Abstract
Crit Care Sci. 2024;36:e20240144en
DOI 10.62675/2965-2774.20240144-pt
To determine whether enteral melatonin decreases the incidence of delirium in critically ill adults.
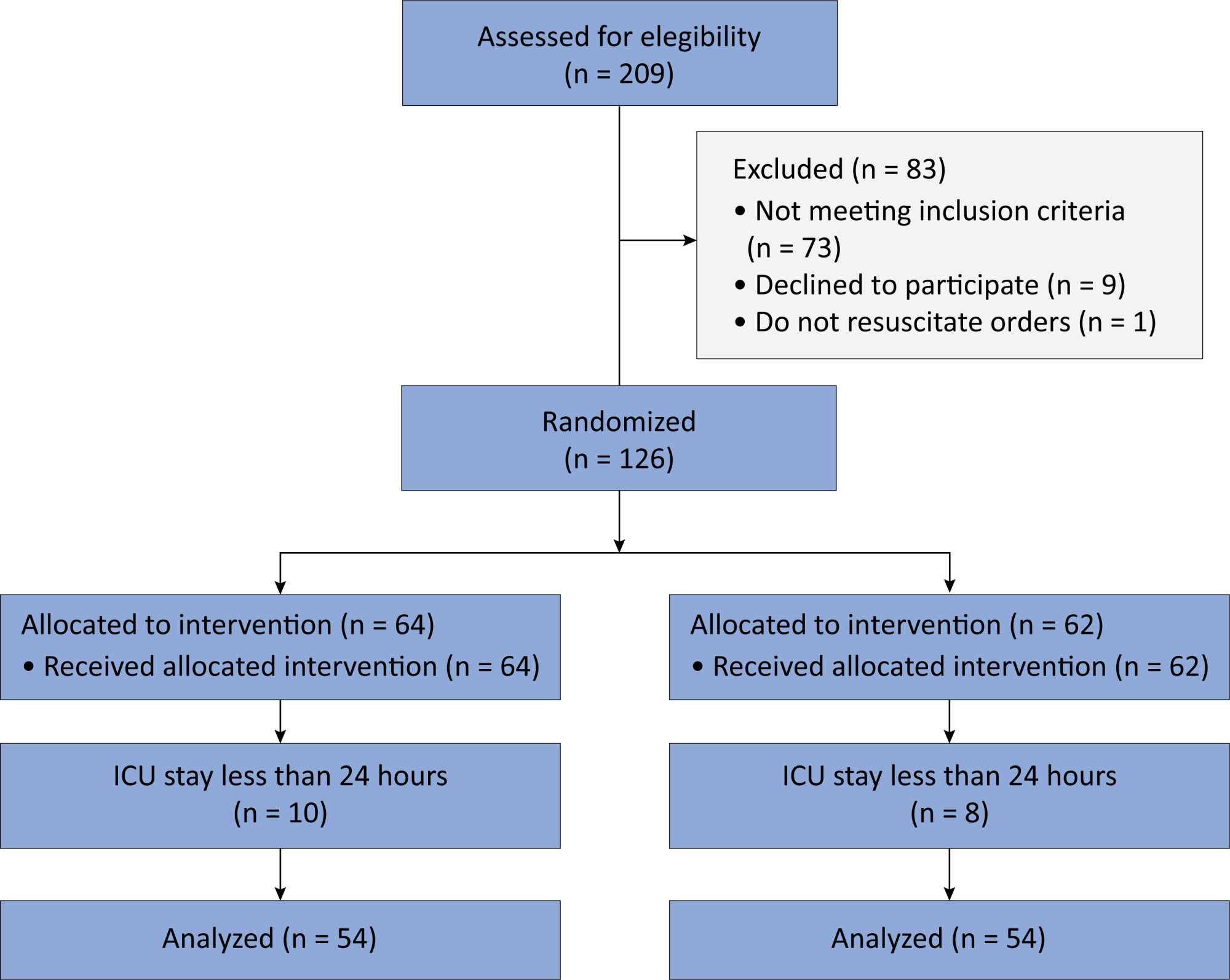
In this randomized controlled trial, adults were admitted to the intensive care unit and received either usual standard care alone (Control Group) or in combination with 3mg of enteral melatonin once a day at 9 PM (Melatonin Group). Concealment of allocation was done by serially numbered opaque sealed envelopes. The intensivist assessing delirium and the investigator performing the data analysis were blinded to the group allocation. The primary outcome was the incidence of delirium within 24 hours of the intensive care unit stay. The secondary outcomes were the incidence of delirium on Days 3 and 7, intensive care unit mortality, length of intensive care unit stay, duration of mechanical ventilation and Glasgow outcome score (at discharge).
