Abstract
Crit Care Sci. 2023;35(1):107-111
DOI 10.5935/2965-2774.20230305-pt
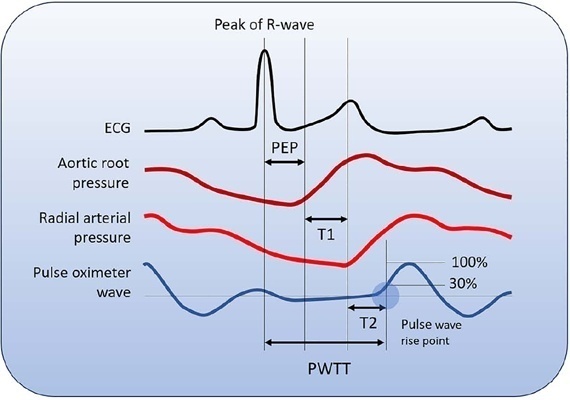
Cardiac output is an essential determinant of oxygen delivery, although unreliably measured on clinical examination and routine monitoring. Unfortunately, cardiac output monitoring is rarely performed in pediatric critical care medicine, with a limited availability of accurate methods for children. Herein, we report two pediatric cases in which noninvasive pulse-wave transit time-based cardiac output monitoring (esCCO, Nihon Kohden, Tokyo, Japan) was used. The esCCO system calculates cardiac output continuously by using the negative correlation between stroke volume and pulse wave transit time and requires only electrocardiogram monitoring, noninvasive blood pressure, and pulse oximetry signals. Before starting its use, esCCO should be calibrated, which can be done using patient information (gender, age, height, and body weight) or entering cardiac output values obtained by other methods. In both cases, when calibrations were performed using patient information, the agreement between esCCO and echocardiographic measurements was poor. However, after calibration with transthoracic echocardiography, the cardiac output values obtained by both methods remained similar after 2 hours and 18 hours. The results indicate that the esCCO system is suitable for use in children; however, further studies are needed to optimize its algorithm and determine its accuracy, precision, and trend in children.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):474-482
DOI 10.5935/0103-507X.20190073
To compare cardiac output measurements by transthoracic echocardiography and a pulmonary artery catheter in mechanically ventilated patients with high positive end-expiratory pressure. To evaluate the effect of tricuspid regurgitation.
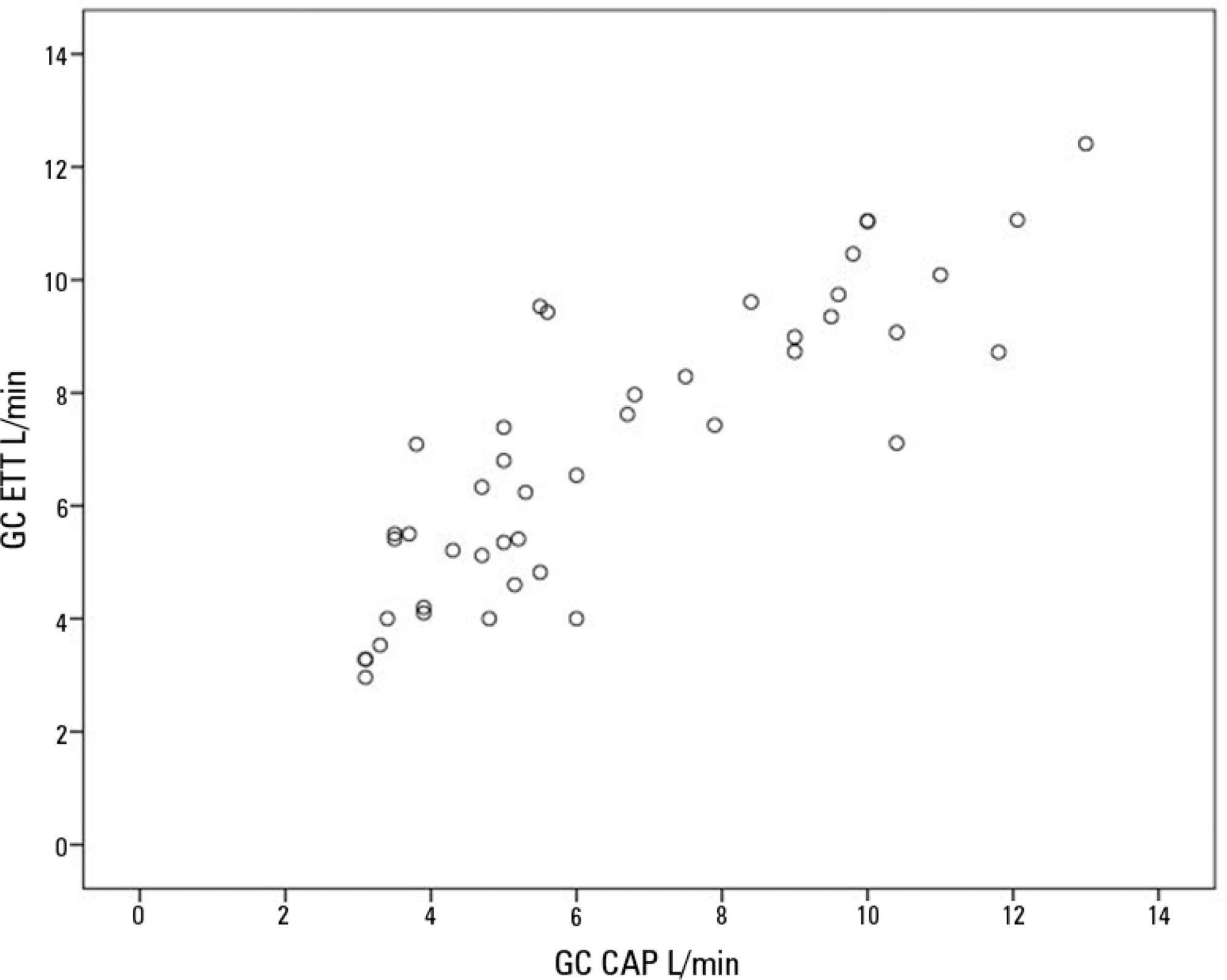
Sixteen mechanically ventilated patients were studied. Cardiac output was measured by pulmonary artery catheterization and transthoracic echocardiography. Measurements were performed at different levels of positive end-expiratory pressure (10cmH2O, 15cmH2O, and 20cmH2O). The effect of tricuspid regurgitation on cardiac output measurement was evaluated. The intraclass correlation coefficient was studied; the mean error and limits of agreement were studied with the Bland-Altman plot. The error rate was calculated.
