Abstract
Rev Bras Ter Intensiva. 2019;31(2):113-121
DOI 10.5935/0103-507X.20190018
To describe (1) the energy transfer from the ventilator to the lungs, (2) the match between venous-venous extracorporeal membrane oxygenation (ECMO) oxygen transfer and patient oxygen consumption (VO2), (3) carbon dioxide removal with ECMO, and (4) the potential effect of systemic venous oxygenation on pulmonary artery pressure.
Mathematical modeling approach with hypothetical scenarios using computer simulation.
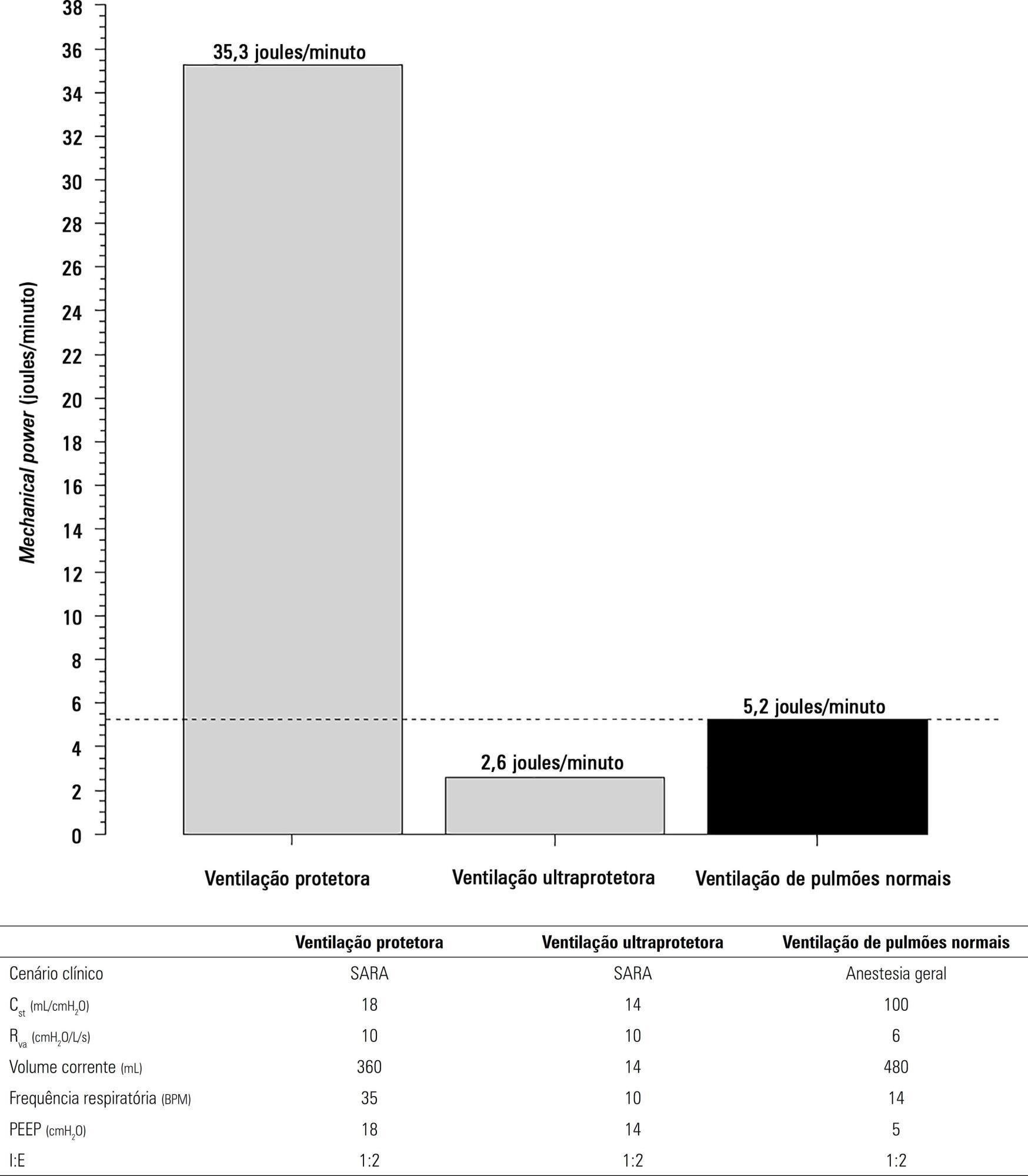
The transition from protective ventilation to ultraprotective ventilation in a patient with severe acute respiratory distress syndrome and a static respiratory compliance of 20mL/cm H2O reduced the energy transfer from the ventilator to the lungs from 35.3 to 2.6 joules/minute. A hypothetical patient, hyperdynamic and slightly anemic with VO2 = 200mL/minute, can reach an arterial oxygen saturation of 80%, while maintaining the match between the oxygen transfer by ECMO and the VO2 of the patient. Carbon dioxide is easily removed, and normal PaCO2 is easily reached. Venous blood oxygenation through the ECMO circuit may drive the PO2 stimulus of pulmonary hypoxic vasoconstriction to normal values.
