You searched for:"Orlei Ribeiro de Araujo"
We found (5) results for your search.-
Original Article
Extracorporeal membrane oxygenation for respiratory failure in children: the years before and after the 2009 H1N1 pandemic
Rev Bras Ter Intensiva. 2021;33(4):544-548
Abstract
Original ArticleExtracorporeal membrane oxygenation for respiratory failure in children: the years before and after the 2009 H1N1 pandemic
Rev Bras Ter Intensiva. 2021;33(4):544-548
DOI 10.5935/0103-507X.20210082
Views0ABSTRACT
Objective:
To evaluate whether there was any impact on the number of pediatric extracorporeal membrane oxygenation runs and survival rates in the years subsequent to the 2009 pandemic.
Methods:
We studied two different periods of extracorporeal membrane oxygenation support for respiratory failure in children by analyzing datasets from the Extracorporeal Life Support Organization. Autoregressive integrated moving average models were constructed to estimate the effect of the pandemic. The year 2009 was the year of intervention (the H1N1 epidemic) in an interrupted time series model. Data collected from 2001 – 2010 were considered preintervention, and data collected from 2010 – 2017 were considered postintervention.
Results:
There was an increase in survival rates in the period 2010 – 2017 compared to 2001 – 2010 (p < 0.0001), with a significant improvement in survival when extracorporeal membrane oxygenation was performed for acute respiratory failure due to viral pneumonia. The autoregressive integrated moving average model shows an increase of 23 extracorporeal membrane oxygenation runs per year, prior to the point of the level effect (2009). In terms of survival, the preslope shows that there was no significant increase in survival rates before 2009 (p = 0.41), but the level effect was nearly significant after two years (p = 0.05), with a 6% increase in survival. In four years, there was an 8% (p = 0.03) increase in survival, and six years after 2009, there was up to a 10% (p = 0.026) increase in survival.
Conclusion:
In the years following 2009, there was a significant, global incremental increase in the extracorporeal membrane oxygenation survival rates for all runs, mainly due to improvements in the technology and treatment protocols for acute respiratory failure related to viral pneumonia and other respiratory conditions.
Keywords:ARDSChildExtracorporeal membrane oxygenationH1N1H1N1 SubtypeHumanInfluenzaInfluenza A virusPandemicsRespiratory distress syndromeRespiratory insufficiencySurvival rateSee more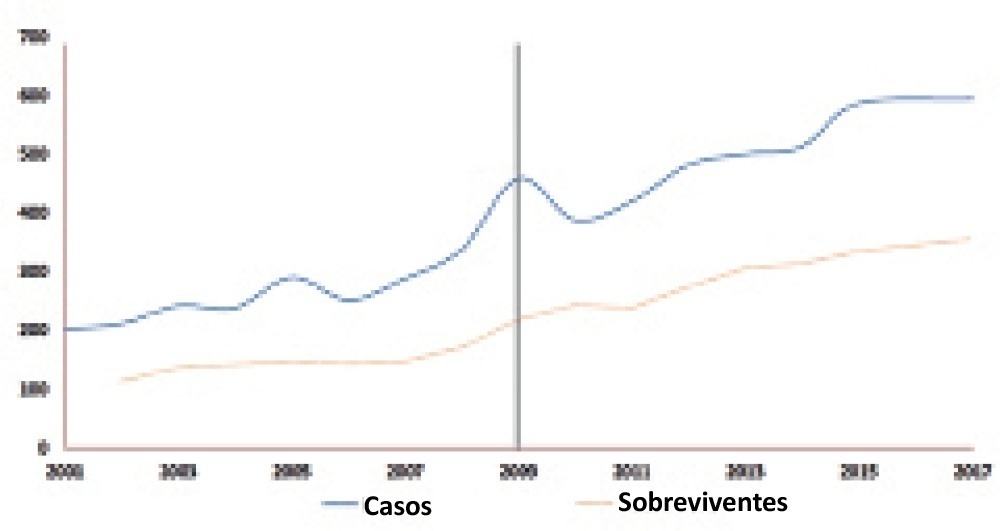
-
Original Article
Clinical practices related to high-flow nasal cannulas in pediatric critical care in Brazil compared to other countries: a Brazilian survey
Rev Bras Ter Intensiva. 2021;33(3):384-393
Abstract
Original ArticleClinical practices related to high-flow nasal cannulas in pediatric critical care in Brazil compared to other countries: a Brazilian survey
Rev Bras Ter Intensiva. 2021;33(3):384-393
DOI 10.5935/0103-507X.20210055
Views1ABSTRACT
Objective:
To describe current clinical practices related to the use of high-flow nasal cannula therapy by Brazilian pediatric intensivists and compare them with those in other countries.
