in studies including simultaneous measurements of venous oxygen saturation, oxygen extraction ratio, and cardiac index. Red blood cell transfusions led to a significant increase in the proportion of perfused small vessels (2.85%; p = 0.553), while tissue oxygenation parameters revealed a significant increase in the tissue hemoglobin index (1.66; p = 0.018). Individual studies reported significant improvements in tissue oxygenation and sublingual microcirculatory parameters in patients with deranged microcirculation at baseline. Red blood cell transfusions seemed to improve systemic oxygen metabolism with apparent independence from cardiac index variations. Some beneficial effects have been observed for tissue oxygenation and microcirculation parameters, particularly in patients with more severe alterations at baseline. More studies are necessary to evaluate their clinical impact and to individualize transfusion decisions.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):551-556
DOI 10.5935/0103-507X.20200092
To analyze the clinical outcome of children with fluid-refractory septic shock initially treated with dopamine or epinephrine.
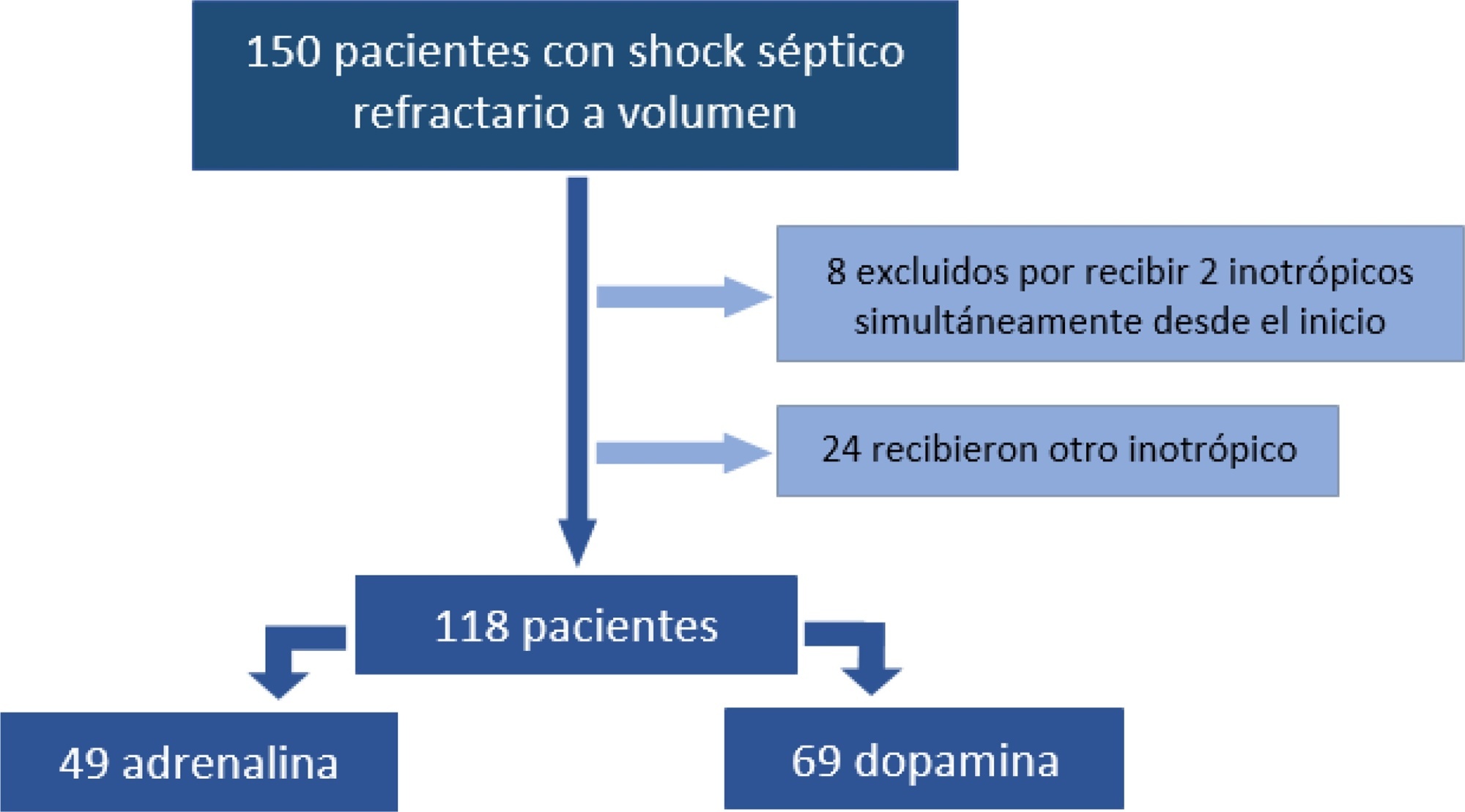
A retrospective cohort study was conducted at a pediatric emergency department of a tertiary hospital. Population: children admitted because of fluid-refractory septic shock. Clinical outcome was compared between two groups: Dopamine and Epinephrine. Variables evaluated were use of invasive mechanical ventilation, days of inotropic therapy, length of hospital stay, intensive care stay, and mortality. For numerical and categorical variables, we used measures of central tendency. They were compared by the Mann-Whitney U-test and the (2 test.
