You searched for:"Alexandre Toledo Maciel"
We found (9) results for your search.-
Original Article
Metabolic acid-base adaptation triggered by acute persistent hypercapnia in mechanically ventilated patients with acute respiratory distress syndrome
Rev Bras Ter Intensiva. 2016;28(1):19-26
Abstract
Original ArticleMetabolic acid-base adaptation triggered by acute persistent hypercapnia in mechanically ventilated patients with acute respiratory distress syndrome
Rev Bras Ter Intensiva. 2016;28(1):19-26
DOI 10.5935/0103-507X.20160009
Views0ABSTRACT
Objective:
Hypercapnia resulting from protective ventilation in acute respiratory distress syndrome triggers metabolic pH compensation, which is not entirely characterized. We aimed to describe this metabolic compensation.
Methods:
The data were retrieved from a prospective collected database. Variables from patients’ admission and from hypercapnia installation until the third day after installation were gathered. Forty-one patients with acute respiratory distress syndrome were analyzed, including twenty-six with persistent hypercapnia (PaCO2 > 50mmHg > 24 hours) and 15 non-hypercapnic (control group). An acid-base quantitative physicochemical approach was used for the analysis.
Results:
The mean ages in the hypercapnic and control groups were 48 ± 18 years and 44 ± 14 years, respectively. After the induction of hypercapnia, pH markedly decreased and gradually improved in the ensuing 72 hours, consistent with increases in the standard base excess. The metabolic acid-base adaptation occurred because of decreases in the serum lactate and strong ion gap and increases in