Methods:
A questionnaire was administered to pediatric intensivists in North and South America, Asia, Europe, and Australia/New Zealand for the main study. We compared the Brazilian cohort with cohorts in the United States of America, Canada, the United Kingdom, and India
Results:
Overall, 501 physicians responded, 127 of which were in Brazil. Only 63.8% of respondents in Brazil had a high-flow nasal cannula available, in contrast to 100% of respondents in the United Kingdom, Canada, and the United States. The attending physician was responsible for the decision to start a high-flow nasal cannula according to 61.2% respondents in Brazil, 95.5% in the United Kingdom, 96.6% in the United States, 96.8% in Canada, and 84.7% in India. A total of 62% of respondents in Brazil, 96.3% in the United Kingdom, 96.6% in the United States, 96.8% in Canada, and 84.7% in India reported that the attending physician was responsible for the decision to wean or modify the high-flow nasal cannula settings. When high-flow nasal cannula therapy failed due to respiratory distress/failure, 82% of respondents in Brazil would consider a trial of noninvasive ventilation before endotracheal intubation, compared to 93% in the United Kingdom, 88% in the United States, 91.5% in Canada, and 76.8% in India. More Brazilian intensivists (6.5%) than intensivists in the United Kingdom, United States, and India (1.6% for all) affirmed using sedatives frequently with high-flow nasal cannulas.