We included 118 patients. A total of 58.5% received dopamine and 41.5% received epinephrine. The rate of invasive mechanical ventilation was 38.8% for epinephrine versus 40.6% for dopamine (p = 0.84), with a median of 4 days for the Epinephrine Group and 5.5 for the Dopamine Group (p = 0.104). Median time of inotropic therapy was 2 days for both groups (p = 0.714). Median hospital stay was 11 and 13 days for the Epinephrine and Dopamine groups, respectively (p = 0.554), and median stay in intensive care was 4 days (0 - 81 days) in both groups (p = 0.748). Mortality was 5% for the Epinephrine Group versus 9% for the Dopamine Group (p = 0.64).
At our center, no differences in use of invasive mechanical ventilation, time of inotropic therapy, length of hospital stay, length of intensive care unit stay, or mortality were observed in children admitted to the pediatric emergency department with a diagnosis of fluid-refractory septic shock initially treated with dopamine versus epinephrine.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):374-380
DOI 10.5935/0103-507X.20200065
To evaluate whether the decrease in blood pressure caused by the increase in the positive end-expiratory pressure corresponds to the pulse pressure variation as an indicator of fluid responsiveness.
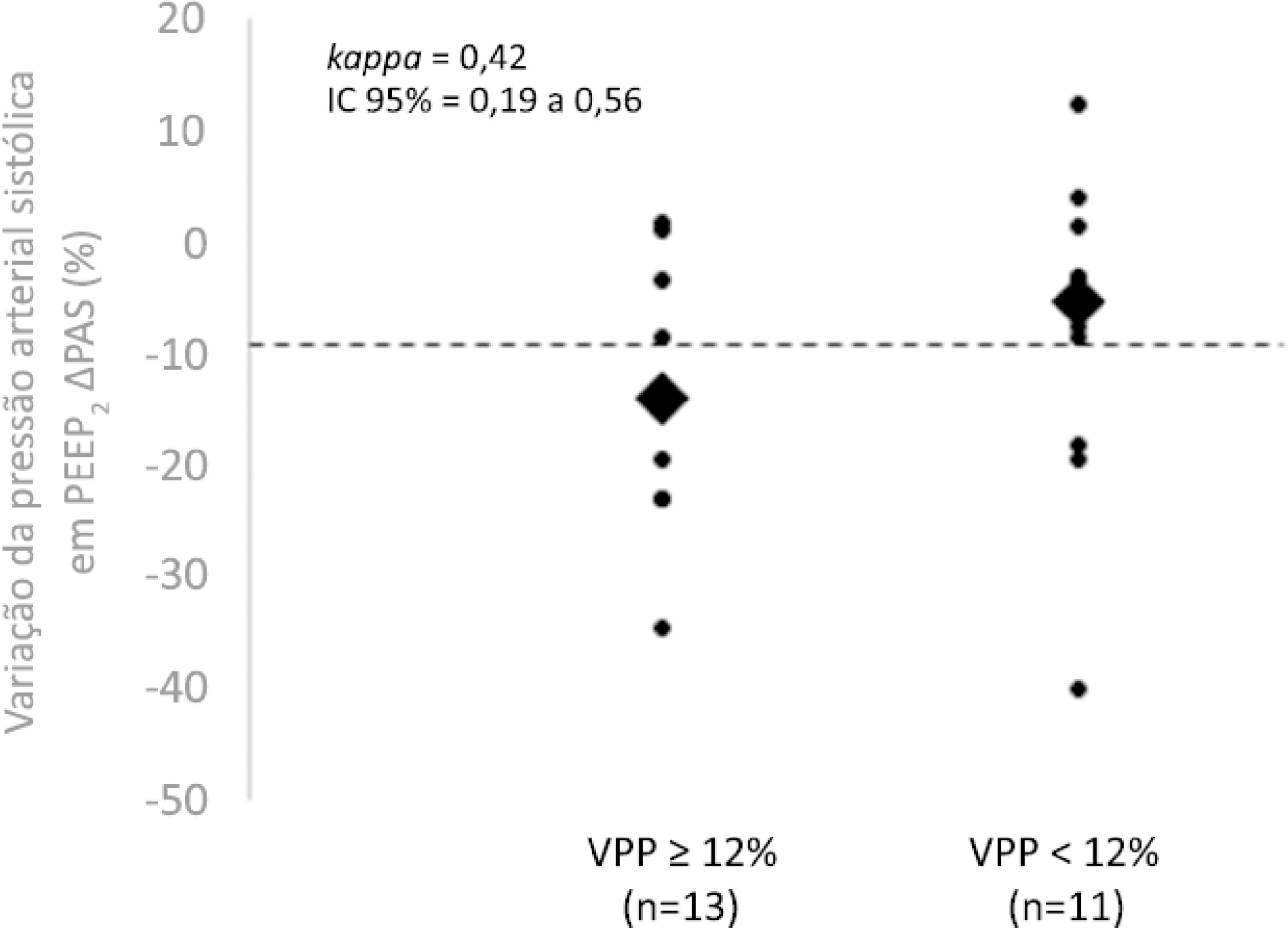
This exploratory study prospectively included 24 patients with septic shock who were mechanically ventilated and subjected to three stages of elevation of the positive end-expiratory pressure: from 5 to 10cmH2O (positive end-expiratory pressure level 1), from 10 to 15cmH2O (positive end-expiratory pressure level 2), and from 15 to 20cmH2O (positive end-expiratory pressure level 3). Changes in systolic blood pressure, mean arterial pressure, and pulse pressure variation were evaluated during the three maneuvers. The patients were classified as responsive (pulse pressure variation ≥ 12%) or unresponsive to volume replacement (pulse pressure variation < 12%).
The best performance at identifying patients with pulse pressure variation ≥ 12% was observed at the positive end-expiratory pressure level 2: -9% systolic blood pressure variation (area under the curve 0.73; 95%CI: 0.49 - 0.79; p = 0.04), with a sensitivity of 63% and specificity of 80%. Concordance was low between the variable with the best performance (variation in systolic blood pressure) and pulse pressure variation ≥ 12% (kappa = 0.42; 95%CI: 0.19 - 0.56). The systolic blood pressure was < 90mmHg at positive end-expiratory pressure level 2 in 29.2% of cases and at positive end-expiratory pressure level 3 in 41.63% of cases.
