Abstract
Rev Bras Ter Intensiva. 2020;32(3):374-380
DOI 10.5935/0103-507X.20200065
To evaluate whether the decrease in blood pressure caused by the increase in the positive end-expiratory pressure corresponds to the pulse pressure variation as an indicator of fluid responsiveness.
This exploratory study prospectively included 24 patients with septic shock who were mechanically ventilated and subjected to three stages of elevation of the positive end-expiratory pressure: from 5 to 10cmH2O (positive end-expiratory pressure level 1), from 10 to 15cmH2O (positive end-expiratory pressure level 2), and from 15 to 20cmH2O (positive end-expiratory pressure level 3). Changes in systolic blood pressure, mean arterial pressure, and pulse pressure variation were evaluated during the three maneuvers. The patients were classified as responsive (pulse pressure variation ≥ 12%) or unresponsive to volume replacement (pulse pressure variation < 12%).
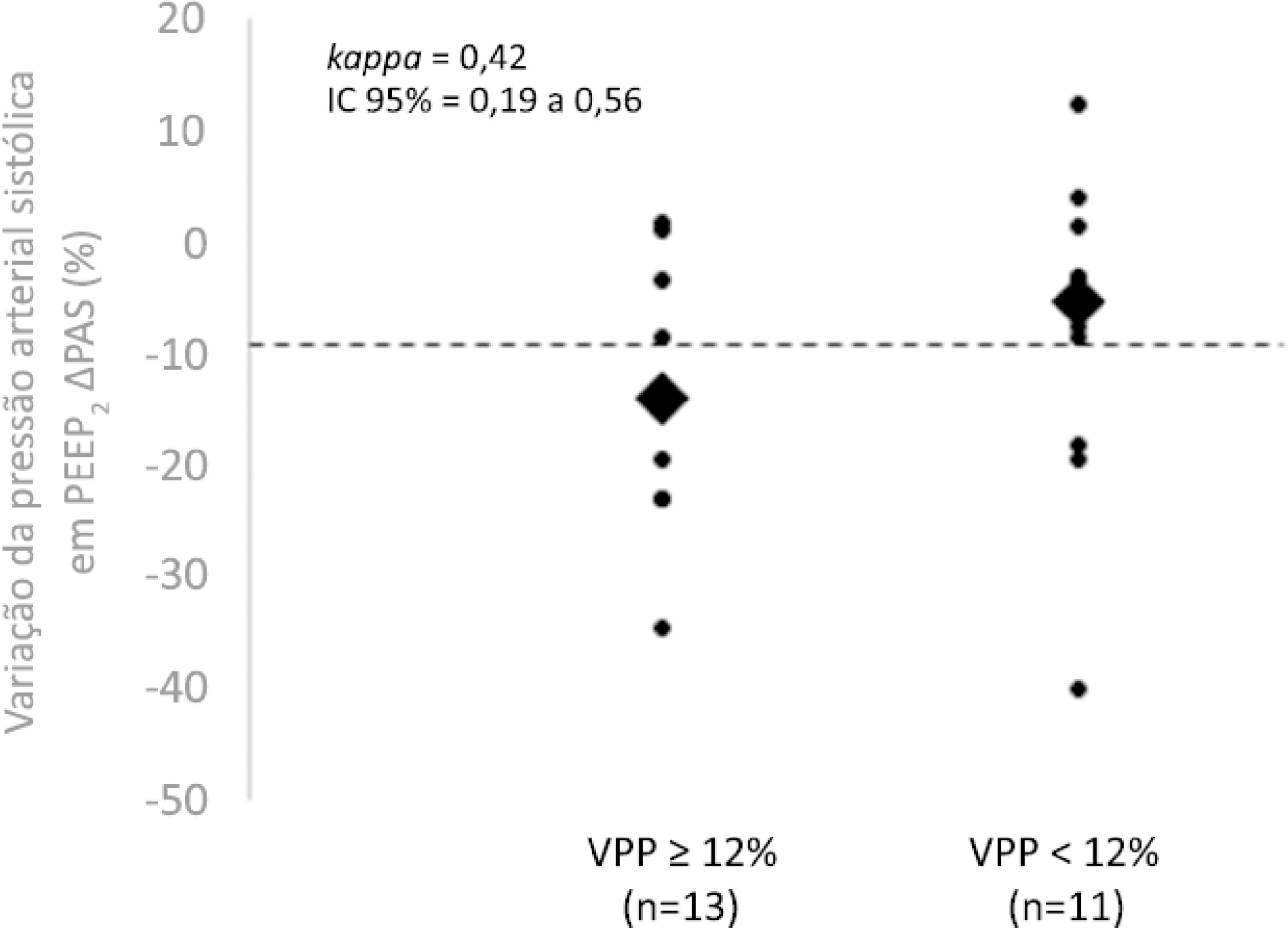
The best performance at identifying patients with pulse pressure variation ≥ 12% was observed at the positive end-expiratory pressure level 2: -9% systolic blood pressure variation (area under the curve 0.73; 95%CI: 0.49 - 0.79; p = 0.04), with a sensitivity of 63% and specificity of 80%. Concordance was low between the variable with the best performance (variation in systolic blood pressure) and pulse pressure variation ≥ 12% (kappa = 0.42; 95%CI: 0.19 - 0.56). The systolic blood pressure was < 90mmHg at positive end-expiratory pressure level 2 in 29.2% of cases and at positive end-expiratory pressure level 3 in 41.63% of cases.
Variations in blood pressure in response to the increase in positive end-expiratory pressure do not reliably reflect the behavior of the pulse pressure as a measure to identify the fluid responsiveness status.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):474-482