Forty-four pairs of cardiac output measurements were obtained. An intraclass correlation coefficient of 0.908 was found (p < 0.001). The mean error was 0.44L/min for cardiac output values between 5 and 13L/min. The limits of agreement were 3.25L/min and -2.37L/min. With tricuspid insufficiency, the intraclass correlation coefficient was 0.791, and without tricuspid insufficiency, 0.935. Tricuspid insufficiency increased the error rate from 32% to 52%.
In patients with high positive end-expiratory pressure, cardiac output measurement by transthoracic echocardiography is comparable to that with a pulmonary artery catheter. Tricuspid regurgitation influences the intraclass correlation coefficient. In patients with high positive end-expiratory pressure, the use of transthoracic echocardiography to measure cardiac output is comparable to invasive measures.
Abstract
Rev Bras Ter Intensiva. 2006;18(1):63-77
DOI 10.1590/S0103-507X2006000100012
BACKGROUND AND OBJECTIVES: Monitoring of vital functions is one of the most important tools in the management of critically ill patients. Nowadays is possible to detect and analyze a great deal of physiologic data using a lot of invasive and non-invasive methods. The intensivist must be able to select and carry out the most appropriate monitoring technique according to the patient requirements and taking into account the benefit/risk ratio. Despite the fast development of non invasive monitoring techniques, invasive hemodynamic monitoring using Pulmonary Artery Catheter still is one of the basic procedures in Critical Care. The aim was to define recommendations about clinical utility of basic hemodynamic monitoring methods and the Use of Pulmonary Artery Catheter. METHODS: Modified Delphi methodology was used to create and quantify the consensus between the participants. AMIB indicated a coordinator who invited more six experts in the area of monitoring and hemodynamic support to constitute the Consensus Advisory Board. Twenty-five physicians and nurses selected from different regions of the country completed the expert panel, which reviewed the pertinent bibliography listed at the MEDLINE in the period from 1996 to 2004. RESULTS: Recommendations were made based on 55 questions about the use of central venous pressure, invasive arterial pressure, pulmonary artery catheter and its indications in different settings. CONCLUSIONS: Evaluation of central venous pressure and invasive arterial pressure, besides variables obtained by the PAC allow the understanding of cardiovascular physiology that is of great value to the care of critically ill patients. However, the correct use of these tools is fundamental to achieve the benefits due to its use.