We included 108 patients in the final analysis, with 54 patients in each group. At 24 hours of intensive care unit stay, there was no difference in the incidence of delirium between Melatonin and Control Groups (29.6 versus 46.2%; RR = 0.6; 95%CI 0.38 - 1.05; p = 0.11). No secondary outcome showed a statistically significant difference.
Enteral melatonin 3mg is not more effective at decreasing the incidence of delirium than standard care is in critically ill adults.
Abstract
Crit Care Sci. 2023;35(1):107-111
DOI 10.5935/2965-2774.20230305-pt
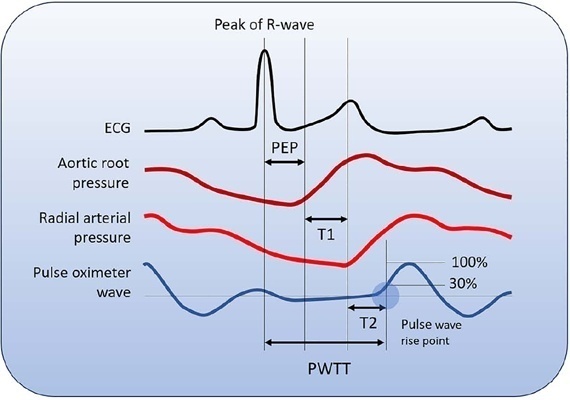
Cardiac output is an essential determinant of oxygen delivery, although unreliably measured on clinical examination and routine monitoring. Unfortunately, cardiac output monitoring is rarely performed in pediatric critical care medicine, with a limited availability of accurate methods for children. Herein, we report two pediatric cases in which noninvasive pulse-wave transit time-based cardiac output monitoring (esCCO, Nihon Kohden, Tokyo, Japan) was used. The esCCO system calculates cardiac output continuously by using the negative correlation between stroke volume and pulse wave transit time and requires only electrocardiogram monitoring, noninvasive blood pressure, and pulse oximetry signals. Before starting its use, esCCO should be calibrated, which can be done using patient information (gender, age, height, and body weight) or entering cardiac output values obtained by other methods. In both cases, when calibrations were performed using patient information, the agreement between esCCO and echocardiographic measurements was poor. However, after calibration with transthoracic echocardiography, the cardiac output values obtained by both methods remained similar after 2 hours and 18 hours. The results indicate that the esCCO system is suitable for use in children; however, further studies are needed to optimize its algorithm and determine its accuracy, precision, and trend in children.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):380-385
DOI 10.5935/0103-507X.20220224-en
To determine the incidence of postintensive care syndrome in a cohort of critically ill patients admitted to the intensive care unit and to identify risk factors related to its development in the physical, cognitive and mental health areas.