Variations in blood pressure in response to the increase in positive end-expiratory pressure do not reliably reflect the behavior of the pulse pressure as a measure to identify the fluid responsiveness status.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):99-107
DOI 10.5935/0103-507X.20200015
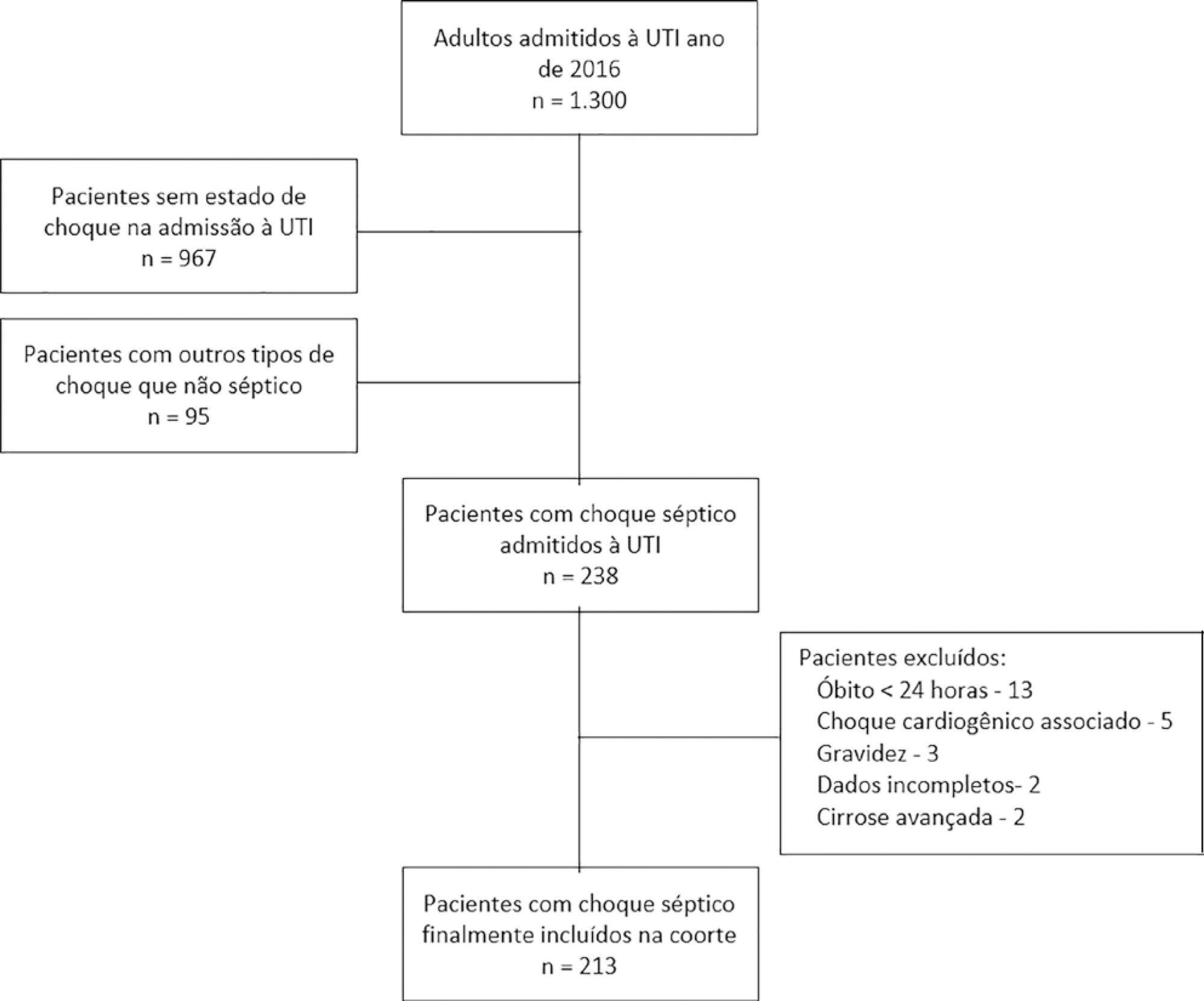
To assess whether fluid overload in fluid therapy is a prognostic factor for patients with septic shock when adjusted for lactate clearance goals.
This was a retrospective cohort study conducted at a level IV care hospital in Bogotá, Colombia. A cohort of patients with septic shock was assembled. Their characteristics and fluid balance were documented. The patients were stratified by exposure levels according to the magnitude of fluid overload by body weight after 24 hours of therapy. Mortality was determined at 30 days, and an unconditional logistic regression model was created, adjusting for confounders. The statistical significance was established at p ≤ 0.05.