Conclusion:
The availability of high-flow nasal cannulas in Brazil is still not widespread. There are some divergences in clinical practices between Brazilian intensivists and their colleagues abroad, mainly in processes and decision-making about starting and weaning high-flow nasal cannula therapy.
Keywords:BrazilCanadaCannulaIndiaIntensive careIntensive care units, pediatricNoninvasive ventilationOxygen inhalation therapyRespiratory insufficiencySurveys and questionnairesUnited KingdomUnited StatesSee more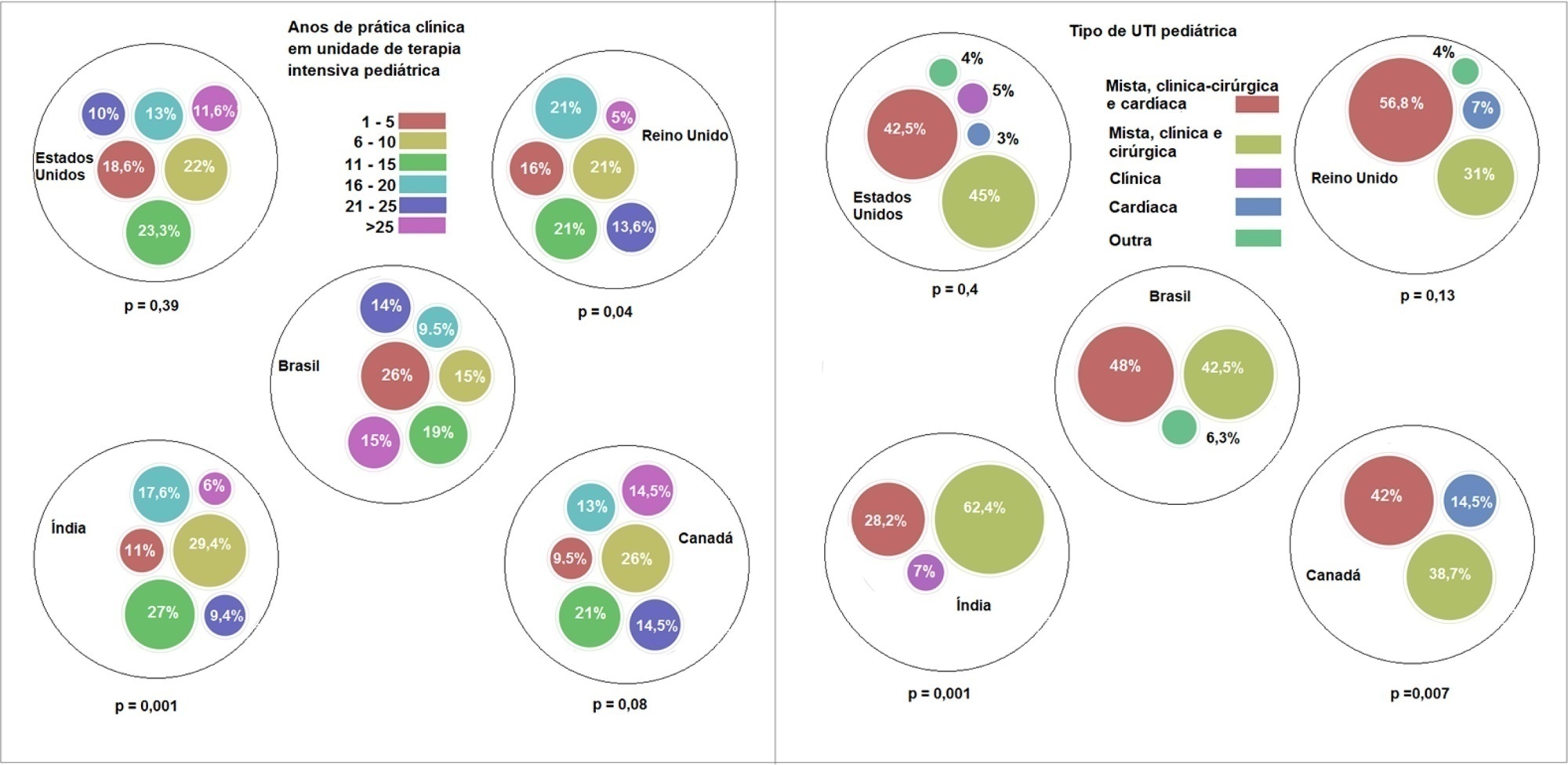
-
Original Articles
Sepsis-related acute respiratory distress syndrome in children with cancer: the respiratory dynamics of a devastating condition
Rev Bras Ter Intensiva. 2016;28(4):436-443
Abstract
Original ArticlesSepsis-related acute respiratory distress syndrome in children with cancer: the respiratory dynamics of a devastating condition
Rev Bras Ter Intensiva. 2016;28(4):436-443
DOI 10.5935/0103-507X.20160077
Views0See moreABSTRACT
Objective:
To evaluate the clinical course and respiratory parameters of mechanically ventilated children with cancer suffering from sepsis-related acute respiratory distress syndrome.