the inorganic apparent strong ion difference. Furthermore, the elevation in the inorganic apparent strong ion difference occurred due to slight increases in serum sodium, magnesium, potassium and calcium. Serum chloride did not decrease for up to 72 hours after the initiation of hypercapnia.
Conclusion:
In this explanatory study, the results indicate that metabolic acid-base adaptation, which is triggered by acute persistent hypercapnia in patients with acute respiratory distress syndrome, is complex. Furthermore, further rapid increases in the standard base excess of hypercapnic patients involve decreases in serum lactate and unmeasured anions and increases in the inorganic apparent strong ion difference by means of slight increases in serum sodium, magnesium, calcium, and potassium. Serum chloride is not reduced.
Keywords:Acid-base equilibriumAcidosis, respiratoryIntensive care unitsRespiration, artificialRespiratory distress syndrome, adultSee more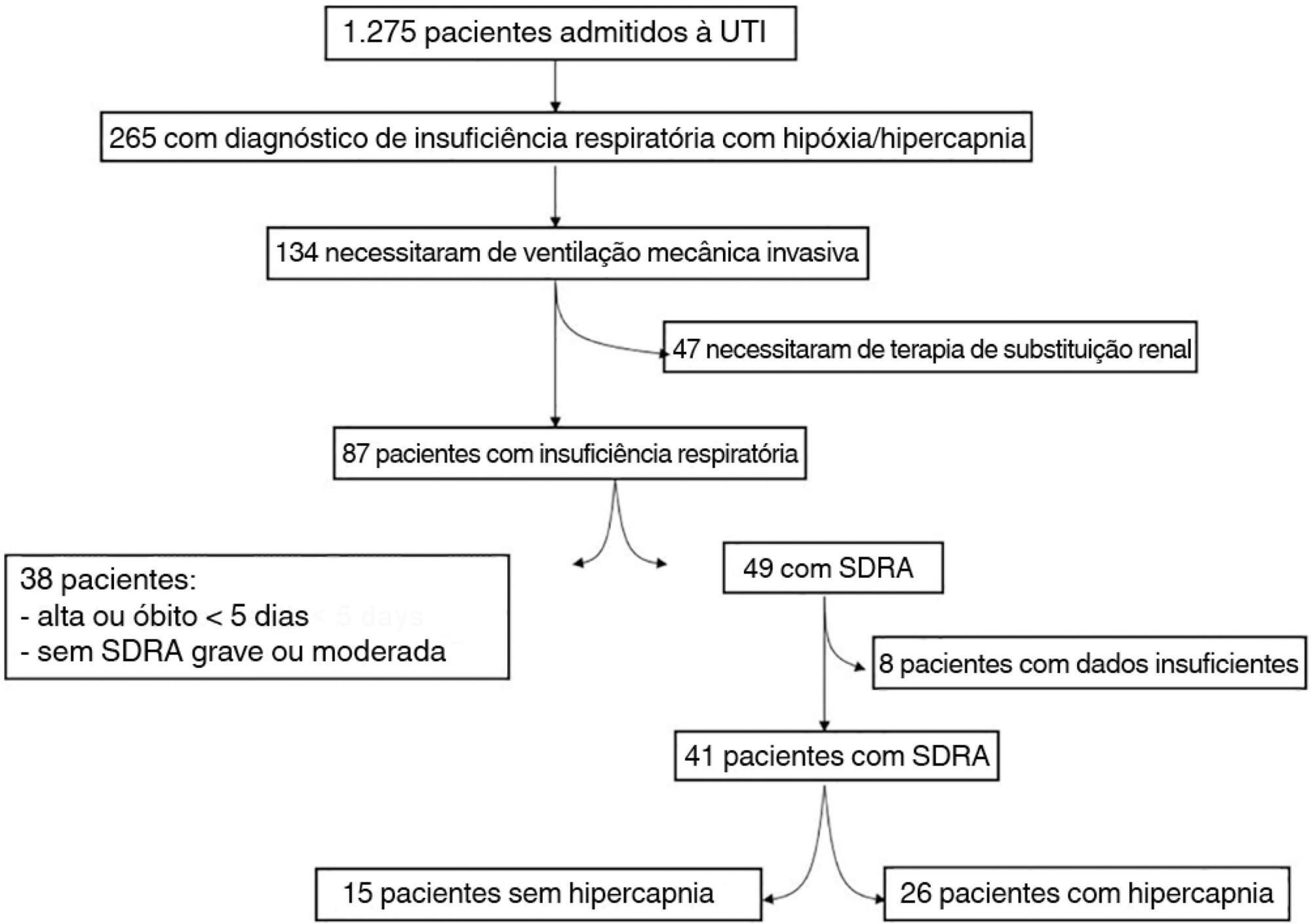
-
Original Articles
Fractional excretion of potassium in the course of acute kidney injury in critically ill patients: potential monitoring tool?
Rev Bras Ter Intensiva. 2014;26(2):143-147
Abstract
Original ArticlesFractional excretion of potassium in the course of acute kidney injury in critically ill patients: potential monitoring tool?
Rev Bras Ter Intensiva. 2014;26(2):143-147
DOI 10.5935/0103-507X.20140021
Views0See moreObjective:
To evaluate the behavior of fractional excretion of potassium in the course of acute kidney injury in critically ill patients.
Methods:
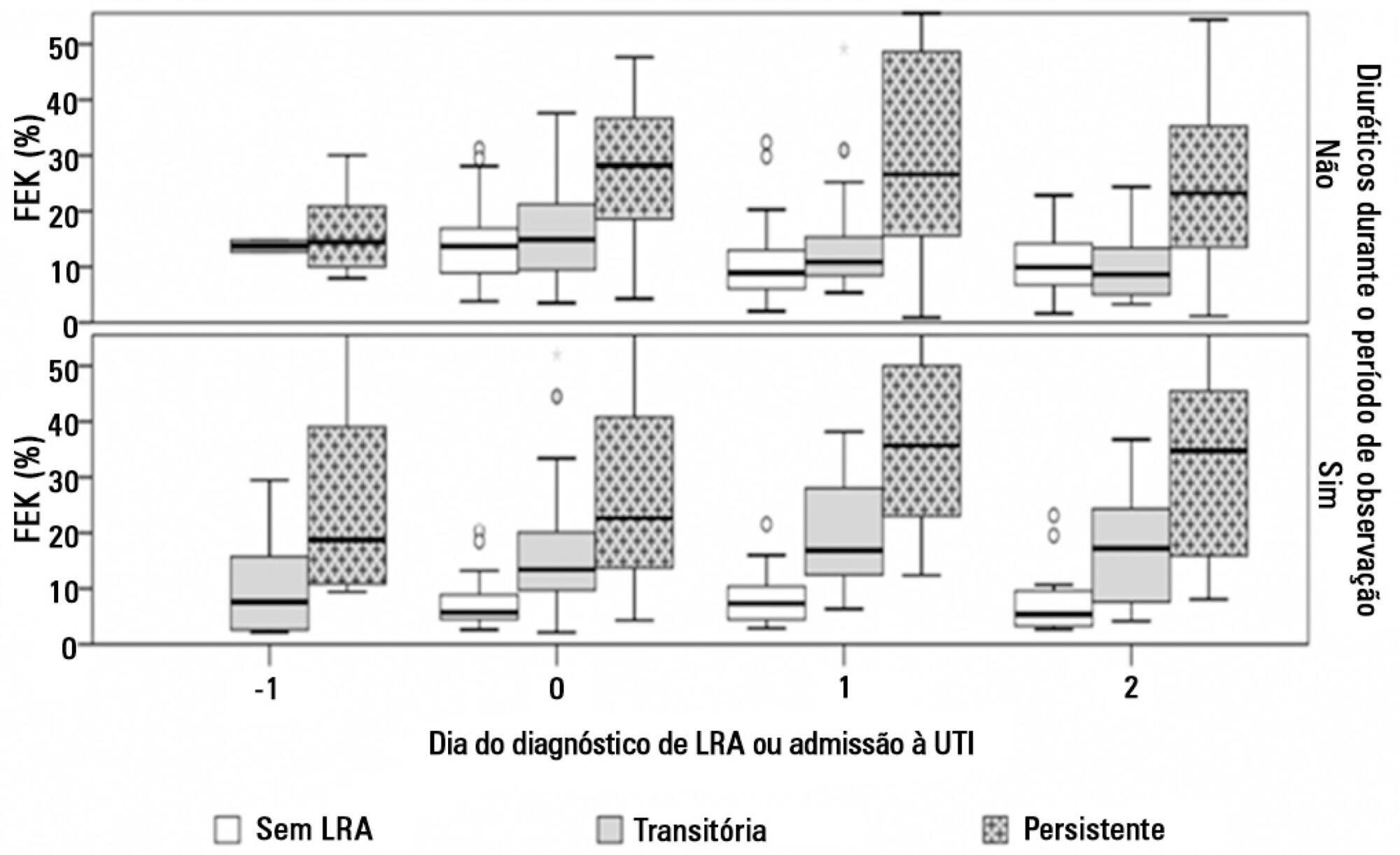
