You searched for:"Nara Yamane dos Santos"
We found (1) results for your search.-
Original Articles – Clinical Research
Acute kidney injury in intensive care unit patients: a prospective study on incidence, risk factors and
Rev Bras Ter Intensiva. 2011;23(3):321-326
Abstract
Original Articles – Clinical ResearchAcute kidney injury in intensive care unit patients: a prospective study on incidence, risk factors and
Rev Bras Ter Intensiva. 2011;23(3):321-326
DOI 10.1590/S0103-507X2011000300010
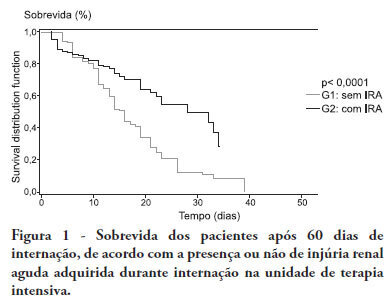
Views0See moreOBJECTIVE:To compare the clinical features and outcomes of patients with and without acute kidney injury in an intensive care unit of a tertiary university hospital and to identify acute kidney injury and mortality risk factors. METHODS: This was a prospective observational study of a cohort including 564 patients followed during their stay in the intensive care unit of Hospital das Clinicas da Faculdade de Medicina de Botucatu (Botucatu, São Paulo, Brazil) between May 2008 and May 2010. Patients were allocated to two different groups: with (G1) and without (G2) acute kidney injury. RESULTS: The incidence of acute kidney injury was 25.5%. The groups were different with respect to the reason for admission to the intensive care unit (sepsis, G1: 41.6% versus G2: 24.1%; P < 0.0001; neurosurgery, postoperative G1: 13.8% versus G2: 38.1%; P < 0.0001); age (G1: 56.8 ± 15.9 vs. G2: 49.8 ± 17.8 years; P < 0.0001); Acute Physiological Chronic Health Evaluation (APACHE) II score (G1: 21.9 ± 6.9 versus G2: 14.1 ± 4.6; P < 0.0001); use of mechanical ventilation (G1: 89.2% vs. G2: 69.1%; P < 0.0001) and use of vasoactive drugs (G1: 78.3% vs. G2: 56.1%; P < 0.0001). Higher rates of diabetes mellitus, congestive heart failure, chronic renal disease and use of non-steroidal anti-inflammatory drugs were more frequent in acute kidney injury patients (28.2% vs. 19.7%, P = 0.03; 23.6 vs. 11.6%, P = 0.0002; 21.5% vs. 11.5%, P < 0.0001 and 23.5% vs. 71.%, P < 0.0001, for G1 versus G2, respectively). Length of hospital stay and mortality were also higher for acute kidney injury patients (G1: 6.6 ± 2.7 days versus G2: 12.9 ±5.6 days, P < 0.0001 and G1: 62.5% versus G2: 16.4%, P < 0.0001). Multivariate analysis identified the following as risk factors for acute kidney injury: age above 55 years, APACHE II score above 16, baseline creatinine above 1.2 and use of non-steroidal anti-inflammatory drugs (odds ratio (OR) = 1.36, 95% confidence interval (95%CI): 1.22 - 1.85; OR = 1.2, 95%CI: 1.11 - 1.33; OR = 5.2, 95%CI: 2.3 - 11.6 and OR = 2.15, 95%CI: 1.1 - 4.2, respectively). Acute kidney injury was independently associated with longer hospital stay and increased mortality (OR = 1.18, 95%CI: 1.05 - 1.26 and OR = 1.24, 95%CI: 1.09 - 1.99, respectively). Analysis of the survival curve 30 days after admission showed 83.3% mortality for acute kidney injury patients and 45.2% for non-acute kidney injury patients (P < 0.0001). CONCLUSION: The incidence of acute kidney injury was high in this intensive care unit; the independent risk factors associated with acute kidney injury were age > 55 years, APACHE II > 16, baseline serum creatinine > 1.2 and use of non-steroidal anti-inflammatory drugs. Acute kidney injury is an independent risk factor for longer intensive care unit stay and mortality.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