Methods:
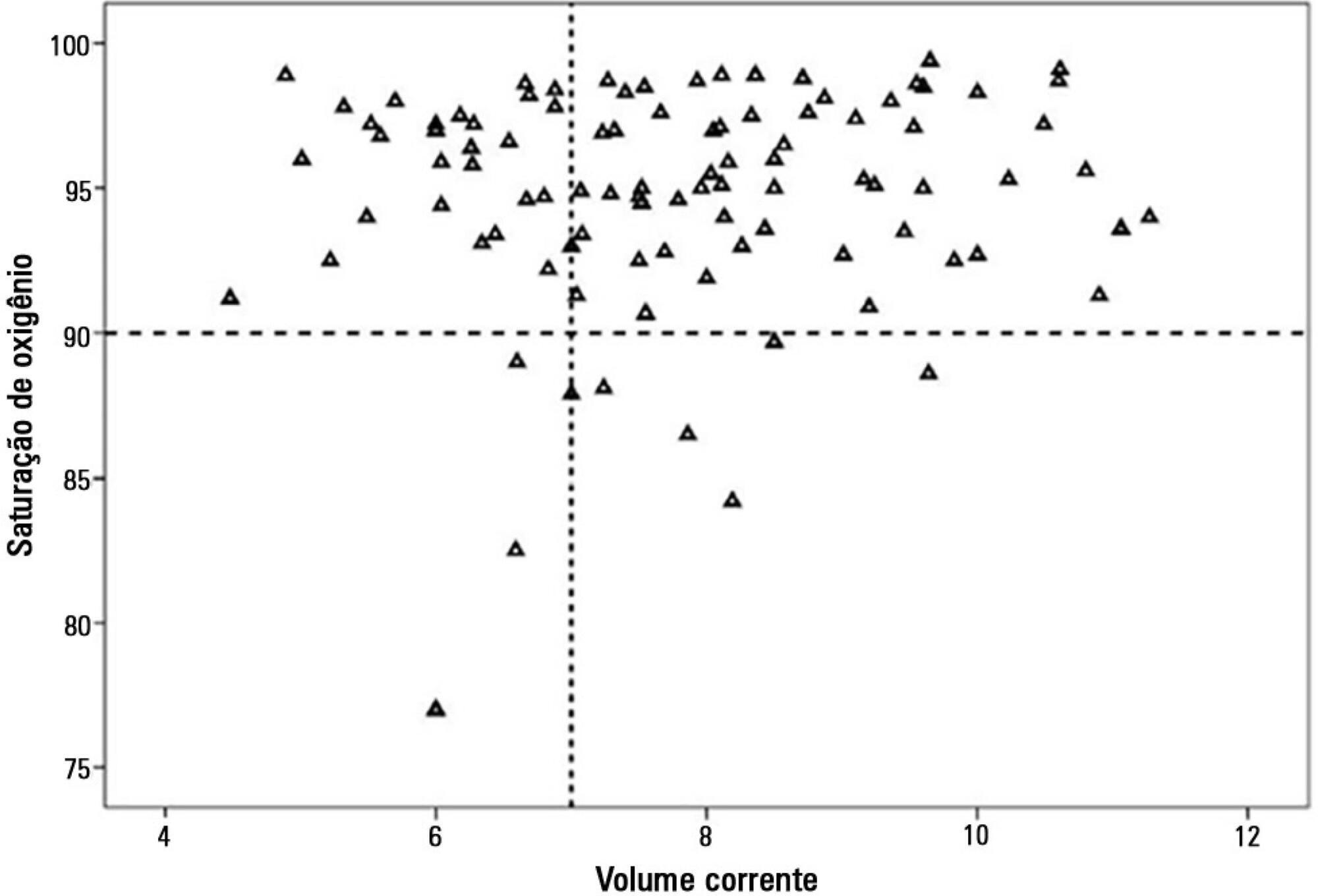
This 2-year prospective, longitudinal, observational cohort study enrolled 29 children and adolescents. Clinical data, measurements of blood gases and ventilation parameters were collected at four different time points. Fluctuations between measurements as well as differences in estimated means were analyzed by linear mixed models in which death within 28 days from the onset of acute respiratory distress syndrome was the primary endpoint.
Results:
There were 17 deaths within 28 days of acute respiratory distress syndrome onset and another 7 between 29 – 60 days. Only 5 patients survived for more than 60 days. Nine (31%) patients died as a direct consequence of refractory hypoxemia, and the others died of multiple organ failure and catecholamine-refractory shock. In 66% of the measurements, the tidal volume required to obtain oxygen saturation equal to or above 90% was greater than 7mL/kg. The estimated means of dynamic compliance were low and were similar for survivors and non-survivors but with a negative slope between the first and final measurements, accompanied by a negative slope of the tidal volume for non-survivors. Non-survivors were significantly more hypoxemic, with PaO2/FiO2 ratios showing lower estimated means and a negative slope along the four measurements. Peak, expiratory and mean airway pressures showed positive slopes in the non-survivors, who also had more metabolic acidosis.
