Abstract
Rev Bras Ter Intensiva. 2021;33(3):362-373
DOI 10.5935/0103-507X.20210059
To determine the effectiveness of noninvasive ventilation versus conventional oxygen therapy in patients with acute respiratory failure after extubation failure.
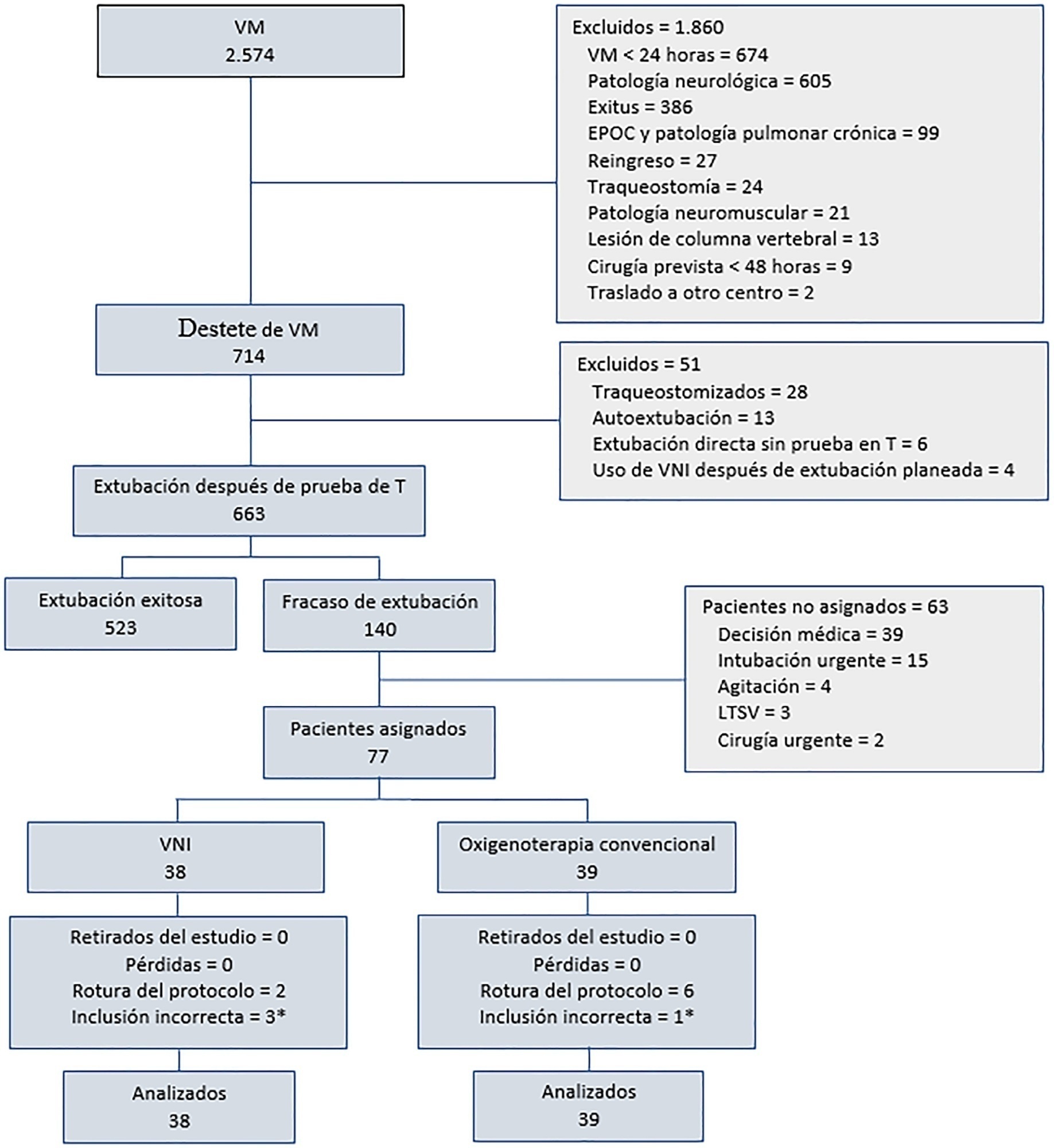
A pragmatic clinical trial was conducted in an intensive care unit from March 2009 to September 2016. Patients on mechanical ventilation > 24 hours who developed acute respiratory failure after scheduled extubation were included and were assigned to noninvasive ventilation or conventional oxygen therapy. The primary objective was to reduce the reintubation rate. The secondary objectives were to improve respiratory parameters and reduce complications, the duration of mechanical ventilation, the intensive care unit stay, the hospital stay, and mortality in the intensive care unit, in the hospital, and 90 days after discharge. Factors correlated with reintubation were also analyzed.