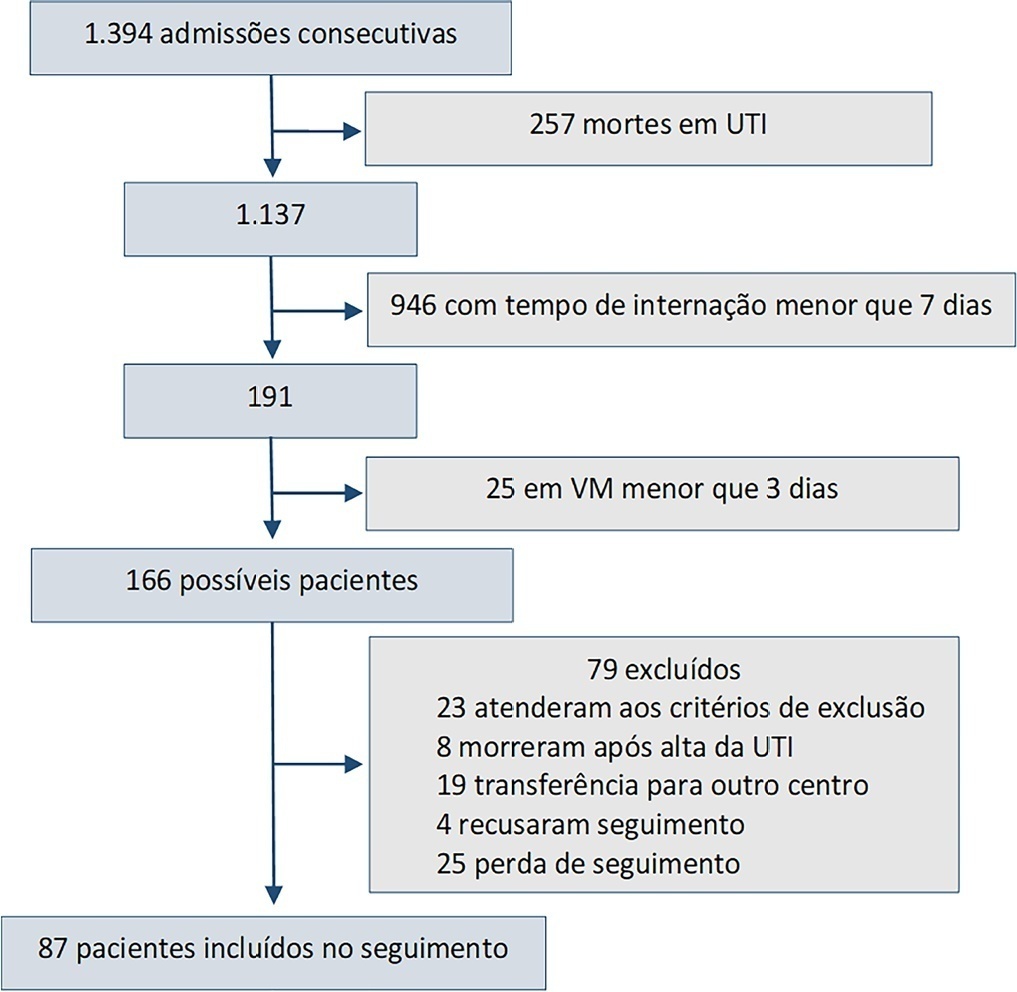
This was a prospective observational cohort study developed in the intensive care unit of a university hospital. Patients with intensive care unit stays equal to or longer than one week and the need for mechanical ventilation for more than 3 days, shock or delirium were included in the study. Demographic variables, reasons for admission, diagnoses, sedation, type of mechanical ventilation used, complications and length of stay were recorded. A univariate analysis was performed to identify risk factors related to postintensive care syndrome. The scales used for the assessment of the different spheres were Barthel, Pfeiffer, Hospital Anxiety and Depression Scale and Impact of Event Scale-6. The main variables of interest were postintensive care syndrome incidence overall and by domains. Risk factors were examined in each of the health domains (physical, cognitive and mental health).
Eighty-seven patients were included. The mean Acute Physiology and Chronic Health Evaluation II score was 16.5. The mean number of intensive care unit days was 17. The incidence of global postintensive care syndrome was 56.3% (n = 49, 95%CI 45.8 - 66.2%). The incidence of postintensive care syndrome in each of the spheres was 32.1% (physical), 11.5% (cognitive), and 36.6% (mental health).
The incidence of postintensive care syndrome is 56.3%. The mental health sphere is the most frequently involved. The risk factors are different depending on the area considered.