Conclusions:
In most of our children with cancer, sepsis and acute respiratory distress syndrome progressed with deteriorating ventilation indexes and escalating organic dysfunction, making this triad nearly fatal in children.
-
Original Articles – Clinical Research
Intermittent heparin is not effective at preventing the occlusion of peripherally inserted central venous catheters in preterm and term neonates
Rev Bras Ter Intensiva. 2011;23(3):335-340
Abstract
Original Articles – Clinical ResearchIntermittent heparin is not effective at preventing the occlusion of peripherally inserted central venous catheters in preterm and term neonates
Rev Bras Ter Intensiva. 2011;23(3):335-340
DOI 10.1590/S0103-507X2011000300012
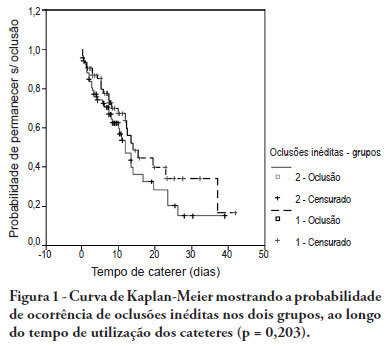
Views0See moreOBJECTIVE: To evaluate the effectiveness of intermittent 10 U/mL heparin flushes in reducing the occlusion of peripherally inserted central catheters in neonates. METHODS: In this randomized, open-label, prospective, controlled study, neonates were allocated either to receive 0.5 mL flushes of heparin (Group 1: n = 64) or saline (Group 2: n = 69) every 4 hours. Actions were taken to restore patency by using negative pressure (3-way stopcock method) in cases of occlusion. RESULTS: A total of 133 neonates were included. No significant intergroup difference was observed in the number of new occlusions (26 in Group 1, or 31/1,000 catheter-days; 36 in Group 2, or 36/1,000 catheter-days; P = 0.19). In Group 1, 5 catheters had 9 recurrent obstructions after successful clearance maneuvers. In Group 2, 19 catheters had 40 relapses (P < 0.0001), showing heparin's protective role against recurrence of obstruction (Relative Risk = 0.36). However, heparin failed to prevent catheter withdrawal due to permanent occlusion (3 catheters in Group 1 and 8 in Group 2; P = 0.24). CONCLUSION: Intermittent heparin is not effective for preventing the occlusion of peripherally inserted central catheters in neonates but reduces relapses when clearance maneuvers were successful
-
Original Articles
Cesarean deliveries and other risks for persistent pulmonary hypertension of the newborn
Rev Bras Ter Intensiva. 2008;20(4):394-397
Abstract
Original ArticlesCesarean deliveries and other risks for persistent pulmonary hypertension of the newborn
Rev Bras Ter Intensiva. 2008;20(4):394-397
DOI 10.1590/S0103-507X2008000400012
Views0See moreOBJECTIVES: To evaluate risks for persistent pulmonary hypertension in the newborn, confirmed by echocardiography, associated with cesarean deliveries and other factors. METHODS: Cohort of all deliveries >36 weeks within a period of 23 months. A nested case-control study was performed in a subset of the cohort, involving newborns admitted into neonatal intensive care unit with diagnosis of persistent pulmonary hypertension matched with normal controls, with application of questionnaires to mothers to identify risks. Logistic regression was used to calculate odds ratios. RESULTS: From 9452 newborns, 8388 (88.7%) were delivered by cesarean and 1064 (11.3%) by vaginal delivery. Questionnaires were applied to 173 mothers. Infants from cesareans had a fivefold increased risk of persistent pulmonary hypertension of the newborn: 42 (0.5%) versus 1 case (0.09%) in the vaginal group (OR 5.32, p=0.027). No interactions were found between smoking, parity, arterial hypertension and labor before cesarean section and persistent pulmonary hypertension of the newborn. First minute Apgar score <7 and maternal diabetes were related to increased risk. CONCLUSION: Reducing cesarean deliveries could prevent many cases of serious persistent pulmonary hypertension of the newborn.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