Ultraprotective ventilation largely reduces the energy transfer from the ventilator to the lungs. Severe hypoxemia on venous-venous-ECMO support may occur despite the matching between the oxygen transfer by ECMO and the VO2 of the patient. The normal range of PaCO2 is easy to reach. Venous-venous-ECMO support potentially relieves hypoxic pulmonary vasoconstriction.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):508-511
DOI 10.5935/0103-507X.20180072
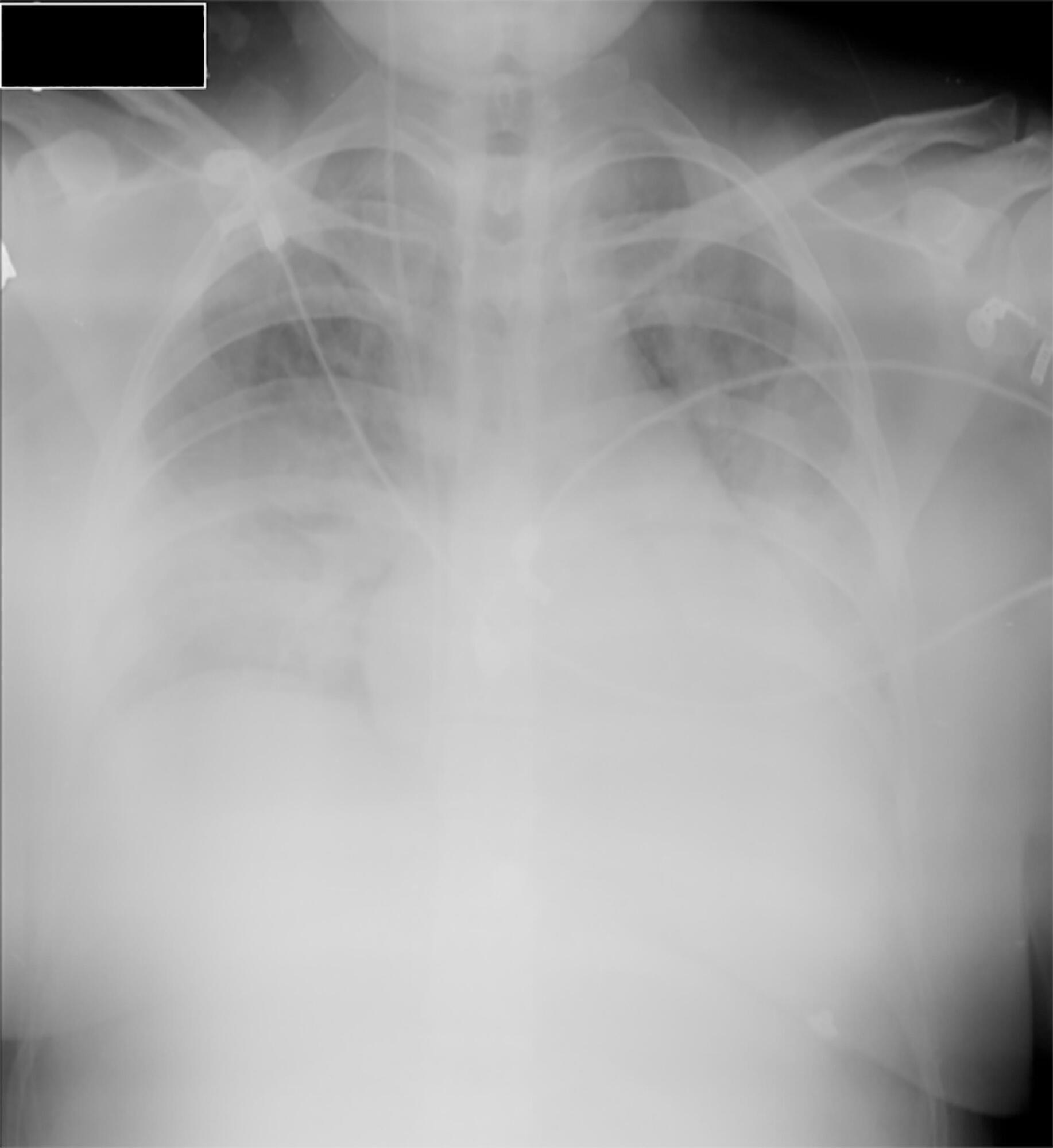
Little evidence exists to support the use of noninvasive mechanical ventilation for acute hypoxemic respiratory failure. However, considering the complications associated with endotracheal intubation, we attempted to implement noninvasive mechanical ventilation in a 24-year-old patient who was 32 weeks pregnant and was admitted to the intensive care unit with acute hypoxemic respiratory failure and sepsis secondary to a urinary tract infection. Lack of tolerance to noninvasive mechanical ventilation led us to use an alternative method to avoid endotracheal intubation. The use of high-flow nasal cannula allowed to overcome this situation, wich supports this technique as a treatment option for critical obstetric patients that is safe for both the mother and fetus.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):12-16
DOI 10.1590/S0103-507X2013000100004
OBJECTIVE: This study aimed to evaluate the outcomes for patients with lung cancer admitted to intensive care units and assess their clinical and demographic profiles. METHODS: Retrospective, analytical, observational study, wherein the outcomes for patients diagnosed with lung cancer admitted to the intensive care unit of university hospital from January 2010 until February 2011 were evaluated. RESULTS: Thirty-four patients' medical records were included. Twenty-six (76.5%) patients received some type of ventilatory support, of whom 21 (61.8%) used invasive mechanical ventilation and 11 (32.4%) used noninvasive ventilation at some point during their stay at the intensive care unit. Regarding mortality, 12 (35.3%) patients died during hospitalization at the intensive care unit, totaling 15 (44.1%) deaths during the entire hospitalization period; 19 (55.9%) patients were discharged from the hospital. The analysis of the variables showed that the patients who died had remained on invasive mechanical ventilation for a longer period 5.0 (0.25 to 15.0) days than the survivors (1.0 (0 to 1.0) days) (p=0.033) and underwent dialysis during their stay at the intensive care unit (p=0.014). CONCLUSIONS: The mortality of patients with lung cancer admitted to the intensive care unit is associated with the time spent on invasive mechanical ventilation and the need for dialysis.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):321-326