Abstract
Rev Bras Ter Intensiva. 2022;34(2):255-261
DOI 10.5935/0103-507X.20220023-en
To test whether tissue oxygen saturation (StO2) after a venous occlusion test estimates central venous oxygen saturation (ScvO2).
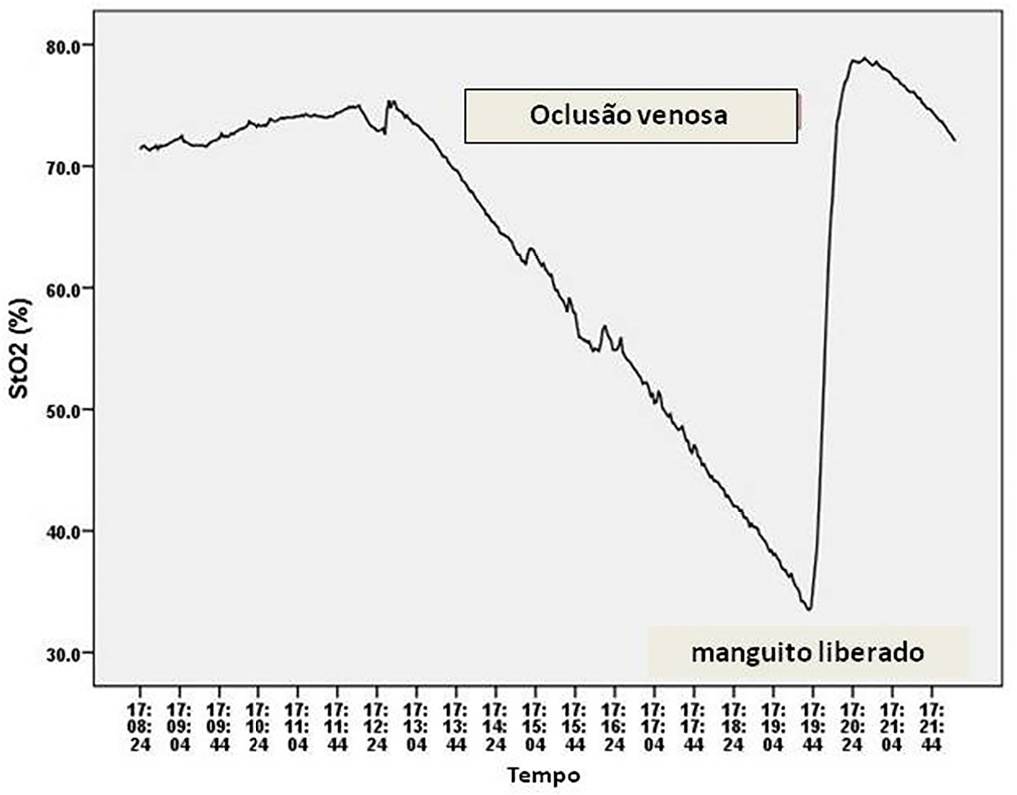
Observational study in intensive care unit patients. Tissue oxygen saturation was monitored (InSpectra Tissue Spectrometer Model 650, Hutchinson Technology Inc., MN, USA) with a multiprobe (15/25mm) in the thenar position. A venous occlusion test in volunteers was applied in the upper arm to test the tolerability and pattern of StO2 changes during the venous occlusion test. A sphygmomanometer cuff was inflated to a pressure 30mmHg above diastolic pressure until StO2 reached a plateau and deflated to 0mmHg. Tissue oxygen saturation parameters were divided into resting StO2 (r-StO2) and minimal StO2 (m-StO2) at the end of the venous occlusion test. In patients, the cuff was inflated to a pressure 30mmHg above diastolic pressure for 5 min (volunteers’ time derived) or until a StO2 plateau was reached. Tissue oxygen saturation parameters were divided into r-StO2, m-StO2, and the mean time that StO2 reached ScvO2. The StO2 value at the mean time was compared to ScvO2.
