Abstract
Rev Bras Ter Intensiva. 2011;23(3):335-340
DOI 10.1590/S0103-507X2011000300012
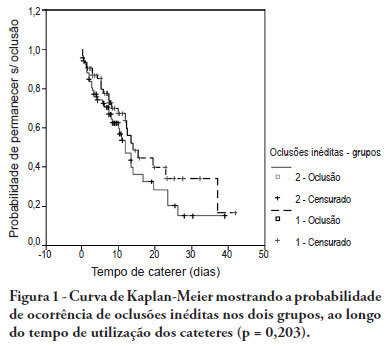
OBJECTIVE: To evaluate the effectiveness of intermittent 10 U/mL heparin flushes in reducing the occlusion of peripherally inserted central catheters in neonates. METHODS: In this randomized, open-label, prospective, controlled study, neonates were allocated either to receive 0.5 mL flushes of heparin (Group 1: n = 64) or saline (Group 2: n = 69) every 4 hours. Actions were taken to restore patency by using negative pressure (3-way stopcock method) in cases of occlusion. RESULTS: A total of 133 neonates were included. No significant intergroup difference was observed in the number of new occlusions (26 in Group 1, or 31/1,000 catheter-days; 36 in Group 2, or 36/1,000 catheter-days; P = 0.19). In Group 1, 5 catheters had 9 recurrent obstructions after successful clearance maneuvers. In Group 2, 19 catheters had 40 relapses (P < 0.0001), showing heparin's protective role against recurrence of obstruction (Relative Risk = 0.36). However, heparin failed to prevent catheter withdrawal due to permanent occlusion (3 catheters in Group 1 and 8 in Group 2; P = 0.24). CONCLUSION: Intermittent heparin is not effective for preventing the occlusion of peripherally inserted central catheters in neonates but reduces relapses when clearance maneuvers were successful
Abstract
Rev Bras Ter Intensiva. 2009;21(3):237-246
DOI 10.1590/S0103-507X2009000300002
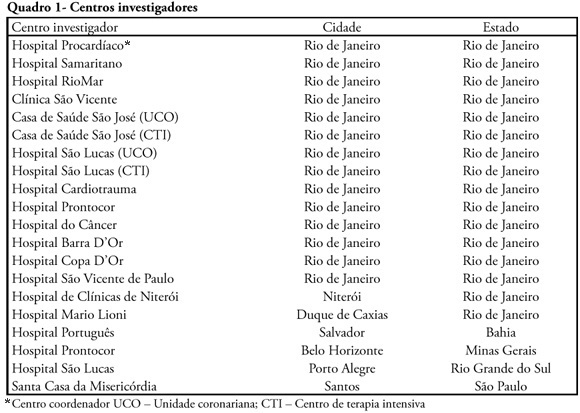
INTRODUCTION: The clinical profile as well as the therapeutic and diagnostic strategies for patients with pulmonary embolism, describes clinical practice in the approach of the disease. Such information, scarce in national studies, enables a better understanding of pulmonary embolism. METHODS: A multicenter trial included 727 patients with pulmonary embolism who were admitted in emergency or intensive care unit. Diagnostic criteria for inclusion were: 1. Visibility of thrombus in the pulmonary artery at pulmonary arteriography, helical computer tomography, magnetic resonance or echocardiogram. 2. High probability at pulmonary scintigraphy. 3. Venous duplex-scan with thrombus and clinical manifestations of pulmonary embolism. Clinical and complementary exams were analyzed. RESULTS: Mean age was 68 years, 42% were male. Most prevalent risk factors were: age>40 years, bed rest and neoplasm. More frequent signs and symptoms were: dyspnea, tachypnea, sinus tachycardia, and chest pain. Changes were observed at electrocardiogram in 30%, at chest X-ray in 45%, at venous duplex-scan in 67%, at transthoracic echocardiogram in 37%. . D-dimer, troponin I and CKMB were positive in, respectively, 93, 9 and 8%. Most frequently used methods to confirm diagnosis were helical computer tomography and non-fractioned heparin was the treatment most used. In-hospital mortality was 19.5%. CONCLUSIONS: It was observed that age>40 years, prolonged rest and neoplasms were the most prevalent risk factors and dyspnea and tachypnea were the more frequent clinical manifestations. Helical computer tomography was the most often used method to confirm diagnosis and non-fractioned heparin was the main form of treatment.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):165-172
DOI 10.1590/S0103-507X2008000200009
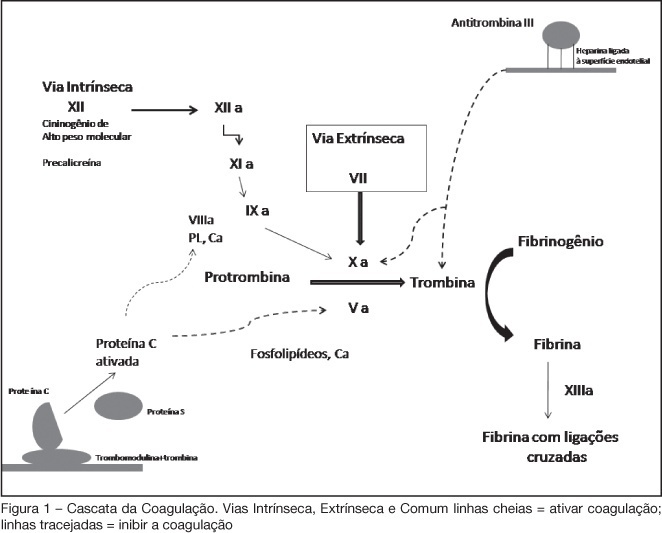
BACKGROUND AND OBJECTIVES: Acute coronary syndromes (ACS) are one of the most common causes of ICU admissions. New drugs have been developed for management of ACS. These drugs reduced morbidity and mortality; however their adverse effects or their incorrect use may cause excessive bleeding. The objective of this review is to present the principal peculiarities, doses, and indications of these drugs in ACS settings. METHODS: Original articles were retrieved crossing the terms acute coronary syndromes and antithrombotic therapy in the MedLine database as well as search for Brazilian and international guidelines in http://sumsearch.uthscsa.edu. RESULTS: In the treatment of acute coronary syndromes with non-ST-segment elevation enoxaparin was as efficient as UFH, but with a simpler management (SYNERGY and A to Z studies). In this same setting, fondaparinux was non inferior to enoxaparin and had lesser bleedings (OASIS 5), bivalirudin, combined or not with GPIIbIIIa blockers, was not inferior when compared with other heparins (ACUITY). In ST-segment elevation ACS, enoxaparin was superior to HNF in patients treated with fibrinolysis (EXTRACT TIMI 25); in OASIS 6 fondaparinux was superior to UFH in patients treated with thrombolytic therapy and not submitted to reperfusion. CONCLUSIONS: The correct management and individual combination of antithrombotic drugs are mandatory for decreased mortality and of major cardiovascular events, reducing the undesirable risk of additional bleeding.