Abstract
Rev Bras Ter Intensiva. 2019;31(4):529-535
DOI 10.5935/0103-507X.20190066
To measure and compare the functionality of patients after discharge from the intensive care unit and at the time of hospital discharge.
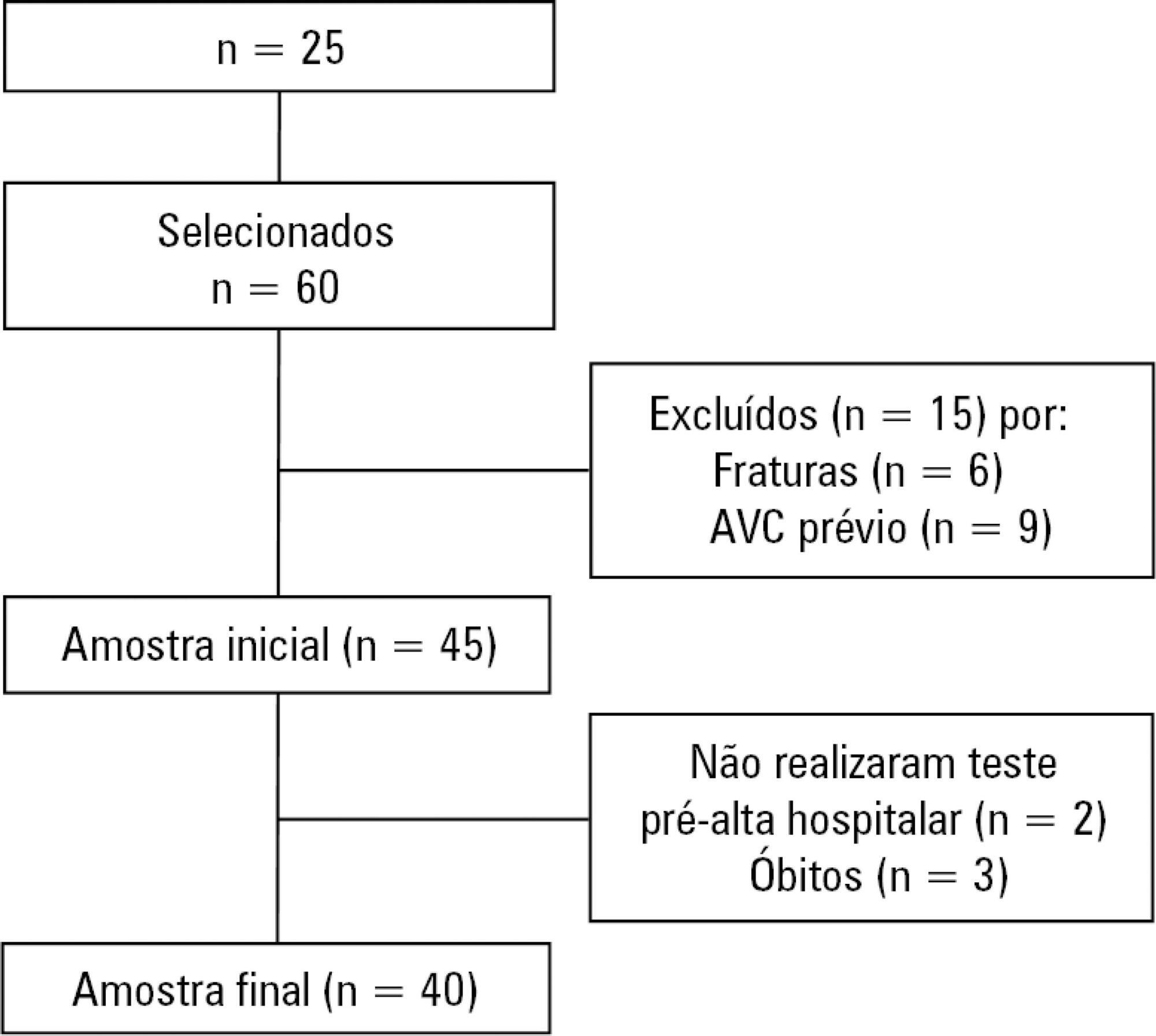
Quantitative study of a prospective cohort performed between August of 2016 and December of 2017 at a university hospital. A 10-meter walk test was performed at 2 timepoints: after discharge from the intensive care unit and prior to hospital discharge. The data were analyzed using Student's t-test and Pearson or Spearman correlation. Statistical Package for Social Science (SPSS) version 21.0 was used for the analysis, and p ≤ 0.05 was adopted as the level of significance.
Forty patients, with a mean age of 57.1 ± 12.2 years and with a predominance of males (60%), were evaluated. For the post-intensive care unit test, a mean speed of 0.48m/s was observed, and for the pre-hospital discharge test, there was an increase to 0.71m/s, evidencing functional evolution during the hospital stay (p < 0.001).