DOI 10.5935/0103-507X.20190073
To compare cardiac output measurements by transthoracic echocardiography and a pulmonary artery catheter in mechanically ventilated patients with high positive end-expiratory pressure. To evaluate the effect of tricuspid regurgitation.
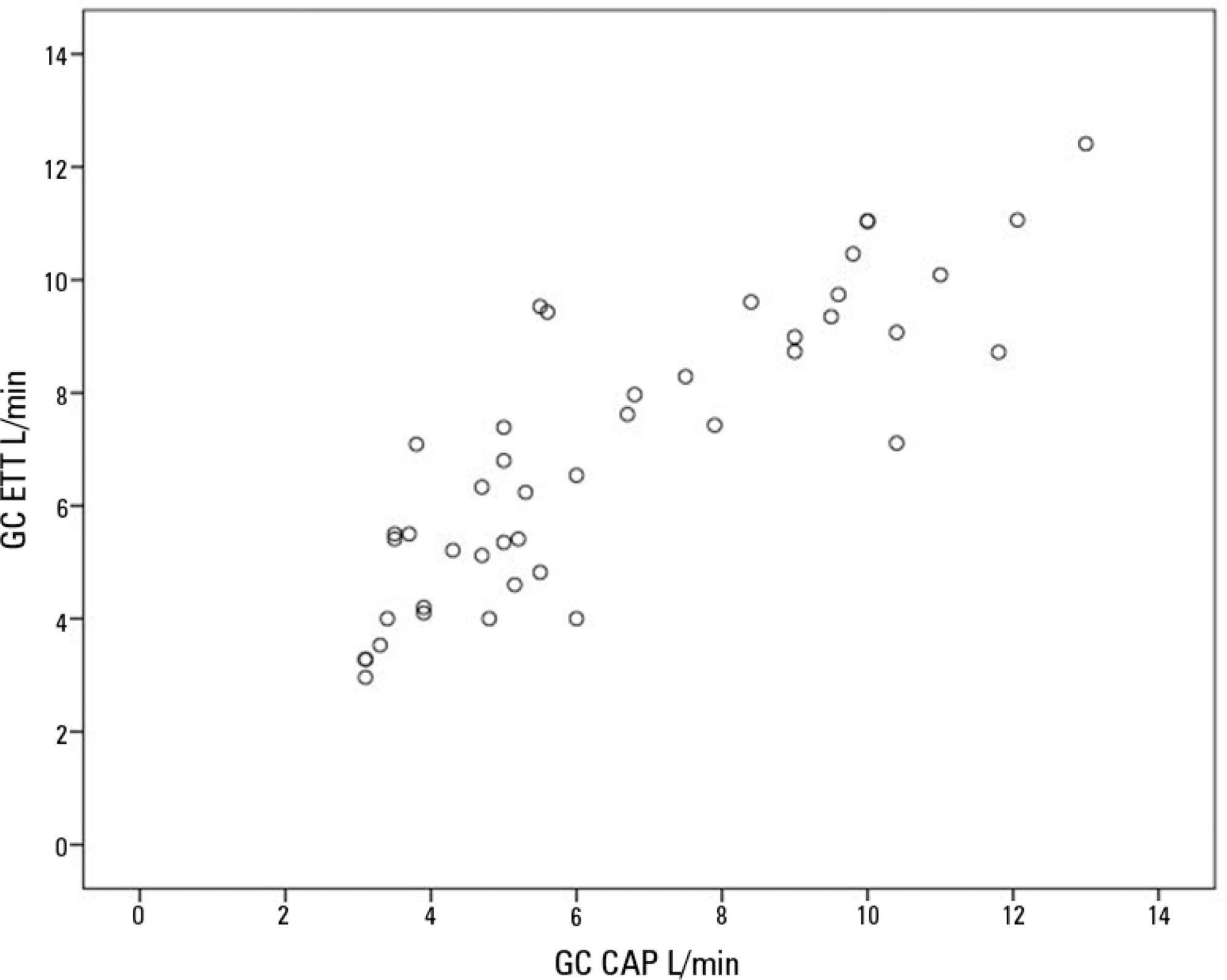
Sixteen mechanically ventilated patients were studied. Cardiac output was measured by pulmonary artery catheterization and transthoracic echocardiography. Measurements were performed at different levels of positive end-expiratory pressure (10cmH2O, 15cmH2O, and 20cmH2O). The effect of tricuspid regurgitation on cardiac output measurement was evaluated. The intraclass correlation coefficient was studied; the mean error and limits of agreement were studied with the Bland-Altman plot. The error rate was calculated.
Forty-four pairs of cardiac output measurements were obtained. An intraclass correlation coefficient of 0.908 was found (p < 0.001). The mean error was 0.44L/min for cardiac output values between 5 and 13L/min. The limits of agreement were 3.25L/min and -2.37L/min. With tricuspid insufficiency, the intraclass correlation coefficient was 0.791, and without tricuspid insufficiency, 0.935. Tricuspid insufficiency increased the error rate from 32% to 52%.
In patients with high positive end-expiratory pressure, cardiac output measurement by transthoracic echocardiography is comparable to that with a pulmonary artery catheter. Tricuspid regurgitation influences the intraclass correlation coefficient. In patients with high positive end-expiratory pressure, the use of transthoracic echocardiography to measure cardiac output is comparable to invasive measures.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):43-51