There were 213 patients with septic shock, and 60.8% had a lactate clearance ≥ 50% after treatment. Ninety-seven (46%) patients developed fluid overload ≥ 5%, and only 30 (13%) developed overload ≥ 10%. Patients exhibiting fluid overload ≥ 5% received an average of 6227mL of crystalloids (SD ± 5838mL) in 24 hours, compared to 3978mL (SD ± 3728mL) among unexposed patients (p = 0.000). The patients who developed fluid overload were treated with mechanical ventilation (70.7% versus 50.8%) (p = 0.003), albumin (74.7% versus 55.2%) (p = 0.003) and corticosteroids (53.5% versus 35.0%) (p = 0.006) more frequently than those who did not develop fluid overload. In the multivariable analysis, cumulative fluid balance was not associated with mortality (OR 1.03; 95%CI 0.89 - 1.20).
Adjusting for the severity of the condition and adequate lactate clearance, cumulative fluid balance was not associated with increased mortality in this Latin American cohort of septic patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):368-378
DOI 10.5935/0103-507X.20190060
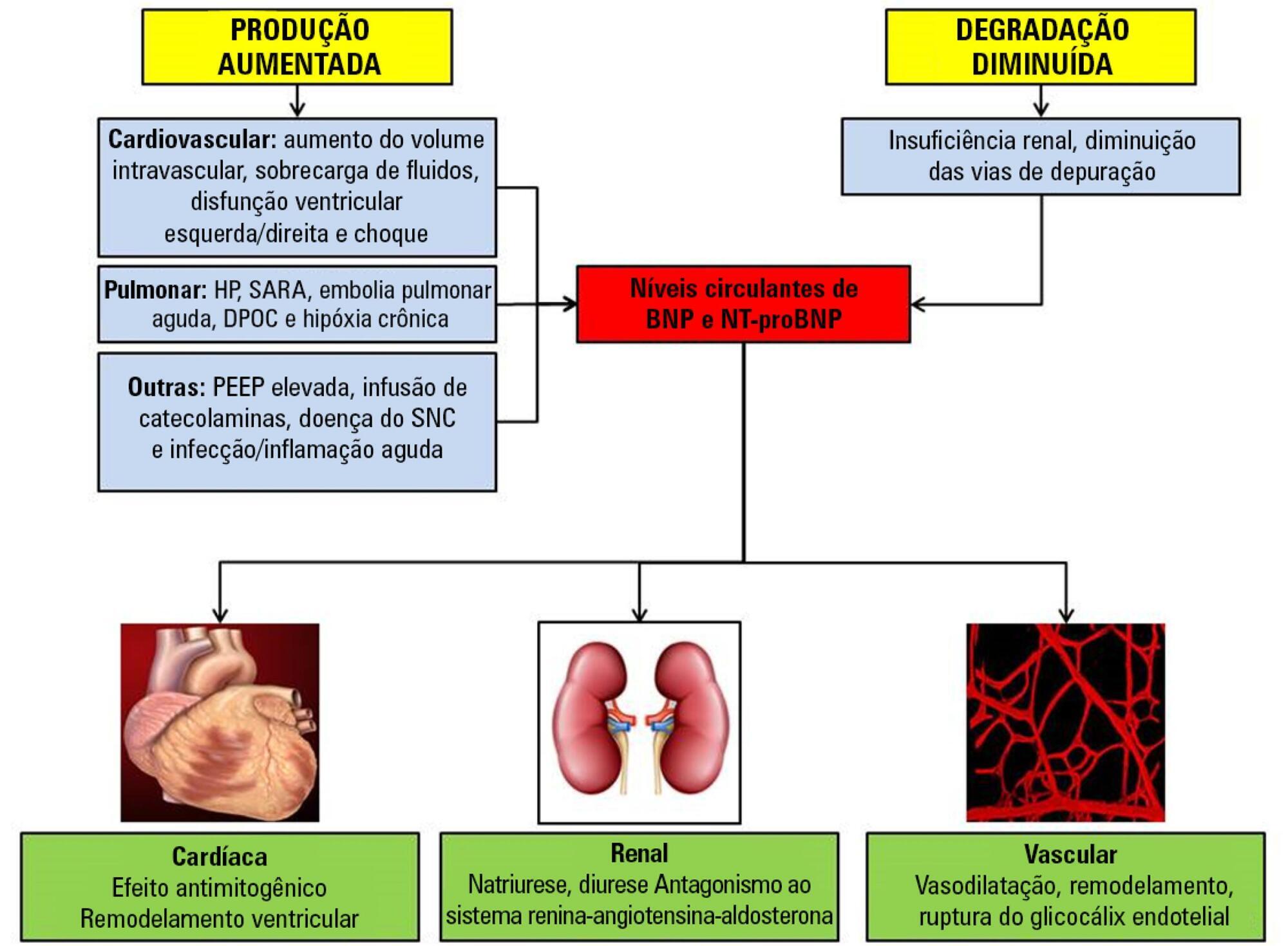
Sepsis continues to be a leading public health burden in the United States and worldwide. With the increasing use of advanced laboratory technology, there is a renewed interest in the use of biomarkers in sepsis to aid in more precise and targeted decision-making. Natriuretic peptides have been