Abstract
Rev Bras Ter Intensiva. 2014;26(1):36-43
DOI 10.5935/0103-507X.20140006
To assess the performance of the Nursing Activities Score in a pediatric intensive care unit, compare its scores expressed as time spent on nursing activities to the corresponding ones calculated using the Simplified Therapeutic Intervention Scoring System, and correlate the results obtained by both instruments with severity, morbidity and mortality.
Prospective, observational, and analytical cohort study conducted at a type III general pediatric intensive care unit. The study participants were all the children aged 29 days to 12 years admitted to the investigated pediatric intensive care unit from August 2008 to February 2009.
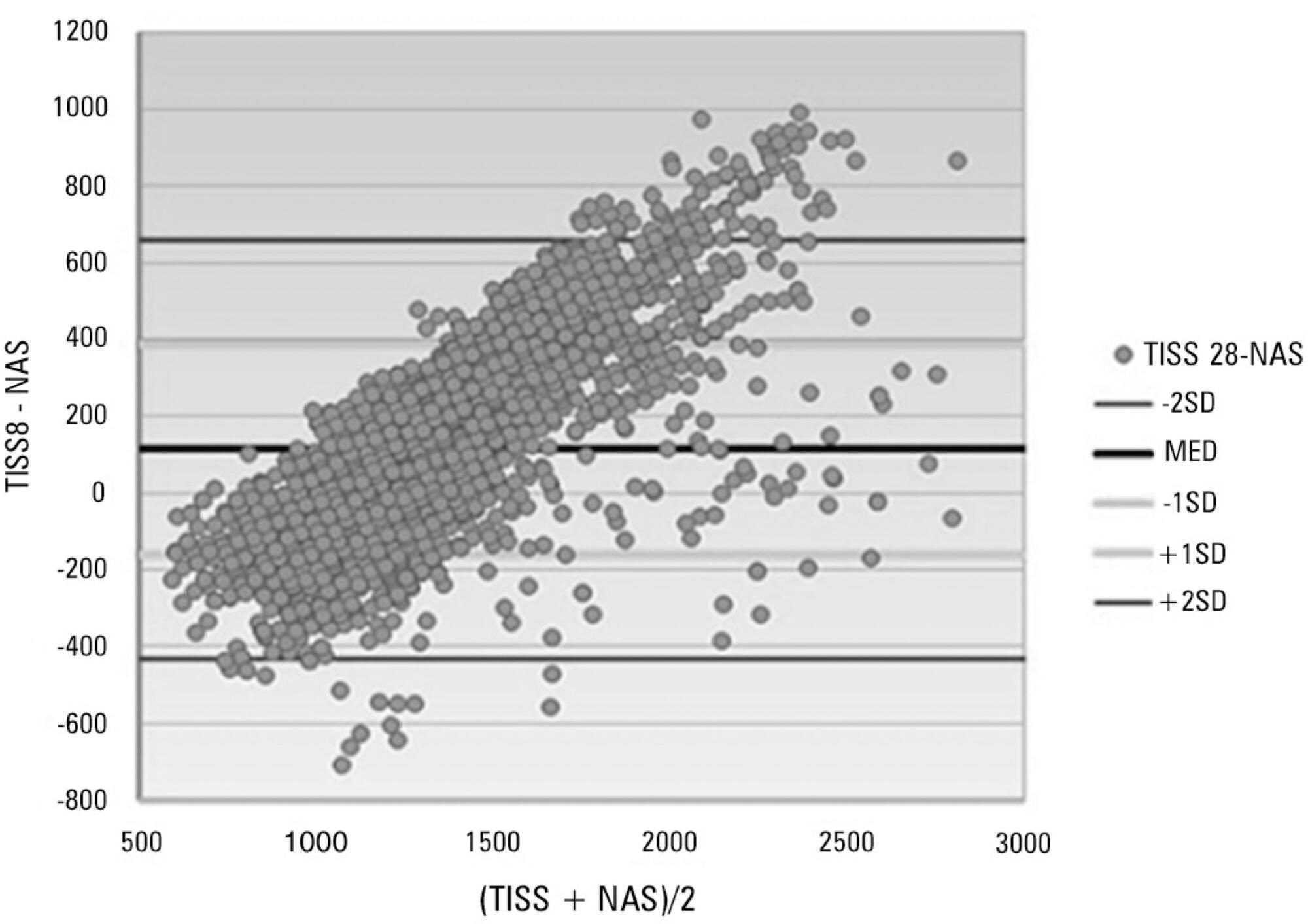
A total of 545 patients were studied, which corresponded to 2,951 assessments. The average score of the Simplified Therapeutic Intervention Scoring System was 28.79±10.37 (915±330 minutes), and that of the Nursing Activities Score was 55.6±11.82 (802±161 minutes). The number of minutes that resulted from the conversion of the Simplified Therapeutic Intervention Scoring System score was higher compared to that resulting from the Nursing Activities Score for all the assessments (p<0.001). The correlation between the instruments was significant, direct, positive, and moderate (R=0.564).