Of a total of 2,574 patients, 77 were analyzed (38 in the noninvasive ventilation group and 39 in the conventional oxygen therapy group). Noninvasive ventilation reduced the respiratory and cardiac rates more rapidly than conventional oxygen therapy. Reintubation was less common in the noninvasive ventilation group [12 (32%) versus 22 (56%) in the conventional oxygen therapy group, relative risk 0.58 (95%CI 0.34 - 0.97), p = 0.039]. The rest of the parameters did not show significant differences. In the multivariate analysis, noninvasive ventilation protected against reintubation [OR 0.17 (95%CI 0.05 - 0.56), p = 0.004], while liver failure before extubation and the inability to maintain airway patency predisposed patients to reintubation.
The use of noninvasive ventilation in patients who failed extubation could be beneficial compared to conventional oxygen therapy.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):384-393
DOI 10.5935/0103-507X.20210055
To describe current clinical practices related to the use of high-flow nasal cannula therapy by Brazilian pediatric intensivists and compare them with those in other countries.
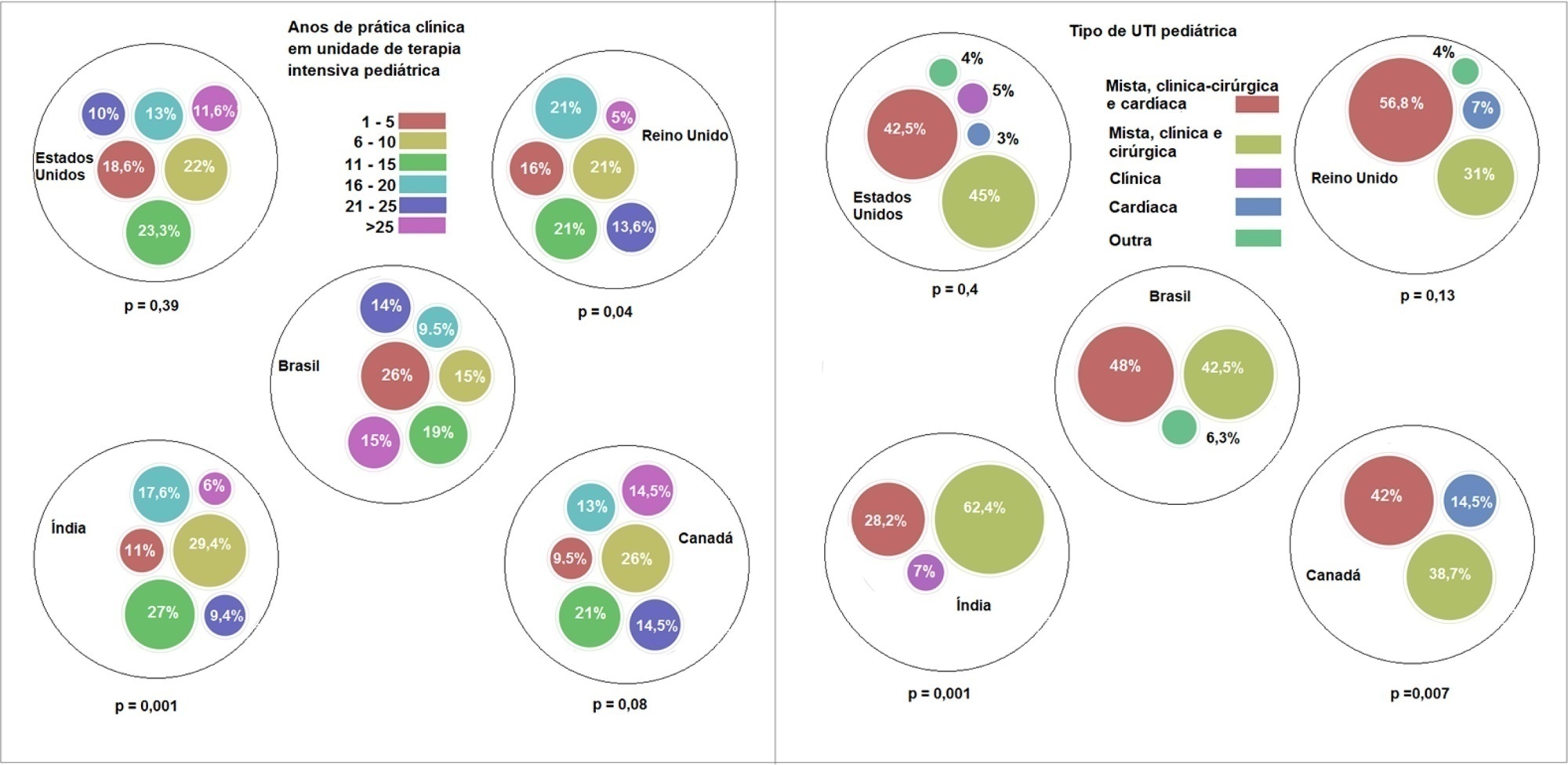
A questionnaire was administered to pediatric intensivists in North and South America, Asia, Europe, and Australia/New Zealand for the main study. We compared the Brazilian cohort with cohorts in the United States of America, Canada, the United Kingdom, and India
Overall, 501 physicians responded, 127 of which were in Brazil. Only 63.8% of respondents in Brazil had a high-flow nasal cannula available, in contrast to 100% of respondents in the United Kingdom, Canada, and the United States. The attending physician was responsible for the decision to start a high-flow nasal cannula according