As part of a larger study in which we have evaluated blood and urinary parameters in the course of acute kidney injury, 168 patients were included. Blood and urine samples were collected daily until the removal of the urinary catheter or the initiation of renal replacement therapy. We describe the evolution of fractional excretion of potassium based on whether acute kidney injury was diagnosed, its duration (transient or persistent) and its severity (creatinine-based Acute Kidney Injury Network – AKIN stage). The diagnostic performance of fractional excretion of potassium in predicting the duration of acute kidney injury and the need for renal replacement therapy on the day of acute kidney injury diagnosis was also evaluated.
Results:
Fractional excretion of potassium was significantly higher in persistent acute kidney injury compared to transient acute kidney injury on the day of acute kidney injury diagnosis (24.8 vs. 13.8%, p<0.001). Both groups had the median fractional excretion of potassium increasing in the two days preceding the acute kidney injury diagnosis. Patients without acute kidney injury had stable low fractional excretion of potassium values. The fractional excretion of potassium was fairly accurate in predicting persistent acute kidney injury (area under the curve: 0.712; 95% confidence interval: 0.614-0.811; p<0.001) on the day of acute kidney injury diagnosis. The area under the curve was 0.663 (95% confidence interval: 0.523-0.803; p=0.03) for renal replacement therapy. The fractional excretion of potassium increased with maximum AKIN stage reached, in both transient and persistent acute kidney injury.
