Abstract
Rev Bras Ter Intensiva. 2015;27(4):412-415
DOI 10.5935/0103-507X.20150069
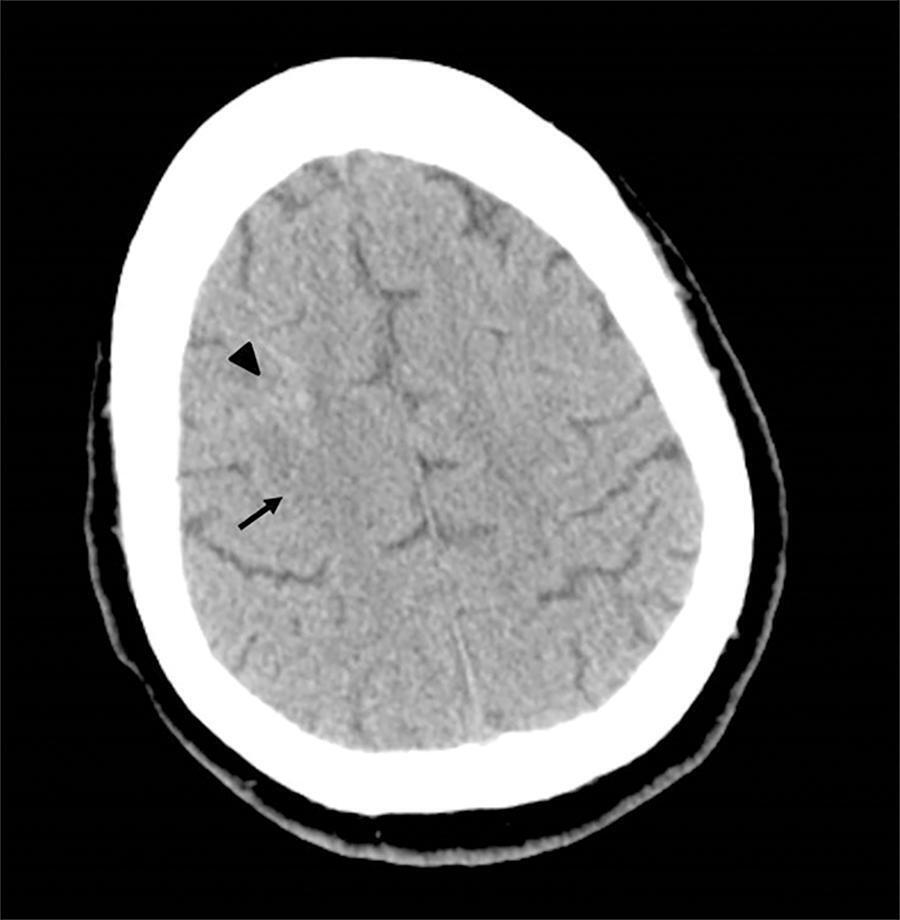
We report the case of a 2-year-old child who survived an acute episode of severe spontaneous intracranial hemorrhage with clinical and radiological signs of intracranial hypertension and transtentorial herniation. The patient underwent emergency surgery to drain the hematoma, and a catheter was inserted to monitor intracranial pressure. In the initial computed tomography analysis performed prior to hematoma drainage, a brain cyst was evident contralateral to the hematoma, which, based on the analysis by the care team, possibly helped to avoid a worse outcome because the cyst accommodated the brain after the massive hemorrhage. After the investigation, the patient was determined to have previously undiagnosed hemophilia A. The patient underwent treatment in intensive care, which included the control of intracranial pressure, factor VIII replacement and discharge without signs of neurological impairment.

Abstract
Rev Bras Ter Intensiva. 2015;27(2):185-189
DOI 10.5935/0103-507X.20150031
This is a case report of a 43-year-old Caucasian male with end-stage renal disease being treated with hemodialysis and infective endocarditis in the aortic and tricuspid valves. The clinical presentation was dominated by neurologic impairment with cerebral embolism and hemorrhagic components. A thoracoabdominal computerized tomography scan revealed septic pulmonary embolus. The patient underwent empirical antibiotherapy with ceftriaxone, gentamicin and vancomycin, and the therapy was changed to flucloxacilin and gentamicin after the isolation of S. aureus in blood cultures. The multidisciplinary team determined that the patient should undergo valve replacement after the stabilization of the intracranial hemorrhage; however, on the 8th day of hospitalization, the patient entered cardiac arrest due to a massive septic pulmonary embolism and died. Despite the risk of aggravation of the hemorrhagic cerebral lesion, early surgical intervention should be considered in high-risk patients.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):415-419
DOI 10.1590/S0103-507X2012000400020
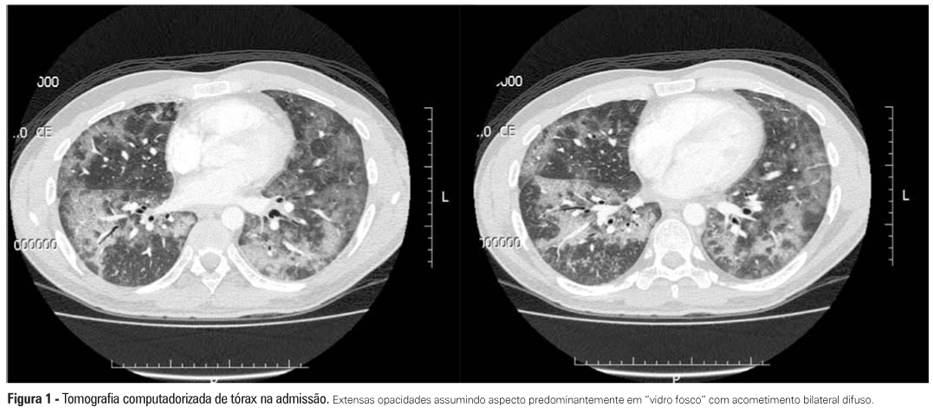
Interstitial lung diseases belong to a group of diseases that typically exhibit a subacute or chronic progression but that may cause acute respiratory failure. The male patient, who was 37 years of age and undergoing therapy for non-Hodgkin's lymphoma, was admitted with cough, fever, dyspnea and acute hypoxemic respiratory failure. Mechanical ventilation and antibiotic therapy were initiated but were associated with unfavorable progression. Thoracic computed tomography showed bilateral pulmonary "ground glass" opacities. Methylprednisolone pulse therapy was initiated with satisfactory response because the patient had used three drugs related to organizing pneumonia (cyclophosphamide, doxorubicin and rituximab), and the clinical and radiological symptoms were suggestive. Organizing pneumonia may be idiopathic or linked to collagen diseases, drugs and cancer and usually responds to corticosteroid therapy. The diagnosis was anatomopathological, but the patient's clinical condition precluded performing a lung biopsy. Organizing pneumonia should be a differential diagnosis in patients with apparent pneumonia and a progression that is unfavorable to antimicrobial treatment.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):43-51
DOI 10.1590/S0103-507X2012000100007