DOI 10.1590/S0103-507X2011000300010
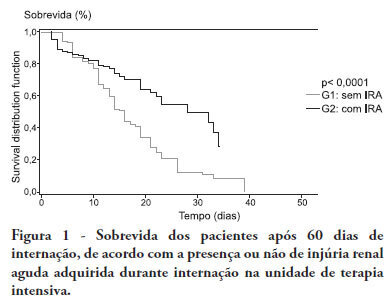
OBJECTIVE:To compare the clinical features and outcomes of patients with and without acute kidney injury in an intensive care unit of a tertiary university hospital and to identify acute kidney injury and mortality risk factors. METHODS: This was a prospective observational study of a cohort including 564 patients followed during their stay in the intensive care unit of Hospital das Clinicas da Faculdade de Medicina de Botucatu (Botucatu, São Paulo, Brazil) between May 2008 and May 2010. Patients were allocated to two different groups: with (G1) and without (G2) acute kidney injury. RESULTS: The incidence of acute kidney injury was 25.5%. The groups were different with respect to the reason for admission to the intensive care unit (sepsis, G1: 41.6% versus G2: 24.1%; P < 0.0001; neurosurgery, postoperative G1: 13.8% versus G2: 38.1%; P < 0.0001); age (G1: 56.8 ± 15.9 vs. G2: 49.8 ± 17.8 years; P < 0.0001); Acute Physiological Chronic Health Evaluation (APACHE) II score (G1: 21.9 ± 6.9 versus G2: 14.1 ± 4.6; P < 0.0001); use of mechanical ventilation (G1: 89.2% vs. G2: 69.1%; P < 0.0001) and use of vasoactive drugs (G1: 78.3% vs. G2: 56.1%; P < 0.0001). Higher rates of diabetes mellitus, congestive heart failure, chronic renal disease and use of non-steroidal anti-inflammatory drugs were more frequent in acute kidney injury patients (28.2% vs. 19.7%, P = 0.03; 23.6 vs. 11.6%, P = 0.0002; 21.5% vs. 11.5%, P < 0.0001 and 23.5% vs. 71.%, P < 0.0001, for G1 versus G2, respectively). Length of hospital stay and mortality were also higher for acute kidney injury patients (G1: 6.6 ± 2.7 days versus G2: 12.9 ±5.6 days, P < 0.0001 and G1: 62.5% versus G2: 16.4%, P < 0.0001). Multivariate analysis identified the following as risk factors for acute kidney injury: age above 55 years, APACHE II score above 16, baseline creatinine above 1.2 and use of non-steroidal anti-inflammatory drugs (odds ratio (OR) = 1.36, 95% confidence interval (95%CI): 1.22 - 1.85; OR = 1.2, 95%CI: 1.11 - 1.33; OR = 5.2, 95%CI: 2.3 - 11.6 and OR = 2.15, 95%CI: 1.1 - 4.2, respectively). Acute kidney injury was independently associated with longer hospital stay and increased mortality (OR = 1.18, 95%CI: 1.05 - 1.26 and OR = 1.24, 95%CI: 1.09 - 1.99, respectively). Analysis of the survival curve 30 days after admission showed 83.3% mortality for acute kidney injury patients and 45.2% for non-acute kidney injury patients (P < 0.0001). CONCLUSION: The incidence of acute kidney injury was high in this intensive care unit; the independent risk factors associated with acute kidney injury were age > 55 years, APACHE II > 16, baseline serum creatinine > 1.2 and use of non-steroidal anti-inflammatory drugs. Acute kidney injury is an independent risk factor for longer intensive care unit stay and mortality.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):250-256