Conclusion:
Sequential fractional excretion of potassium assessment appears to be useful in critically ill patients at risk for acute kidney injury.
-
Commentaries
New concepts for bringing urine biochemistry back to clinical practice in the intensive care unit
Rev Bras Ter Intensiva. 2014;26(4):330-332
Abstract
CommentariesNew concepts for bringing urine biochemistry back to clinical practice in the intensive care unit
Rev Bras Ter Intensiva. 2014;26(4):330-332
DOI 10.5935/0103-507X.20140049
Views0INTRODUCTIONIn the last few years, great attention has been given to the composition of the fluids that are administered to critically ill patients.(,) In particular, the amount of Na+ and Cl– is of paramount relevance because these two electrolytes are major determinants of the strong ion difference (SID) in the blood, which is the most […]See more -
Editorial
Urine assessment in the critically ill: a matter of both quantity and quality
Rev Bras Ter Intensiva. 2013;25(3):184-185
Abstract
EditorialUrine assessment in the critically ill: a matter of both quantity and quality
Rev Bras Ter Intensiva. 2013;25(3):184-185
DOI 10.5935/0103-507X.20130032
Views0In this issue of Revista Brasileira de Terapia Intensiva, Masevicius et al.( ) reported on the behavior of the plasma chloride concentration ([Cl–]plasma) of 148 consecutive postoperative patients in the first 24 hours after their intensive care unit (ICU) admission. The authors’ major finding was that, at the end of the first day in the […]See more -
Original Articles
Anion gap corrected for albumin, phosphate and lactate is a good predictor of strong ion gap in critically ill patients: a nested cohort study
Rev Bras Ter Intensiva. 2013;25(3):205-211
Abstract
Original ArticlesAnion gap corrected for albumin, phosphate and lactate is a good predictor of strong ion gap in critically ill patients: a nested cohort study
Rev Bras Ter Intensiva. 2013;25(3):205-211
DOI 10.5935/0103-507X.20130036
Views1OBJECTIVE:
Corrected anion gap and strong ion gap are commonly used to estimate unmeasured anions. We evaluated the performance of the anion gap corrected for albumin, phosphate and lactate in predicting strong ion gap in a mixed population of critically ill patients. We hypothesized that anion gap corrected for albumin, phosphate and lactate would be a good predictor of strong ion gap, independent of the presence of metabolic acidosis. In addition, we evaluated the impact of strong ion gap at admission on hospital mortality.
METHODS:
We included 84 critically ill patients. Correlation and agreement between the anion gap corrected for albumin, phosphate and lactate and strong ion gap was evaluated by the Pearson correlation test, linear regression, a Bland-Altman plot and calculating interclass correlation coefficient. Two subgroup analyses were performed: one in patients with base-excess <-2mEq/L (low BE group - lBE) and the other in patients with base-excess >-2mEq/L (high BE group – hBE). A logistic regression was performed to evaluate the association between admission strong ion gap levels and hospital mortality.
RESULTS:
There was a very strong correlation and a good agreement between anion gap corrected for albumin, phosphate and lactate and strong ion gap in the general population (r2=0.94; bias 1.40; limits of agreement -0.75 to 3.57). Correlation was also high in the lBE group (r2=0.94) and in the hBE group (r2=0.92). High levels of strong ion gap were present in 66% of the whole population and 42% of the cases in the hBE group. Strong ion gap was not associated with hospital mortality by logistic regression.
CONCLUSION:
Anion gap corrected for albumin, phosphate and lactate and strong ion gap have an excellent correlation. Unmeasured anions are frequently elevated in critically ill patients with normal base-excess. However, there was no association between unmeasured anions and hospital mortality.