to 61.2% respondents in Brazil, 95.5% in the United Kingdom, 96.6% in the United States, 96.8% in Canada, and 84.7% in India. A total of 62% of respondents in Brazil, 96.3% in the United Kingdom, 96.6% in the United States, 96.8% in Canada, and 84.7% in India reported that the attending physician was responsible for the decision to wean or modify the high-flow nasal cannula settings. When high-flow nasal cannula therapy failed due to respiratory distress/failure, 82% of respondents in Brazil would consider a trial of noninvasive ventilation before endotracheal intubation, compared to 93% in the United Kingdom, 88% in the United States, 91.5% in Canada, and 76.8% in India. More Brazilian intensivists (6.5%) than intensivists in the United Kingdom, United States, and India (1.6% for all) affirmed using sedatives frequently with high-flow nasal cannulas.
The availability of high-flow nasal cannulas in Brazil is still not widespread. There are some divergences in clinical practices between Brazilian intensivists and their colleagues abroad, mainly in processes and decision-making about starting and weaning high-flow nasal cannula therapy.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):487-495
DOI 10.5935/0103-507X.20180070
To evaluate the efficacy of high-flow nasal cannula in the prevention of intubation and re-intubation in critically ill patients compared to conventional oxygen therapy or noninvasive ventilation.
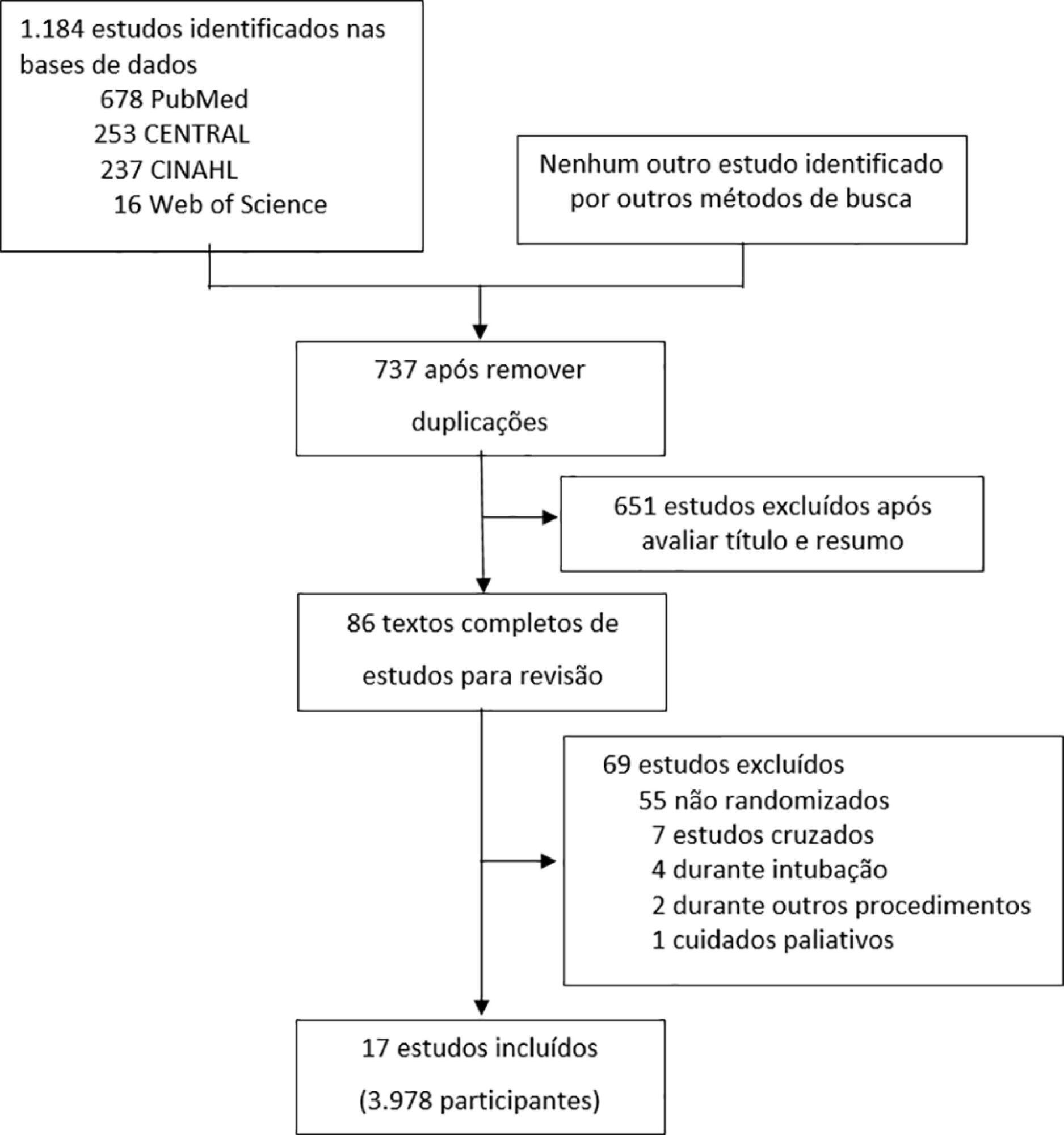
This systematic review was performed through an electronic database search of articles published from 1966 to April 2018. The primary outcome was the need for intubation or re-intubation. The secondary outcomes were therapy escalation, mortality at the longest follow-up, hospital mortality and the need for noninvasive ventilation.