There was significant improvement in walking speed at the time of hospital discharge when compared to the walking speed at the time of intensive care unit discharge.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):335-340
DOI 10.5935/0103-507X.20160057
To evaluate the perceptions of physicians, nurses and nursing technicians of their participation in the decision-making process surrounding life support limitation in terminally ill pediatric patients, with comparisons by professional category.
A cross-sectional study was conducted in the pediatric intensive care unit of a tertiary public university hospital with the participation of physicians, nurses and nursing technicians. The MacArthur Admission Experience Survey Voice Scale was used to assess and quantify the perceptions of professionals who assisted 17 pediatric patients with life support limitation within 24 hours after the outcome of each patient was determined. All professionals working in the unit (n = 117) who were potentially eligible for the study received a free and informed consent form prior to the occurrence of the cases studied.
Study participants included 25/40 (62.5%) physicians, 10/17 (58.8%) nurses and 41/60 (68.3%) nursing technicians, representing 65% of the eligible professionals identified. The questionnaire return rate was higher for physicians than technicians (p = 0.0258). A perceived lack of voice was reported in all three professional categories at varying rates that were lower for physicians than for nurses and nursing technicians (p < 0.00001); there was no difference between the latter (p = 0.7016). In the three professional categories studied, three subscale items were reported. For two of the three statements, there were significant differences between physicians and nurses (p = 0.004) and between physicians and nursing technicians (p = 0.001). For one of the statements, there was no difference among the three professional categories.
Respondents perceived a lack of voice in the decision-making process at varying rates across the three categories of studied professionals who assisted terminally ill pediatric patients with life support limitation, with physicians expressing lowered rates of perceived coercion.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):274-283
DOI 10.5935/0103-507X.20150032
To systematically review the main methods for nutritional risk assessment used in critically ill cancer patients and present the methods that better assess risks and predict relevant clinical outcomes in this group of patients, as well as to discuss the pros and cons of these methods according to the current literature.
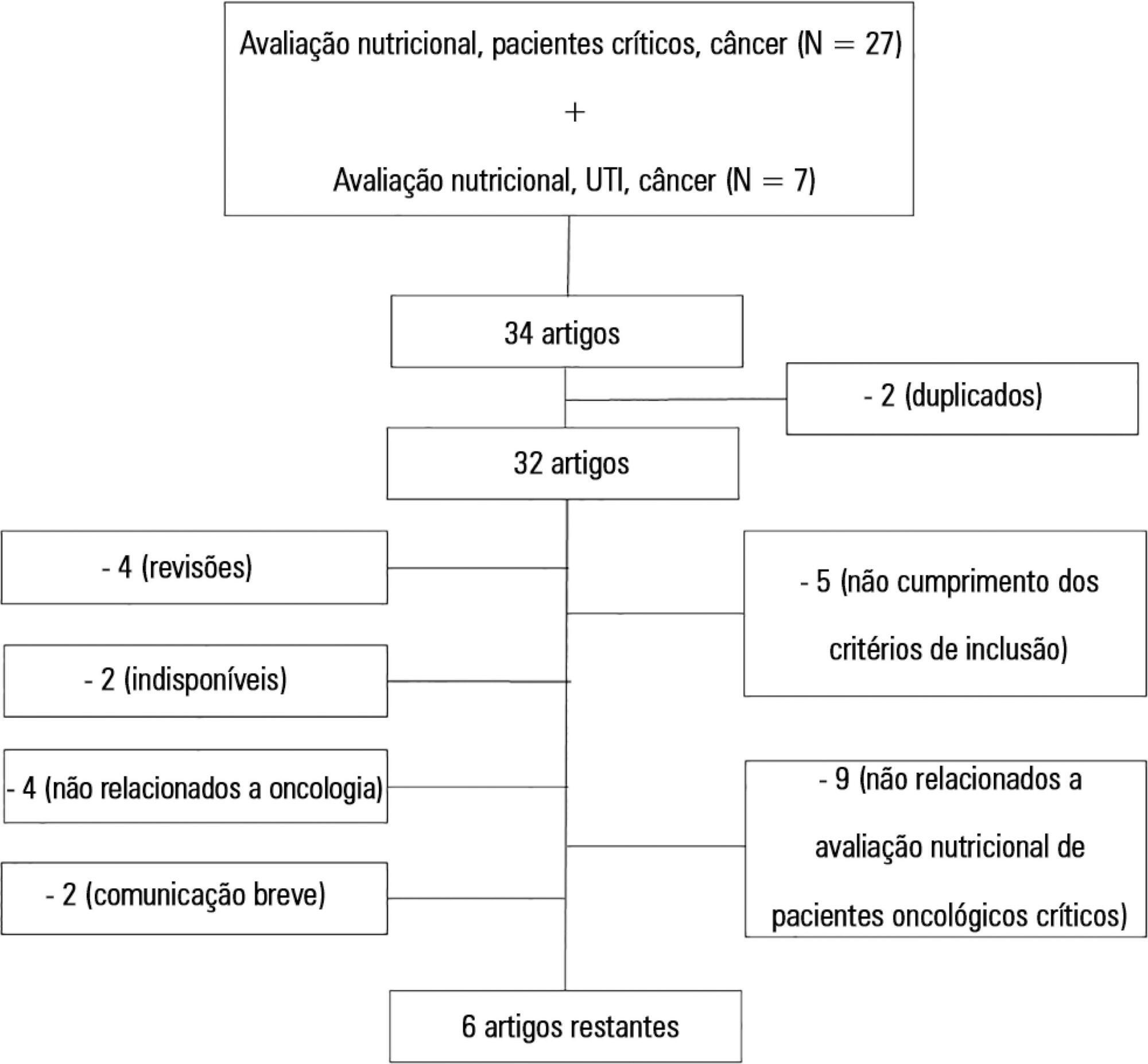
The study consisted of a systematic review based on analysis of manuscripts retrieved from the PubMed, LILACS and SciELO databases by searching for the key words “nutritional risk assessment”, “critically ill” and “cancer”.
