Abstract
Rev Bras Ter Intensiva. 2022;34(2):255-261
DOI 10.5935/0103-507X.20220023-en
To test whether tissue oxygen saturation (StO2) after a venous occlusion test estimates central venous oxygen saturation (ScvO2).
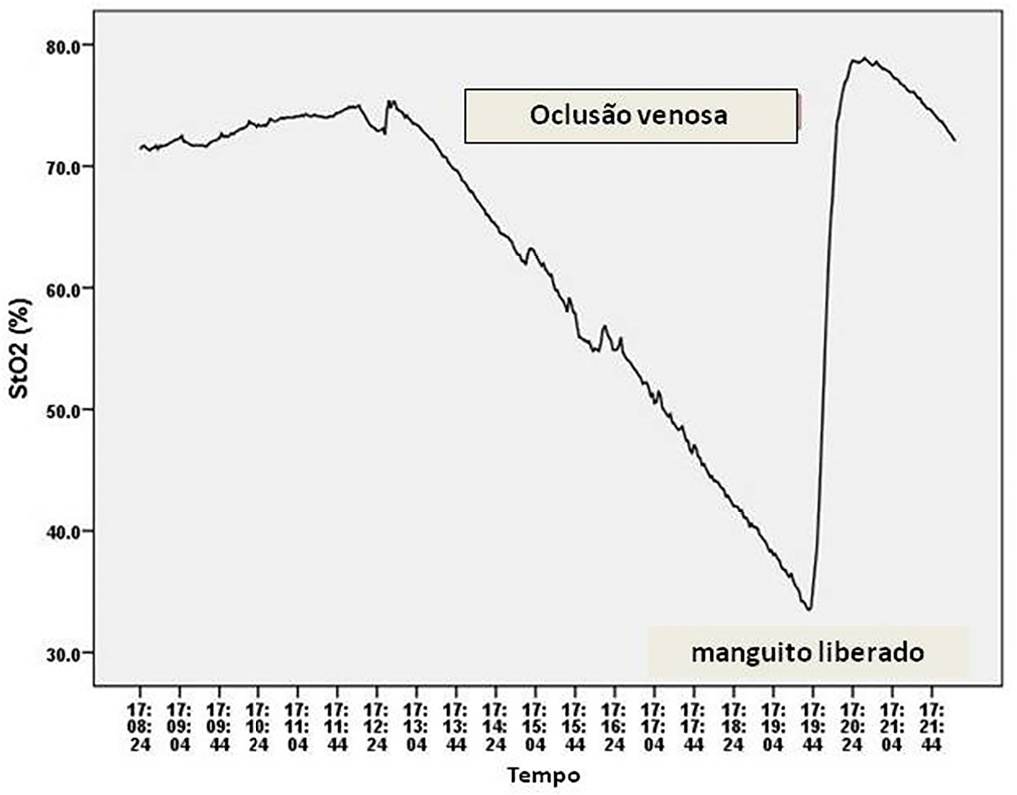
Observational study in intensive care unit patients. Tissue oxygen saturation was monitored (InSpectra Tissue Spectrometer Model 650, Hutchinson Technology Inc., MN, USA) with a multiprobe (15/25mm) in the thenar position. A venous occlusion test in volunteers was applied in the upper arm to test the tolerability and pattern of StO2 changes during the venous occlusion test. A sphygmomanometer cuff was inflated to a pressure 30mmHg above diastolic pressure until StO2 reached a plateau and deflated to 0mmHg. Tissue oxygen saturation parameters were divided into resting StO2 (r-StO2) and minimal StO2 (m-StO2) at the end of the venous occlusion test. In patients, the cuff was inflated to a pressure 30mmHg above diastolic pressure for 5 min (volunteers’ time derived) or until a StO2 plateau was reached. Tissue oxygen saturation parameters were divided into r-StO2, m-StO2, and the mean time that StO2 reached ScvO2. The StO2 value at the mean time was compared to ScvO2.
All 9 volunteers tolerated the venous occlusion test. The time for tolerability or the StO2 plateau was 7 ± 1 minutes. We studied 22 patients. The mean time for StO2 equalized ScvO2 was 100 sec and 95 sec (15/25mm probes). The StO2 value at 100 sec ([100-StO2] 15mm: 74 ± 7%; 25mm: 74 ± 6%) was then compared with ScvO2 (75 ± 6%). The StO2 value at 100 sec correlated with ScvO2 (15 mm: R2 = 0.63, 25mm: R2 = 0.67, p < 0.01) without discrepancy (Bland Altman).
Central venous oxygen saturation can be estimated from StO2 during a venous occlusion test.