Keywords:Acid-base equilibrium/ physiologyBlood chemical analysisCritical illnessLactate/bloodPhosphate/ bloodPrognosisSerum albumin/bloodSee more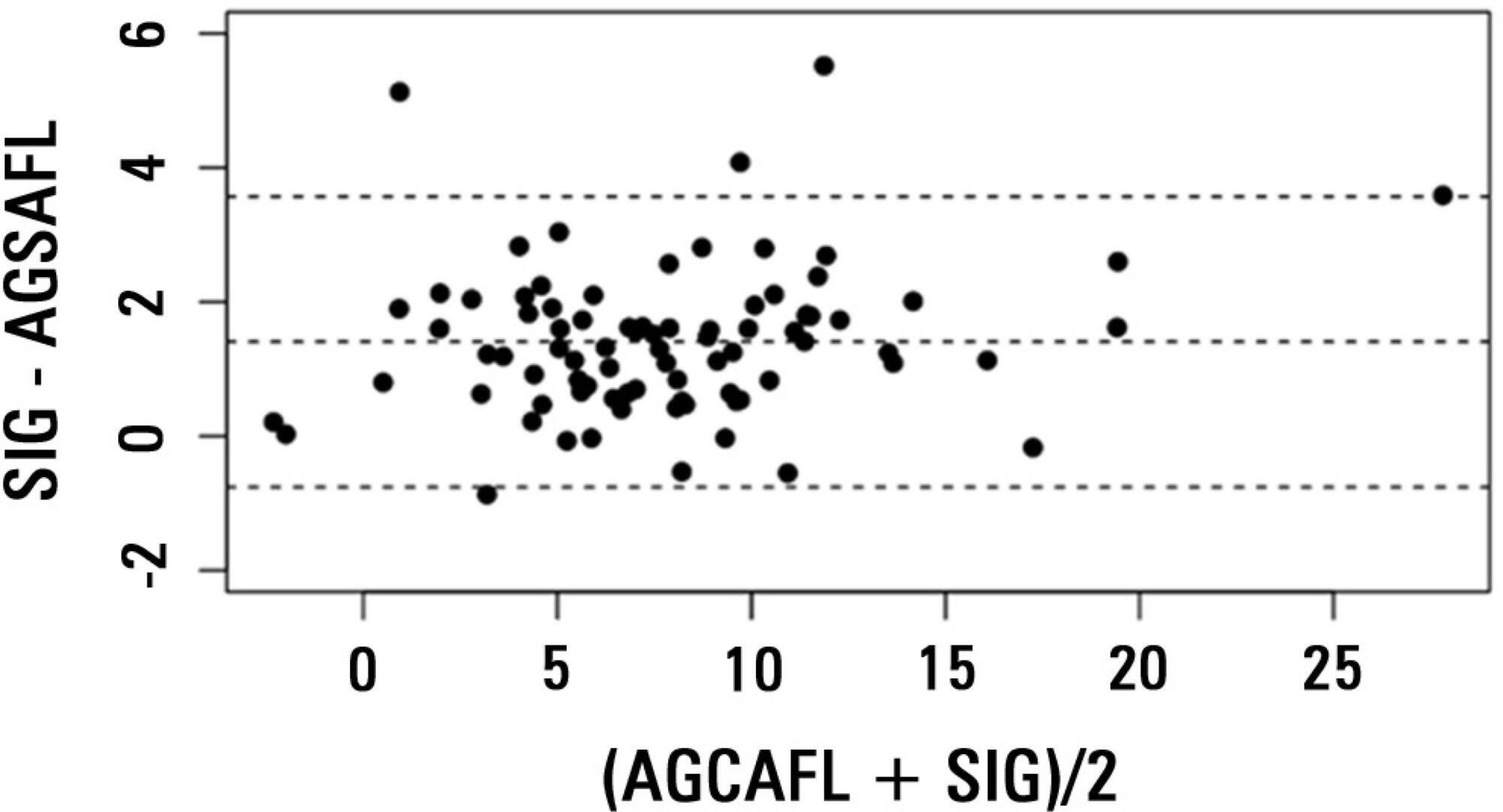
-
Original Articles – Clinical Research
Urinary electrolyte monitoring in critically ill patients: a preliminary observational study
Rev Bras Ter Intensiva. 2012;24(3):236-245
Abstract
Original Articles – Clinical ResearchUrinary electrolyte monitoring in critically ill patients: a preliminary observational study
Rev Bras Ter Intensiva. 2012;24(3):236-245
DOI 10.1590/S0103-507X2012000300006
Views0OBJECTIVE: Intensive care unit survivors and non-survivors have distinct acid-base profiles. The kidney’s regulation of urinary electrolytes and the urinary strong ion difference plays a major role in acid-base homeostasis. The aim of this study was to evaluate the potential utility of daily spot urinary electrolyte measurement in acid-base and renal function monitoring. METHODS: We prospectively recorded daily plasma acid-base parameters and traditional markers of renal function in parallel with spot urinary electrolyte measurements in patients with urinary catheters admitted to our intensive care unit. Patients who remained in the intensive care unit for at least 4 days with a urinary catheter were included in the study. RESULTS: Of the 50 patients included in the study, 22% died during their intensive care unit stay. The incidence of acute kidney injury was significantly higher in non-survivors during the 4-day observation period (64% vs. 18% in survivors). Urinary chloride and sodium were lower and urinary strong ion difference was higher on day 1 in patients who developed acute kidney injury among both survivors and non-survivors. Both groups had similar urine output, although non-survivors had persistently higher urinary strong ion difference on all days. Survivors had a progressive improvement in metabolic acid-base profile due to increases in the plasma strong ion difference and decreases in weak acids. These changes were concomitant with decreases in urinary strong ion difference. In non-survivors, acid-base parameters did not significantly change during follow-up. CONCLUSIONS: Daily assessment of spot urinary electrolytes and strong ion difference are useful components of acid-base and renal function evaluations in critically ill patients, having distinct profiles between intensive care unit survivors and non-survivors.