DOI 10.1590/S0103-507X2010000300006
OBJECTIVE: The intensive care unit is synonymous of high severity, and its mortality rates are between 5.4 and 33%. With the development of new technologies, a patient can be maintained for long time in the unit, causing high costs, psychological and moral for all involved. This study aimed to evaluate the risk factors for mortality and prolonged length of stay in an adult intensive care unit. METHODS: The study included all patients consecutively admitted to the adult medical/surgical intensive care unit of Hospital das Clínicas da Universidade Estadual de Campinas, for six months. We collected data such as sex, age, diagnosis, personal history, APACHE II score, days of invasive mechanical ventilation orotracheal reintubation, tracheostomy, days of hospitalization in the intensive care unit and discharge or death in the intensive care unit. RESULTS: Were included in the study 401 patients; 59.6% men and 40.4% women, age 53.8±18.0. The mean intensive care unit stay was 8.2±10.8 days, with a mortality rate of 13.5%. Significant data for mortality and prolonged length of stay in intensive care unit (p <0.0001), were: APACHE II>11, OT-Re and tracheostomy. CONCLUSION: The mortality and prolonged length of stay in intensive care unit intensive care unit as risk factors were: APACHE>11, orotracheal reintubation and tracheostomy.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):5-10
DOI 10.1590/S0103-507X2010000100003
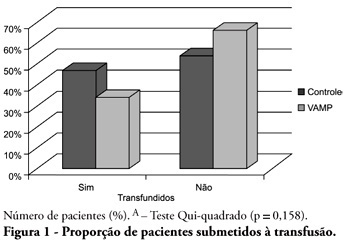
OBJECTIVE: Anemia is common in severely ill patients, and blood sampling plays a relevant causative role. Consequently, blood transfusions are frequent an related to several complications. Trying to reduce the transfusion-related risk, minimizing blood loss is mandatory. Thus, this work aimed to evaluate a closed blood sampling system as a strategy to spare unnecessary blood losses and transfusions. METHODS: This was a prospective, randomized, controlled, multicenter, 6 months, clinical trial. The patients were assigned to either VAMP (Venous Arterial Blood Management Protection) group, using a closed blood sampling system, or control group. The groups' transfusion rate, as well as hemoglobin (Hb) and Hematocrit (Ht) changes were compared for 14 days. RESULTS: Were included 127 patients, 65 assigned to the control group, and 62 to VAMP. During the intensive care unit stay, both groups experienced both hemoglobin and hematocrit drops. However, when the final Ht and Hb were compared between the groups, a difference was identified with higher values in the VAMP group (p=0.03; p=0.006, respectively). No statistical difference was found for both groups transfusion rates, although the VAMP group had an absolute 12% blood transfusion reduction. CONCLUSION: The use of a closed blood sampling system was able to minimize blood count values changes, however failed to reduce transfusions rate.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):432-436