All 9 volunteers tolerated the venous occlusion test. The time for tolerability or the StO2 plateau was 7 ± 1 minutes. We studied 22 patients. The mean time for StO2 equalized ScvO2 was 100 sec and 95 sec (15/25mm probes). The StO2 value at 100 sec ([100-StO2] 15mm: 74 ± 7%; 25mm: 74 ± 6%) was then compared with ScvO2 (75 ± 6%). The StO2 value at 100 sec correlated with ScvO2 (15 mm: R2 = 0.63, 25mm: R2 = 0.67, p < 0.01) without discrepancy (Bland Altman).
Central venous oxygen saturation can be estimated from StO2 during a venous occlusion test.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):274-283
DOI 10.5935/0103-507X.20150032
To systematically review the main methods for nutritional risk assessment used in critically ill cancer patients and present the methods that better assess risks and predict relevant clinical outcomes in this group of patients, as well as to discuss the pros and cons of these methods according to the current literature.
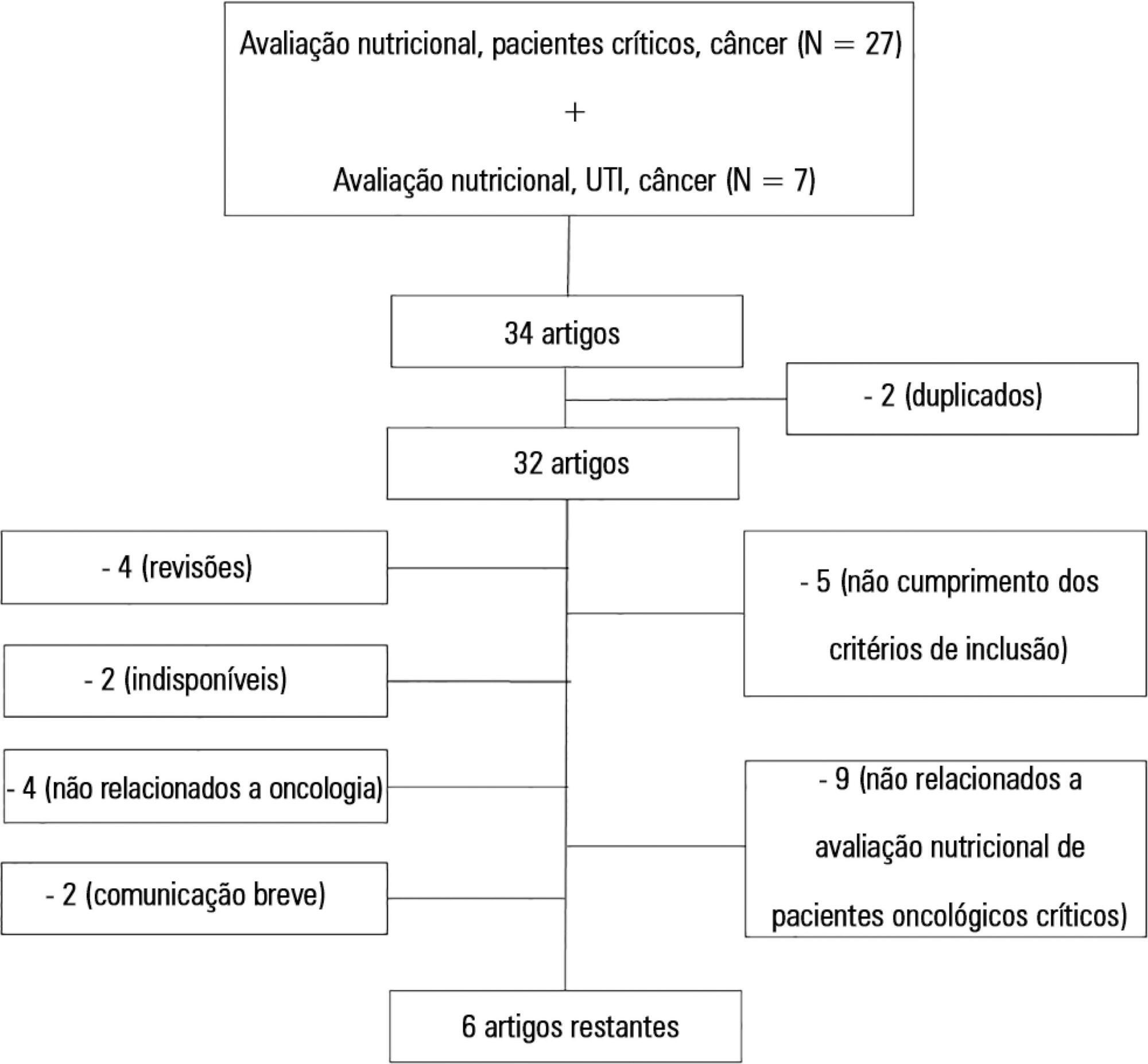
The study consisted of a systematic review based on analysis of manuscripts retrieved from the PubMed, LILACS and SciELO databases by searching for the key words “nutritional risk assessment”, “critically ill” and “cancer”.