Keywords:AcidosisAcute kidney injuryCritical careMonitoring, physiologicPrognosisWater-electrolyte imbalanceSee more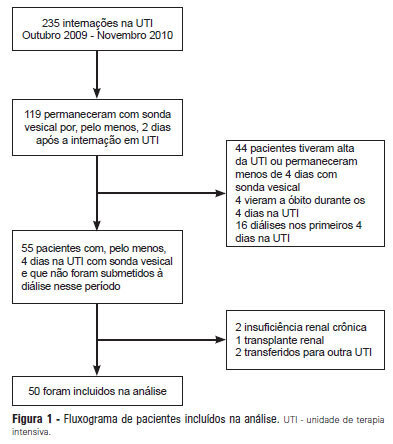
-
Original Articles – Basic Research
Acute hemodynamic, respiratory and metabolic alterations after blood contact with a volume priming and extracorporeal life support circuit: an experimental study
Rev Bras Ter Intensiva. 2012;24(2):137-142
Abstract
Original Articles – Basic ResearchAcute hemodynamic, respiratory and metabolic alterations after blood contact with a volume priming and extracorporeal life support circuit: an experimental study
Rev Bras Ter Intensiva. 2012;24(2):137-142
DOI 10.1590/S0103-507X2012000200007
Views0OBJECTIVE: To investigate the hemodynamic, respiratory and metabolic impact of blood contact with a priming volume and extracorporeal membrane oxygenation circuit, before the initiation of oxygenation and ventilation METHODS: Five animals were instrumented and submitted to extracorporeal membrane oxygenation. Data were collected at the baseline and 30 minutes after starting extracorporeal circulation, without membrane ventilatory (sweeper) flow. RESULTS: After starting extracorporeal membrane oxygenation, there was a non-significant elevation in pulmonary vascular resistance from 235 (178,303) to 379 (353,508) dyn.seg.(cm5)-1 (P=0.065), associated with an elevation in the alveolar arterial oxygen gradient from 235 (178,303) to 379 (353,508) mmHg (P=0.063). We also observed a reduction in the left ventricle stroke work from 102 (94,105) to 78 (71,87) (mL.mmHg)/beat (P=0.064), in addition to a reduction in cardiac output from 7.2 (6.8,7.6) to 5.9 (5.8,6.3) L/min (P=0.188). The right ventricle stroke work was counterbalanced between the pulmonary vascular resistance increment and the cardiac output reduction, maintaining a similar value. CONCLUSIONS: We presented an experimental model that is feasible and safe. Blood contact with the priming volume and extracorporeal membrane oxygenation circuit resulted in non-significant systemic or metabolic changes.