Seventeen studies involving 3,978 patients were included. There was no reduction in the need for intubation or re-intubation with high-flow nasal cannula (OR 0.72; 95%CI 0.52 - 1.01; p = 0.056). There was no difference in the need for therapy escalation (OR 0.80, 95% CI 0.59 - 1.08, p = 0.144), mortality at the longest follow-up (OR 0.94; 95%CI 0.70 - 1.25; p = 0.667), hospital mortality (OR 0.84; 95%CI 0.56 - 1.26; p = 0.391) or noninvasive ventilation (OR 0.64, 95%CI 0.39 - 1.05, p = 0.075). In the trial sequential analysis, the number of events included was lower than the optimal information size with a global type I error > 0.05.
In the present study and setting, high-flow nasal cannula was not associated with a reduction of the need for intubation or re-intubation in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):508-511
DOI 10.5935/0103-507X.20180072
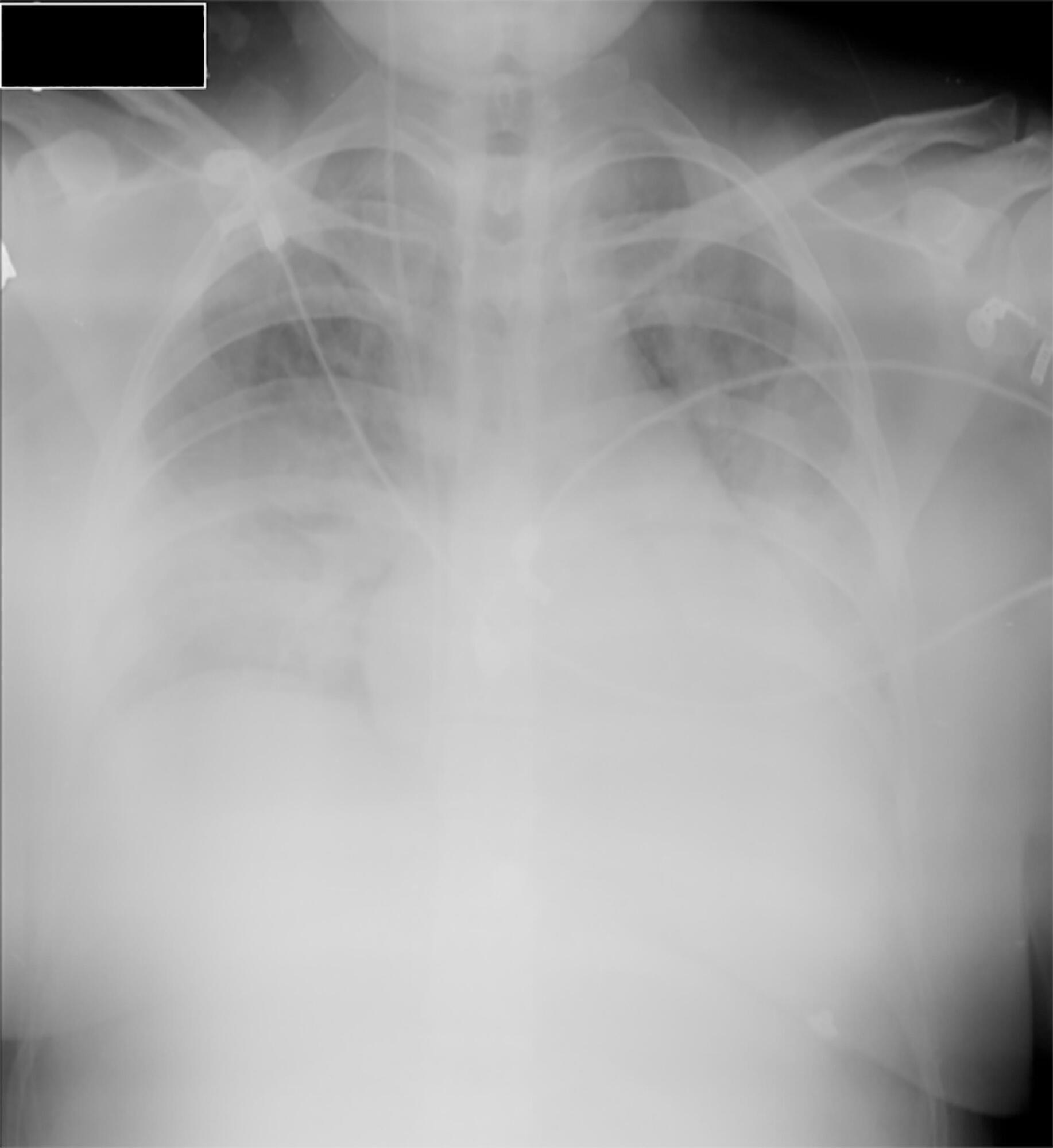
Little evidence exists to support the use of noninvasive mechanical ventilation for acute hypoxemic respiratory failure. However, considering the complications associated with endotracheal intubation, we attempted to implement noninvasive mechanical ventilation in a 24-year-old patient who was 32 weeks pregnant and was admitted to the intensive care unit with acute hypoxemic respiratory failure and sepsis secondary to a urinary tract infection. Lack of tolerance to noninvasive mechanical ventilation led us to use an alternative method to avoid endotracheal intubation. The use of high-flow nasal cannula allowed to overcome this situation, wich supports this technique as a treatment option for critical obstetric patients that is safe for both the mother and fetus.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):292-298