OBJECTIVE: The objective of this study was to assess the effects of positive end-expiratory pressure on recruitment, cyclic recruitment and derecruitment and strain in patients with acute lung injury and acute respiratory distress syndrome using lung computed tomography. METHODS: This is an open, controlled, non-randomized interventional study of ten patients with acute lung injury and acute respiratory distress syndrome. Using computed tomography, single, basal slices of the lung were obtained during inspiratory and expiratory pauses at a tidal volume of 6 ml/kg and a positive end-expiratory pressure of 5, 10, 15 and 20 cmH2O. The densities of the lung parenchyma were measured in Hounsfield units. The values for positive end-expiratory pressure-induced recruitment, cyclic recruitment and derecruitment and strain were then calculated. RESULTS: Increasing levels of positive end-expiratory pressure were correlated with increased recruitment and global strain (p < 0.01), which was significantly correlated with plateau pressure (r² = 0.97, p < 0.01). In addition, increasing levels of positive end-expiratory pressure systematically increased strain along the sternovertebral axis. CONCLUSION: While strain is an adverse effect of positive end-expiratory pressure, the decision use positive end-expiratory pressure with any patient should be balanced against the potential benefits of recruitment. Due to the small number of patients in this study, the present data should be treated as hypothesis generating and is not intended to limit the clinical application of a high level of positive end-expiratory pressure in patients with severe hypoxemia.

Abstract
Rev Bras Ter Intensiva. 2009;21(3):237-246
DOI 10.1590/S0103-507X2009000300002
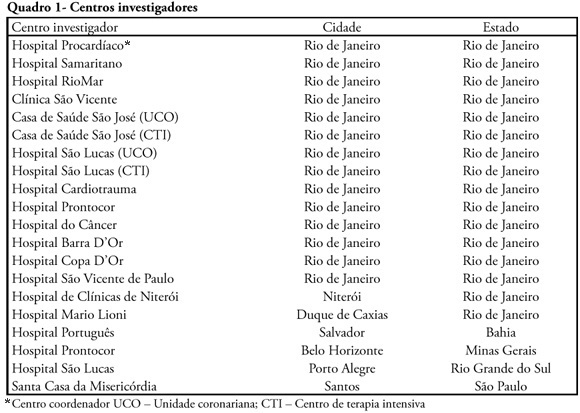
INTRODUCTION: The clinical profile as well as the therapeutic and diagnostic strategies for patients with pulmonary embolism, describes clinical practice in the approach of the disease. Such information, scarce in national studies, enables a better understanding of pulmonary embolism. METHODS: A multicenter trial included 727 patients with pulmonary embolism who were admitted in emergency or intensive care unit. Diagnostic criteria for inclusion were: 1. Visibility of thrombus in the pulmonary artery at pulmonary arteriography, helical computer tomography, magnetic resonance or echocardiogram. 2. High probability at pulmonary scintigraphy. 3. Venous duplex-scan with thrombus and clinical manifestations of pulmonary embolism. Clinical and complementary exams were analyzed. RESULTS: Mean age was 68 years, 42% were male. Most prevalent risk factors were: age>40 years, bed rest and neoplasm. More frequent signs and symptoms were: dyspnea, tachypnea, sinus tachycardia, and chest pain. Changes were observed at electrocardiogram in 30%, at chest X-ray in 45%, at venous duplex-scan in 67%, at transthoracic echocardiogram in 37%. . D-dimer, troponin I and CKMB were positive in, respectively, 93, 9 and 8%. Most frequently used methods to confirm diagnosis were helical computer tomography and non-fractioned heparin was the treatment most used. In-hospital mortality was 19.5%. CONCLUSIONS: It was observed that age>40 years, prolonged rest and neoplasms were the most prevalent risk factors and dyspnea and tachypnea were the more frequent clinical manifestations. Helical computer tomography was the most often used method to confirm diagnosis and non-fractioned heparin was the main form of treatment.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)