increasingly recognized to play a role outside of heart failure. They are commonly elevated among critically ill patients in the setting of cardiopulmonary dysfunction and may play a role in identifying patients with sepsis and septic shock. There are limited data on the role of these biomarkers in the diagnosis, management, outcomes and prognosis of septic patients. This review seeks to describe the role of natriuretic peptides in fluid resuscitation, diagnosis of ventricular dysfunction and outcomes and the prognosis of patients with sepsis. B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP) have been noted to be associated with left ventricular systolic and diastolic and right ventricular dysfunction in patients with septic cardiomyopathy. BNP/NT-proBNP may predict fluid responsiveness, and trends of these peptides may play a role in fluid resuscitation. Despite suggestions of a correlation with mortality, the role of BNP in mortality outcomes and prognosis during sepsis needs further evaluation.
Abstract
Rev Bras Ter Intensiva. 2018;30(3):253-263
DOI 10.5935/0103-507X.20180041
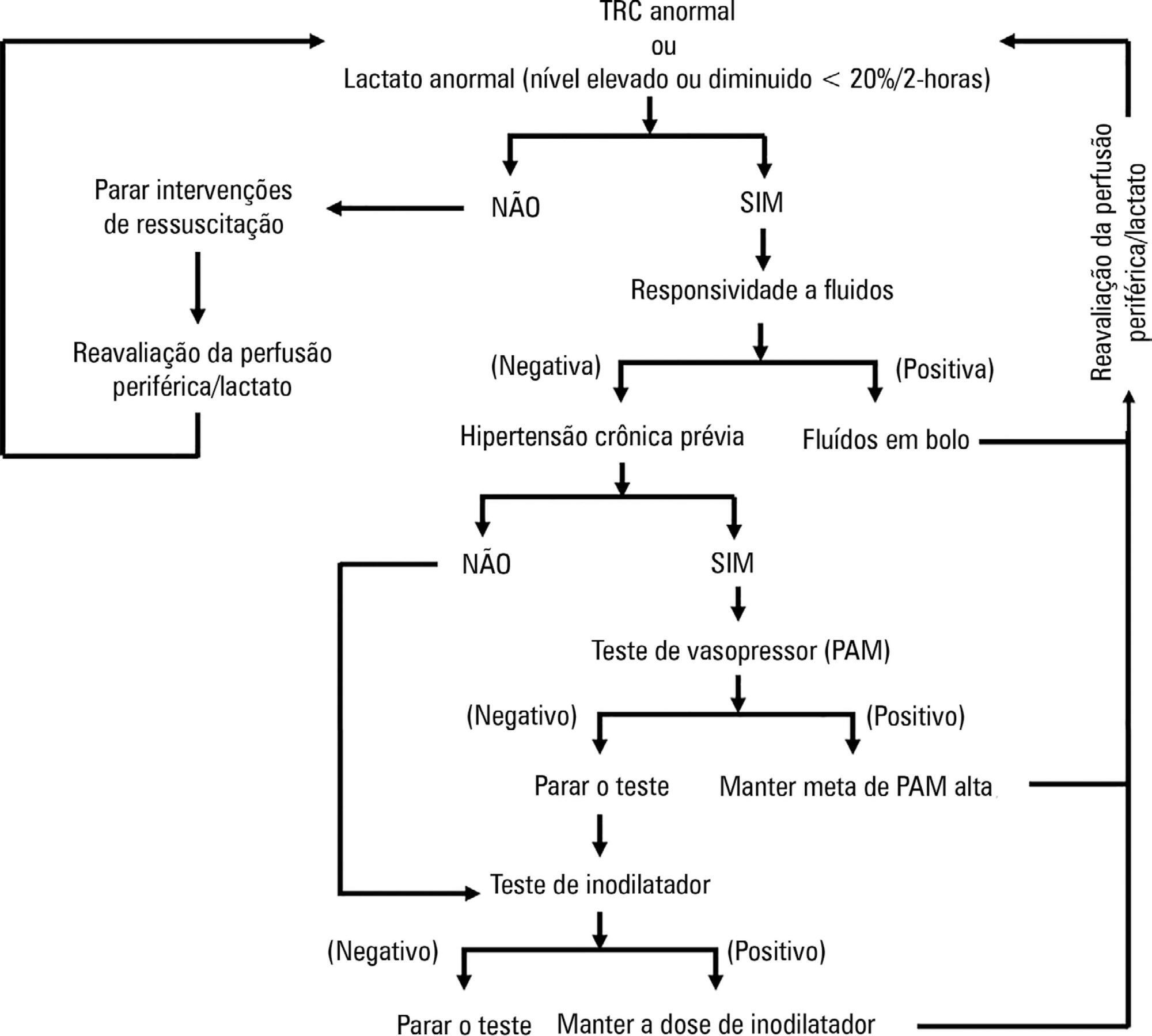
ANDROMEDA-SHOCK is an international, multicenter, randomized controlled trial comparing peripheral perfusion-targeted resuscitation to lactate-targeted resuscitation in patients with septic shock in order to test the hypothesis that resuscitation targeting peripheral perfusion will be associated with lower morbidity and mortality.