DOI 10.1590/S0103-507X2009000400014
The world is aging. In Brazil, and in several other countries in the world, changes in population's age composition have been accompanied by an increase in demand for types of health care whose cost is high. Actually, some moral conflicts are arising from allocation of public resources for health, because the magnitude of social inequalities in health and limited resources require that priorities for public management are based on knowledge of the health situation and the impact of policies, programs, projects and actions on health. In this context, the intensive medicine, managers and physicians in intensive care are subject to moral conflicts, especially at the fair micro allocation resources for the elderly in the intensive care unit level. This paper attempts to review the situation of conflicts in the light of the tools of bioethics.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):283-291
DOI 10.1590/S0103-507X2009000300008
OBJECTIVES: The intensive care unit emerged to improve and concentrate material and human resources for the care of critical patients, and need for constant observation and continuous assistance. However, patients in intensive care unit requires exceptional care, directed not only to the physiopathological problem, but also towards the psychosocial issue, now intimately interlinked to the physical disease. In this ambient, very demanding for capability of the multiprofessional team, presence of the physiotherapist has become more frequent. This study aims to verify if the attitude of an experienced physiotherapist in the intensive care unit is humanized. METHODS: To evaluate physiotherapy care humanization, a questionnaire was prepared and patients over 18 years of age, lucid and staying in intensive care unit for 24 hours or more were included. RESULTS: Forty four patients were interviewed and 95.5% of these considered the physiotherapy care as humanized. Positive association was observed between dissatisfaction with the items of dignity, communication, warranty and empathy, and a dehumannized physiotherapy care. Patients who evaluated warranty as negative had a twofold greater chance (0.7 - 5.3) of perceiving care as dehumanized. Patients who evaluated empathy as negative had a 1.6 (0.8 - 3.4) times greater chance of perceiving care as dehumanized. CONCLUSION: Physiotherapy care given in the intensive care unit was marked by good assistance, attention provided to the patient and quality of treatment, characterizing humanized care.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)