Only 6 (17.7%) of 34 initially retrieved papers met the inclusion criteria and were selected for the review. The main outcomes of these studies were that resting energy expenditure was associated with undernourishment and overfeeding. The high Patient-Generated Subjective Global Assessment score was significantly associated with low food intake, weight loss and malnutrition. In terms of biochemical markers, higher levels of creatinine, albumin and urea were significantly associated with lower mortality. The worst survival was found for patients with worse Eastern Cooperative Oncologic Group - performance status, high Glasgow Prognostic Score, low albumin, high Patient-Generated Subjective Global Assessment score and high alkaline phosphatase levels. Geriatric Nutritional Risk Index values < 87 were significantly associated with mortality. A high Prognostic Inflammatory and Nutritional Index score was associated with abnormal nutritional status in critically ill cancer patients. Among the reviewed studies that examined weight and body mass index alone, no significant clinical outcome was found.
None of the methods reviewed helped to define risk among these patients. Therefore, assessment by a combination of weight loss and serum measurements, preferably in combination with other methods using scores such as Eastern Cooperative Oncologic Group - performance status, Glasgow Prognostic Score and Patient-Generated Subjective Global Assessment, is suggested given that their use is simple, feasible and useful in such cases.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):143-147
DOI 10.5935/0103-507X.20140021
To evaluate the behavior of fractional excretion of potassium in the course of acute kidney injury in critically ill patients.
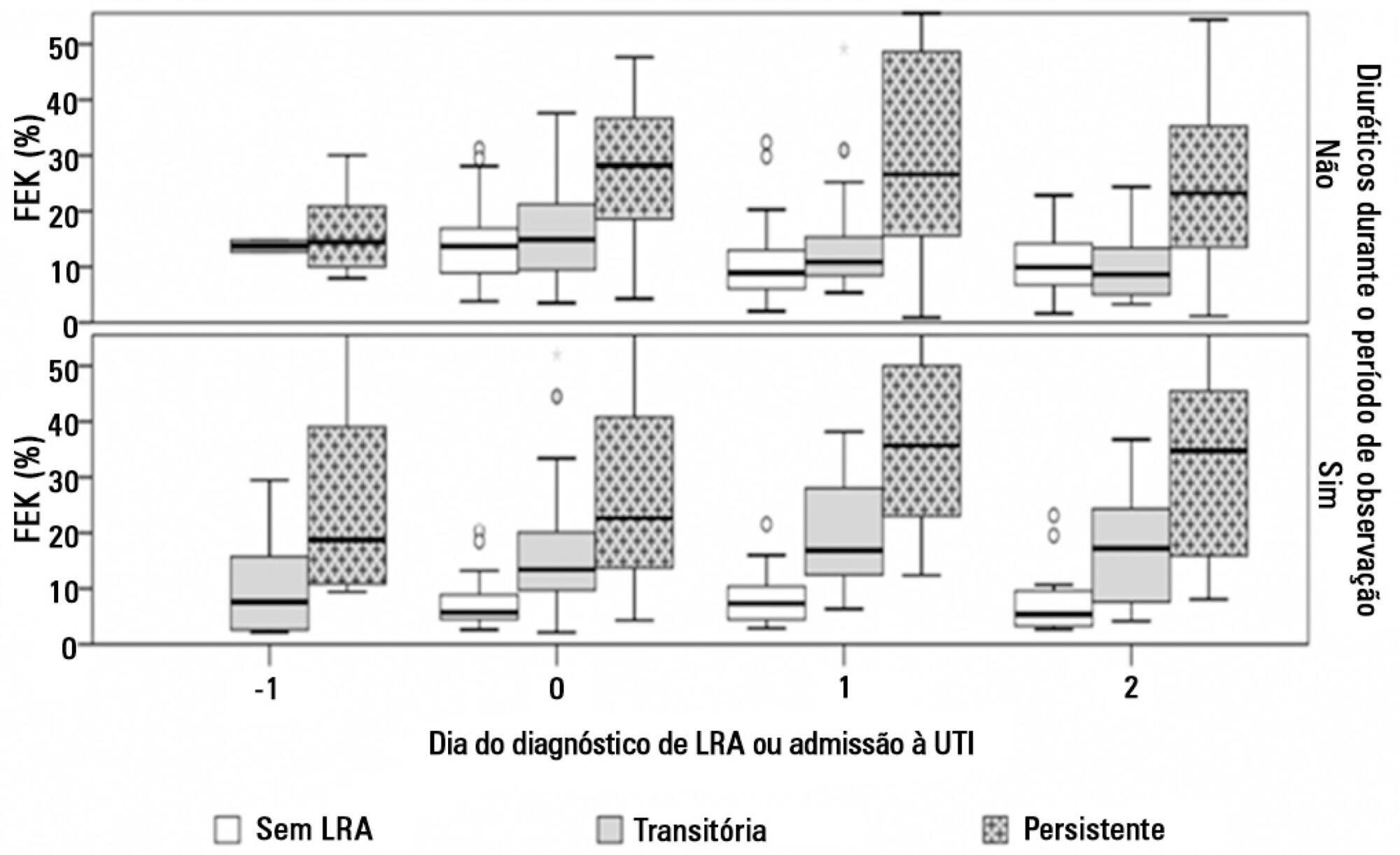