To report the statistical analysis plan for the ANDROMEDA-SHOCK trial.
We describe the trial design, primary and secondary objectives, patients, methods of randomization, interventions, outcomes, and sample size. We describe our planned statistical analysis for the primary, secondary and tertiary outcomes. We also describe the subgroup and sensitivity analyses. Finally, we provide details for presenting our results, including mock tables showing baseline characteristics, the evolution of hemodynamic and perfusion variables, and the effects of treatments on outcomes.
According to the best trial practice, we report our statistical analysis plan and data management plan prior to locking the database and initiating the analyses. We anticipate that this procedure will prevent analysis bias and enhance the utility of the reported results.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):14-22
DOI 10.5935/0103-507X.20170004
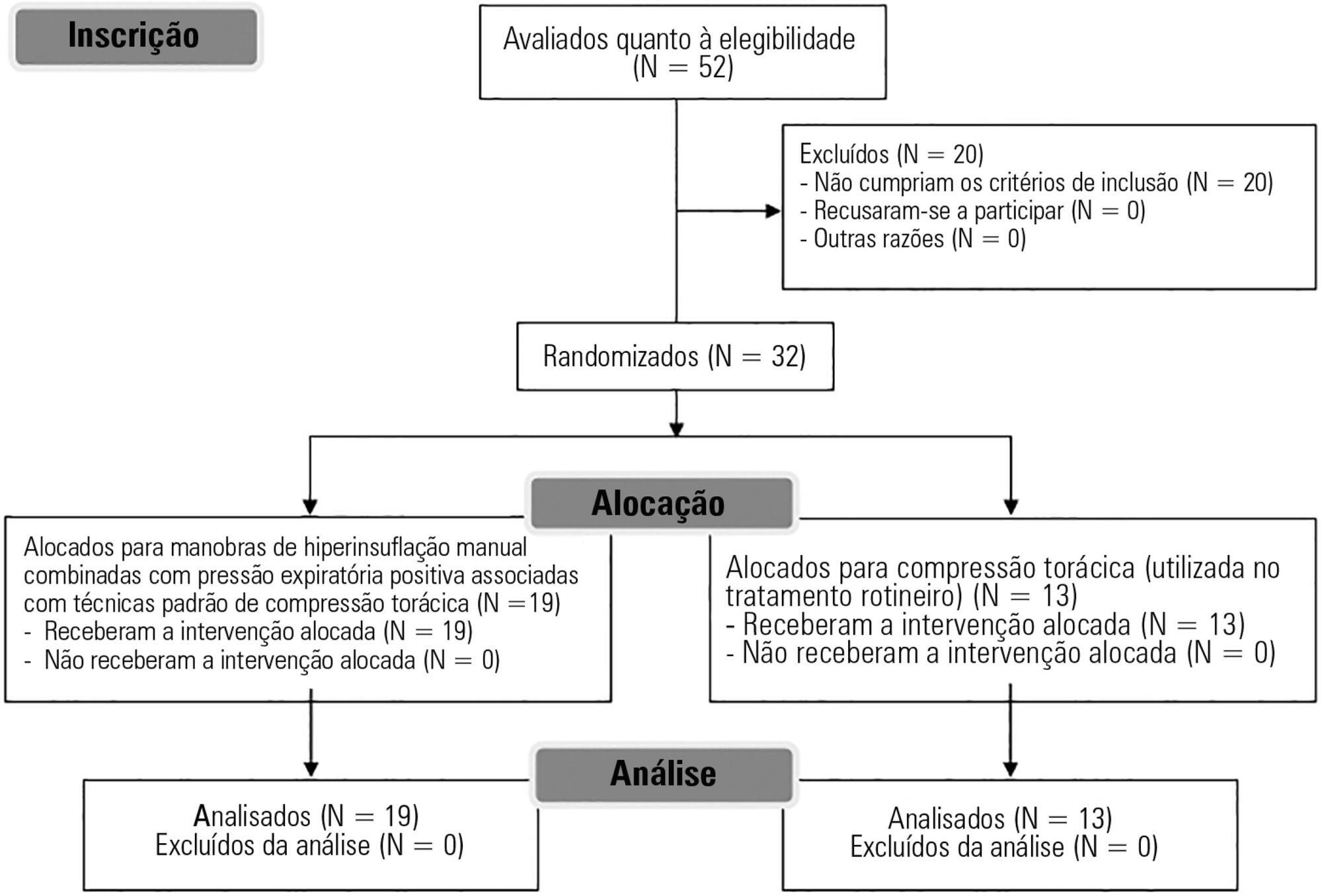
To evaluate the effects of bag-valve breathing maneuvers combined with standard manual chest compression techniques on safety, hemodynamics and oxygenation in stable septic shock patients.
A parallel, assessor-blinded, randomized trial of two groups. A computer-generated list of random numbers was prepared by an independent researcher to allocate treatments.
The Intensive Care Unit at Hospital São Lucas, Pontifícia Universidade Católica do Rio Grande do Sul.
Fifty-two subjects were assessed for eligibility, and 32 were included. All included subjects (n = 32) received the allocated intervention (n = 19 for the Experimental Group and n = 13 for the Control Group).
Twenty minutes of bag-valve breathing maneuvers combined with manual chest compression techniques (Experimental Group) or chest compression, as routinely used at our intensive care unit (Control Group). Follow-up was performed immediately after and at 30 minutes after the intervention.
Mean artery pressure.
All included subjects completed the trial (N = 32). We found no relevant effects on mean artery pressure (p = 0.17), heart rate (p = 0.50) or mean pulmonary artery pressure (p = 0.89) after adjusting for subject age and weight. Both groups were identical regarding oxygen consumption after the data adjustment (p = 0.84). Peripheral oxygen saturation tended to increase over time in both groups (p = 0.05), and there was no significant association between cardiac output and venous oxygen saturation (p = 0.813). No clinical deterioration was observed.
A single session of bag-valve breathing maneuvers combined with manual chest compression is hemodynamically safe for stable septic-shocked subjects over the short-term.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)