DOI 10.1590/S0103-507X2009000300009
BACKGROUND AND OBJECTIVES: An inspired oxygen fraction (FiO2) of 40% is often used for weaning patients, but lower FiO2 values are also recommended, if arterial oxygen pressure (PaO2)/ FiO2 >150-200 mmHg. This study aimed to compare respiratory variables and vital data values recorded during use of sufficient FiO2 (ideal) to maintain peripheral oxygen saturation at 92% with values recorded during use of FiO2 established at 40% (baseline) in weaning patients. METHODS: Prospective cross-over study. Respiratory variables (respiratory frequency, tidal volume, occlusion pressure, inspiratory time/total time ratio) and vital data (blood pressure and heart rate) were collected sequentially at 30 and 60 minutes with baseline FiO2, followed by ideal FiO2. These were compared to a generalized linear model for repeated measurements. Comparisons between baseline and ideal FiO2 values, and arterial blood gases were evaluated by the Student's t or Wilcoxon tests. RESULTS: In 30 adult patients the median of ideal FiO2 was 25% (IQ25%-75% 23-28). This was significantly lower than baseline FiO2 (40%) (p< 0.001). No significant difference was found in the PaO2/ FiO2 ratio between baseline FiO2 (269±53) and ideal FiO2 (268±47). Tidal volume was significantly lower during use of ideal FiO2 (p=0.003) and blood pressure was significantly higher during use of baseline FiO2 (p=0.041), but there was no clinical significance. The remaining variables were not affected by reduction in FiO2. The ideal FiO2 did not influence remaining variables. CONCLUSIONS: These results suggest that FiO2 levels sufficient to ensure a SpO2>92% did not alter breathing patterns or trigger clinical changes in weaning patients.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)