Keywords:acute respiratory distress syndromeExtracorporeal membrane oxygenationMultiple organ failureRespiration, artificialSwineSee more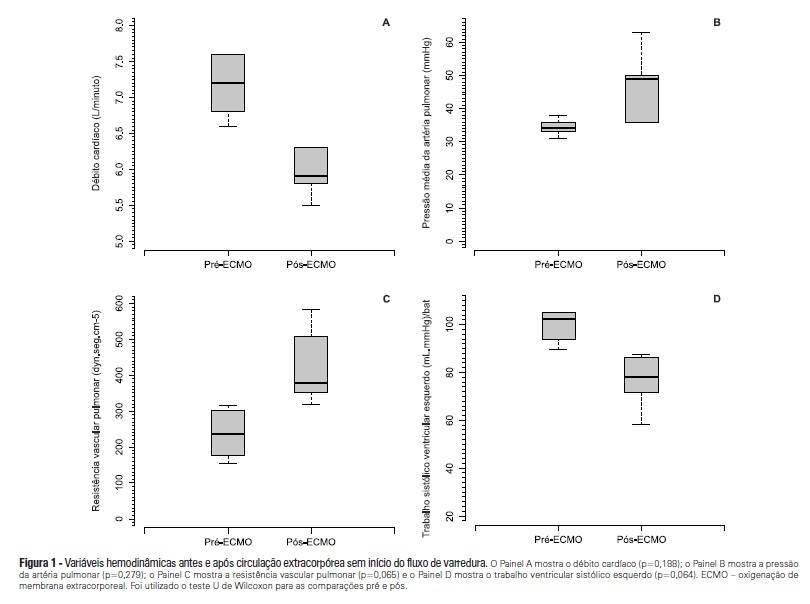
-
Case Reports
Hemodynamic and respiratory support using venoarterial extracorporeal membrane oxygenation (ECMO) in a polytrauma patient
Rev Bras Ter Intensiva. 2011;23(3):374-379
Abstract
Case ReportsHemodynamic and respiratory support using venoarterial extracorporeal membrane oxygenation (ECMO) in a polytrauma patient
Rev Bras Ter Intensiva. 2011;23(3):374-379
DOI 10.1590/S0103-507X2011000300017
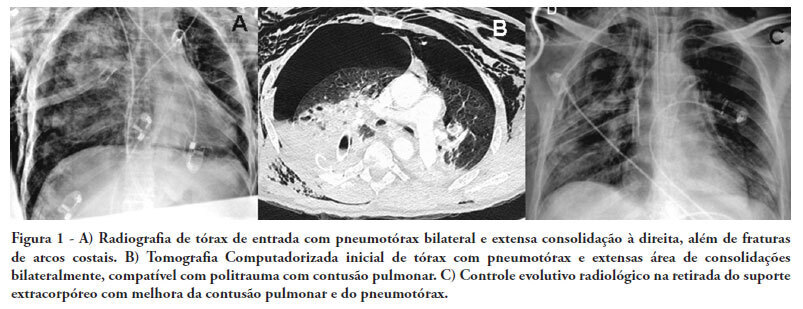
Views0See moreThere are few reports in the literature regarding the use of venoarterial extracorporeal membrane oxygenation (ECMO) for double-dysfunction from both heart and lung contusions in polytrauma patients. This article reports a 48-year-old patient admitted after a traffic accident. He rapidly progressed to shock with low cardiac output due to myocardial contusion and refractory hypoxemia due to pulmonary contusion, an unstable chest wall and bilateral pneumothorax. ECMO was an effective rescue procedure in this dramatic situation and was successfully discontinued on the fourth day after the trauma. The patient also developed an extensive brain infarction and eventually died on the seventh day after admission
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