Only 6 (17.7%) of 34 initially retrieved papers met the inclusion criteria and were selected for the review. The main outcomes of these studies were that resting energy expenditure was associated with undernourishment and overfeeding. The high Patient-Generated Subjective Global Assessment score was significantly associated with low food intake, weight loss and malnutrition. In terms of biochemical markers, higher levels of creatinine, albumin and urea were significantly associated with lower mortality. The worst survival was found for patients with worse Eastern Cooperative Oncologic Group - performance status, high Glasgow Prognostic Score, low albumin, high Patient-Generated Subjective Global Assessment score and high alkaline phosphatase levels. Geriatric Nutritional Risk Index values < 87 were significantly associated with mortality. A high Prognostic Inflammatory and Nutritional Index score was associated with abnormal nutritional status in critically ill cancer patients. Among the reviewed studies that examined weight and body mass index alone, no significant clinical outcome was found.
None of the methods reviewed helped to define risk among these patients. Therefore, assessment by a combination of weight loss and serum measurements, preferably in combination with other methods using scores such as Eastern Cooperative Oncologic Group - performance status, Glasgow Prognostic Score and Patient-Generated Subjective Global Assessment, is suggested given that their use is simple, feasible and useful in such cases.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):115-122
DOI 10.5935/0103-507X.20130022
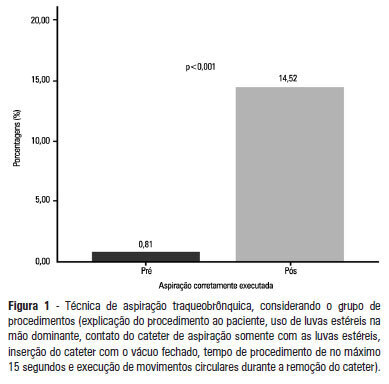
OBJECTIVE: To evaluate the effectiveness of an educational intervention on healthcare professionals' adherence to the technical recommendations for tracheobronchial aspiration in intensive care unit patients. METHODS: A quasi-experimental study was performed to evaluate intensive care unit professionals' adherence to the tracheobronchial aspiration technical recommendations in intensive care unit patients both before and after a theoretical and practical educational intervention. Comparisons were performed using the chi-square test, and the significance level was set to p<0.05. RESULTS: A total of 124 procedures, pre- and post-intervention, were observed. Increased adherence was observed in the following actions: the use of personal protective equipment (p=0.01); precaution when opening the catheter package (p<0.001); the use of a sterile glove on the dominant hand to remove the catheter (p=0.003); the contact of the sterile glove with the catheter only (p<0.001); the execution of circular movements during the catheter removal (p<0.001); wrapping the catheter in the sterile glove at the end of the procedure (p=0.003); the use of distilled water, opened at the start of the procedure, to wash the connection latex (p=0.002); the disposal of the leftover distilled water at the end of the procedure (p<0.001); and the performance of the aspiration technique procedures (p<0.001). CONCLUSION: There was a low adherence by health professionals to the preventive measures against hospital infection, indicating the need to implement educational strategies. The educational intervention used was shown to be effective in increasing adherence to the technical recommendations for tracheobronchial aspiration.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):44-48
DOI 10.1590/S0103-507X2013000100009
OBJECTIVE: To evaluate the effectiveness of a tongue cleaner in the removal of tongue biofilm in mechanically ventilated patients. METHODS: Tongue biofilm and tracheal secretion samples were collected from a total of 50 patients: 27 in the study group (SG) who were intubated or tracheostomized under assisted ventilation and treated with the tongue cleaner and 23 in the control group (CG) who did not undergo tongue cleaning. Oral and tracheal secretion cultures of the SG (initially and after 5 days) and the CG (at a single time-point) were performed to evaluate the changes in bacterial flora. RESULTS: The median age of the SG patients was 77 years (45-99 years), and that of the CG patients was 79 years (21-94 years). The length of hospital stay ranged from 17-1,370 days for the SG with a median stay of 425 days and from 4-240 days for the CG with a median stay of 120 days. No significant differences were found when the dental plaque indexes were compared between the SG and the CG. There was no correlation between the index and the length of hospital stay. The same bacterial flora was found in the dental plaque of 9 of the 27 SG patients before and after the tongue scraper was used for 5 days compared with the CG (p=0.683). Overall, 7 of the 27 SG patients had positive bacterial cultures for the same strains in both tongue biofilm and tracheal secretions compared with the CG (p=0.003). Significant similarities in strain resistance and susceptibility of the assessed microorganisms were observed between oral and tracheal microflora in 6/23 cases in the CG (p=0.006). CONCLUSION: The use of a tongue cleaner is effective at reducing tongue biofilm in patients on mechanical ventilation and facilitates oral hygiene interventions performed by caregivers.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):276-282