DOI 10.1590/S0103-507X2012000100007
OBJECTIVE: The objective of this study was to assess the effects of positive end-expiratory pressure on recruitment, cyclic recruitment and derecruitment and strain in patients with acute lung injury and acute respiratory distress syndrome using lung computed tomography. METHODS: This is an open, controlled, non-randomized interventional study of ten patients with acute lung injury and acute respiratory distress syndrome. Using computed tomography, single, basal slices of the lung were obtained during inspiratory and expiratory pauses at a tidal volume of 6 ml/kg and a positive end-expiratory pressure of 5, 10, 15 and 20 cmH2O. The densities of the lung parenchyma were measured in Hounsfield units. The values for positive end-expiratory pressure-induced recruitment, cyclic recruitment and derecruitment and strain were then calculated. RESULTS: Increasing levels of positive end-expiratory pressure were correlated with increased recruitment and global strain (p < 0.01), which was significantly correlated with plateau pressure (r² = 0.97, p < 0.01). In addition, increasing levels of positive end-expiratory pressure systematically increased strain along the sternovertebral axis. CONCLUSION: While strain is an adverse effect of positive end-expiratory pressure, the decision use positive end-expiratory pressure with any patient should be balanced against the potential benefits of recruitment. Due to the small number of patients in this study, the present data should be treated as hypothesis generating and is not intended to limit the clinical application of a high level of positive end-expiratory pressure in patients with severe hypoxemia.

Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)