The agreement between the investigated instruments was satisfactory, and both instruments also exhibited satisfactory discrimination of mortality; for that purpose, the best cutoff point was 16 nursing hours/patient day.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):335-340
DOI 10.1590/S0103-507X2011000300012
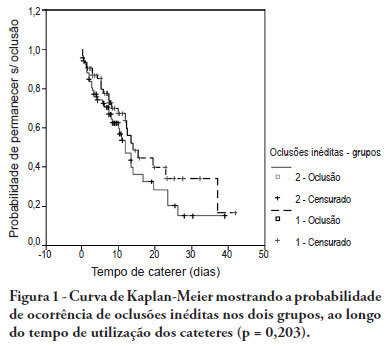
OBJECTIVE: To evaluate the effectiveness of intermittent 10 U/mL heparin flushes in reducing the occlusion of peripherally inserted central catheters in neonates. METHODS: In this randomized, open-label, prospective, controlled study, neonates were allocated either to receive 0.5 mL flushes of heparin (Group 1: n = 64) or saline (Group 2: n = 69) every 4 hours. Actions were taken to restore patency by using negative pressure (3-way stopcock method) in cases of occlusion. RESULTS: A total of 133 neonates were included. No significant intergroup difference was observed in the number of new occlusions (26 in Group 1, or 31/1,000 catheter-days; 36 in Group 2, or 36/1,000 catheter-days; P = 0.19). In Group 1, 5 catheters had 9 recurrent obstructions after successful clearance maneuvers. In Group 2, 19 catheters had 40 relapses (P < 0.0001), showing heparin's protective role against recurrence of obstruction (Relative Risk = 0.36). However, heparin failed to prevent catheter withdrawal due to permanent occlusion (3 catheters in Group 1 and 8 in Group 2; P = 0.24). CONCLUSION: Intermittent heparin is not effective for preventing the occlusion of peripherally inserted central catheters in neonates but reduces relapses when clearance maneuvers were successful
Abstract
Rev Bras Ter Intensiva. 2010;22(4):346-350
DOI 10.1590/S0103-507X2010000400006
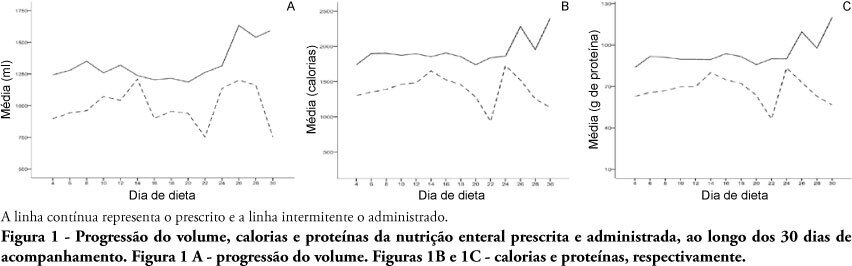
OBJECTIVES: Different conditions require that critically ill patients to receive lower than prescribed enteral nutrition volumes, energy and protein. This study objective was to evaluate the prescribed versus administered enteral nutrition difference in adults admitted to an intensive care unit. METHODS: In 2009, patients were followed for 30 days from the start of enteral nutrition to its discontinuation, or discharge from the intensive care unit. Parametric and nonparametric tests were used to evaluate prescribed versus administered differences. RESULTS: Eighty five patients were enrolled; mean age was 58.6±18.0 years and 40% were male. The patients remained in hospital for 29.5 days (IQ: 15.2 - 48.7) and were under enteral nutrition for 10 (IQ: 4.2 - 27.5) days. Lower than enteral nutrition prescribed volume (-428±243ml/day), energy (-665±412 Kcal/day) and protein (-30±19 g protein/day) was received. Individual patients' evaluation demonstrated that about 40% of the prescribed volume was not actually given. The main reasons for enteral nutrition interruptions were nausea and vomiting, abdominal distension, constipation and clinical complications (52%); diagnostic procedures (41.6%); and transition to oral feeding (5.6%). CONCLUSION: Patients admitted to intensive care unit receive less than the prescribed enteral nutrition. The routine care and gastrointestinal tract complications lead to enteral nutrition interruptions, contributing to less than prescribed calories administration.