DOI 10.1590/S0103-507X2009000300007
OBJECTIVE: The understanding of adverse events may simplify the inquiry regarding the quality of nursing care, presuming a foregrounding role in evaluating health services. The aim of the study was to identify adverse events in nursing care in an intensive care unit. METHODS: Data were collected using an appropriate form known as problem-oriented record (POR) over a 10-month period; patients were monitored throughout their intensive care unit stay. RESULTS: Over the study period, 550 adverse events were recorded as follows: 26 concerned the "five rights" related to drug administration; 23 to non-administered medication; 181 to inappropriate medication records; 28 to failure in infusion pump assembly; 17 to not performed inhalation; 8 to incorrect handling of needles and syringes; 53 to not performed nursing procedures; 46 to incorrect handling of therapeutic and diagnostic devices; 37 to alarms/warnings of devices used incorrectly; and 131 to failure in data recording by nurses. CONCLUSION: The occurrence of adverse events in the care given to patients by the nursing team are significant indicators that disclose the quality of nursing care. Therefore, these events should be analyzed to support in-service training of the nursing staff.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):283-291
DOI 10.1590/S0103-507X2009000300008
OBJECTIVES: The intensive care unit emerged to improve and concentrate material and human resources for the care of critical patients, and need for constant observation and continuous assistance. However, patients in intensive care unit requires exceptional care, directed not only to the physiopathological problem, but also towards the psychosocial issue, now intimately interlinked to the physical disease. In this ambient, very demanding for capability of the multiprofessional team, presence of the physiotherapist has become more frequent. This study aims to verify if the attitude of an experienced physiotherapist in the intensive care unit is humanized. METHODS: To evaluate physiotherapy care humanization, a questionnaire was prepared and patients over 18 years of age, lucid and staying in intensive care unit for 24 hours or more were included. RESULTS: Forty four patients were interviewed and 95.5% of these considered the physiotherapy care as humanized. Positive association was observed between dissatisfaction with the items of dignity, communication, warranty and empathy, and a dehumannized physiotherapy care. Patients who evaluated warranty as negative had a twofold greater chance (0.7 - 5.3) of perceiving care as dehumanized. Patients who evaluated empathy as negative had a 1.6 (0.8 - 3.4) times greater chance of perceiving care as dehumanized. CONCLUSION: Physiotherapy care given in the intensive care unit was marked by good assistance, attention provided to the patient and quality of treatment, characterizing humanized care.
Abstract
Rev Bras Ter Intensiva. 2008;20(3):286-295
DOI 10.1590/S0103-507X2008000300012
Considering the importance and the difficulties inherent to nutritional state assessment, as well as the results interpretation and the inexistence of specific and validated guidelines related to applied methods to the severely ill patient, the present revision aims to contribute to the analysis and recommendation of efficient methods, which are suitable to use and reliable in terms of interpretation in the context of the severely ill patient. The presence of edema and unspecific alterations in the plasmatic concentrations of proteins; altered anthropometrics variables reflecting more the rearrangement of the total body water than the nutritional state changes; inconclusive studies with electric bioimpedance; absence of data related to the application of the global subjective assessment to severely ill patients; altered biochemical markers as a consequence of the metabolic changes that, among others, indicate several method limitations to these patients. Notwithstanding the lack of studies to validate the various methods, recommendations based on clinical evidences, observation and physiopathology alterations are available. Independent from the methods, clinical observation by the health staff at all stages is mandatory. It is crucial to dedicate more efforts to identify methods and their specificity to detection, risk assessment or monitoring.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)