Abstract
Rev Bras Ter Intensiva. 2022;34(1):185-196
DOI 10.5935/0103-507X.20220013-en
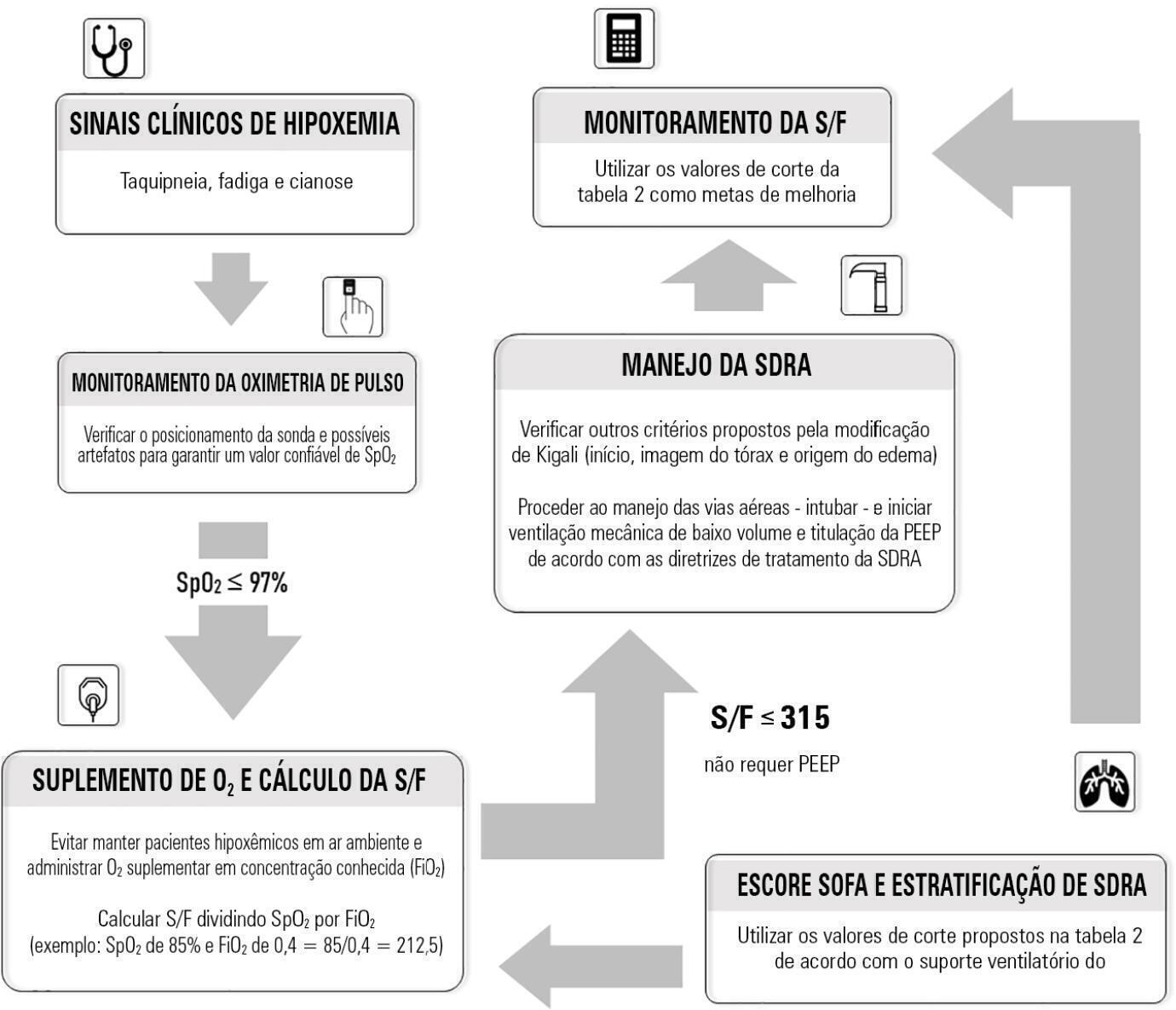
Although the PaO 2/FiO 2 derived from arterial blood gas analysis remains the gold standard for the diagnosis of acute respiratory failure, the SpO2/FiO2 has been investigated as a potential substitute. The current narrative review presents the state of the preclinical and clinical literature on the SpO2/FiO2 as a possible substitute for PaO2/FiO2 and for use as a diagnostic and prognostic marker; provides an overview of pulse oximetry and its limitations, and assesses the utility of SpO2/ FiO2 as a surrogate for PaO2/FiO2 in COVID-19 patients. Overall, 49 studies comparing SpO2/FiO2 and PaO2/FiO2 were found according to a minimal search strategy. Most were conducted on neonates, some were conducted on adults with acute respiratory distress syndrome, and a few were conducted in other clinical scenarios (including a very few on COVID-19 patients). There is some evidence that the SpO2/ FiO2 criteria can be a surrogate for PaO2/FiO2 in different clinical scenarios. This is reinforced by the fact that unnecessary invasive procedures should be avoided in patients with acute respiratory failure. It is undeniable that pulse oximeters are becoming increasingly widespread and can provide costless monitoring. Hence, replacing PaO2/FiO2 with SpO2/FiO2may allow resourcelimited facilities to objectively diagnose acute respiratory failure.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)