Abstract
Rev Bras Ter Intensiva. 2006;18(1):78-85
DOI 10.1590/S0103-507X2006000100013
BACKGROUND AND OBJECTIVES: Cardiac output and preload as absolute data do not offer helpful information about the hemodynamic of critically ill patients. However, monitoring the response of these variables to volume challenge or inotropic drugs is a very useful tool in the critical care setting, particularly for patients with signs of tissue hypoperfusion. Although PAC remains the " gold standard" to measure cardiac output and preload, new and alternative technologies were developed to evaluate these hemodynamic variables. METHODS: Modified Delphi methodology was used to create and quantify the consensus between the participants. AMIB indicated a coordinator who invited more six experts in the area of monitoring and hemodynamic support to constitute the Consensus Advisory Board. Twenty three physician and two nurses selected from different regions of the country completed the expert panel, which reviewed the pertinent bibliography listed at the MEDLINE in the period from 1996 to 2004. RESULTS: Recommendations regarding the use of arterial pulse pressure variation during mechanical ventilation, continuous arterial pulse contour and lithium dilution cardiac output measurements, esophageal Doppler waveform, thoracic electrical bioimpedance, echocardiography and partial CO2 rebreathing for monitoring cardiac output and preload were created. CONCLUSIONS: The new and less invasive techniques for the measurement of cardiac output, preload or fluid responsiveness are accurate and may be an alternative to PAC in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2006;18(2):154-160
DOI 10.1590/S0103-507X2006000200009
BACKGROUND AND OBJECTIVES: The main cardiovascular function is to maintain the adequate perfusion e oxygen delivery to the cells. Physiologically, this is controlled by the cellular metabolic rate. The critically ill patients are in high danger of tissue hipoperfusion and this is directly related to cellular injury and organ dysfunction. Therefore, the tissue perfusion monitoring makes part and is indissociated of hemodynamic evaluation of the critically ill patient and is indicated to all this patients. The objective was to define recommendations about clinical utility of different tolls to bedside perfusion monitoring. METHODS: Modified Delphi methodology was used to create and quantify the consensus between the participants. AMIB indicated a coordinator who invited more six experts in the area of monitoring and hemodynamic support to constitute the Consensus Advisory Board. Twenty five physician and two nurses selected from different regions of the country completed the expert panel, which reviewed the pertinent bibliography listed at the MedLine in the period from 1996 to 2004. RESULTS: Recommendations were done about the utility of clinical monitoring of tissue perfusion, temperature gradient and transcutaneous oxygen monitoring, serum lactate, base excess, SvO² and ScvO², gastric and sublingual capnometry, CO² venous-arterial gradient and Orthogonal Polarization Spectral (OPS). CONCLUSIONS: The homodynamic compensation of a critically ill patient isn’t complete unless the tissue perfusion is corrected. Many different methods of monitoring is available and are useful in clinical practice, however, none has accuracy and effectiveness characteristics to be used independently of clinical context.
Abstract
Rev Bras Ter Intensiva. 2006;18(2):137-142
DOI 10.1590/S0103-507X2006000200006
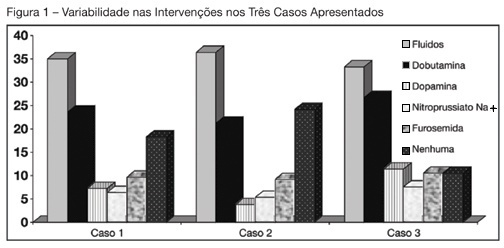
BACKGROUND AND OBJECTIVES: Use of Pulmonary Artery Catheter (PAC) is still a debatable issue, mainly due to questions raised about its security and efficacy. This study reproduced in a sample of Brazilian physicians, another one conducted amidst American doctors, in which was pointed out the heterogeneity of clinical decisions guided by data obtained from PAC. METHODS: During the Brazilian Congress of Intensive Care Medicine (Curitiba 2004), doctors were asked to answer a survey form with three vignettes. Each of them contained PAC data and one half of the surveys contained echocardiographic information. Every doctor was asked to select one of six interventions for each vignette. A homogeneous answer was considered when it was selected by at least 80% of the respondents. RESULTS: Two hundred and thirty seven doctors answered the questionnaires. They selected completely different therapeutic interventions in all three vignettes and none of the interventions achieved more than 80% agreement. Variability persisted with the choices guided by echocardiography. CONCLUSIONS: As in the original study, we observed total heterogeneity of therapeutic interventions guided by CAP and echocardiography. These results could be caused by lack of knowledge about basic pathophysiologic concepts and maybe we had to improve its teaching at the medical school benches.
Abstract
Rev Bras Ter Intensiva. 2006;18(2):161-176
DOI 10.1590/S0103-507X2006000200010
BACKGROUND AND OBJECTIVES: Shock occurs when the circulatory system cannot maintain adequate cellular perfusion. If this condition is not reverted irreversible cellular injury establishes. Shock treatment has as its initial priority the fast and vigorous correction of mean arterial pressure and cardiac output to maintain life and avoid or lessen organic dysfunctions. Fluid challenge and vasoactive drugs are necessary to warrant an adequate tissue perfusion and maintenance of function of different organs and systems, always guided by cardiovascular monitorization. The recommendations built in this consensus are aimed to guide hemodynamic support needed to maintain adequate tisular perfusion. METHODS: Modified Delphi methodology was used to create and quantify the consensus between the participants. AMIB indicated a coordinator who invited more six experts in the area of monitoring and hemodynamic support to constitute the Consensus Advisory Board. Twenty five physician and two nurses selected from different regions of the country completed the expert panel, which reviewed the pertinent bibliography listed at the MEDLINE in the period from 1996 to 2004. RESULTS: Recommendations were made answering 17 questions about hemodynamic support with focus on fluid challenge, red blood cell transfusions, vasoactive drugs and perioperative hemodynamic optimization. CONCLUSIONS: Hemodynamic monitoring by itself does not reduce the mortality of critically ill patients, however, we believe that the correct interpretation of the data obtained by the hemodynamic monitoring and the use of hemodynamic support protocols based on well defined tissue perfusion goals can improve the outcome of these patients.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)