As part of a larger study in which we have evaluated blood and urinary parameters in the course of acute kidney injury, 168 patients were included. Blood and urine samples were collected daily until the removal of the urinary catheter or the initiation of renal replacement therapy. We describe the evolution of fractional excretion of potassium based on whether acute kidney injury was diagnosed, its duration (transient or persistent) and its severity (creatinine-based Acute Kidney Injury Network - AKIN stage). The diagnostic performance of fractional excretion of potassium in predicting the duration of acute kidney injury and the need for renal replacement therapy on the day of acute kidney injury diagnosis was also evaluated.
Fractional excretion of potassium was significantly higher in persistent acute kidney injury compared to transient acute kidney injury on the day of acute kidney injury diagnosis (24.8 vs. 13.8%, p<0.001). Both groups had the median fractional excretion of potassium increasing in the two days preceding the acute kidney injury diagnosis. Patients without acute kidney injury had stable low fractional excretion of potassium values. The fractional excretion of potassium was fairly accurate in predicting persistent acute kidney injury (area under the curve: 0.712; 95% confidence interval: 0.614-0.811; p<0.001) on the day of acute kidney injury diagnosis. The area under the curve was 0.663 (95% confidence interval: 0.523-0.803; p=0.03) for renal replacement therapy. The fractional excretion of potassium increased with maximum AKIN stage reached, in both transient and persistent acute kidney injury.
Sequential fractional excretion of potassium assessment appears to be useful in critically ill patients at risk for acute kidney injury.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (33) COVID-19 (45) Critical care (115) Critical illness (54) ICU (25) Infant, newborn (27) Intensive care (72) Intensive care units (254) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (75) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (117) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)