Home
Abstract
Rev Bras Ter Intensiva. 2020;32(4):592-602
DOI 10.5935/0103-507X.20200097
To systematically review the current evidence on the efficacy of milrinone in the treatment of cerebral vasospasm after subarachnoid hemorrhage.
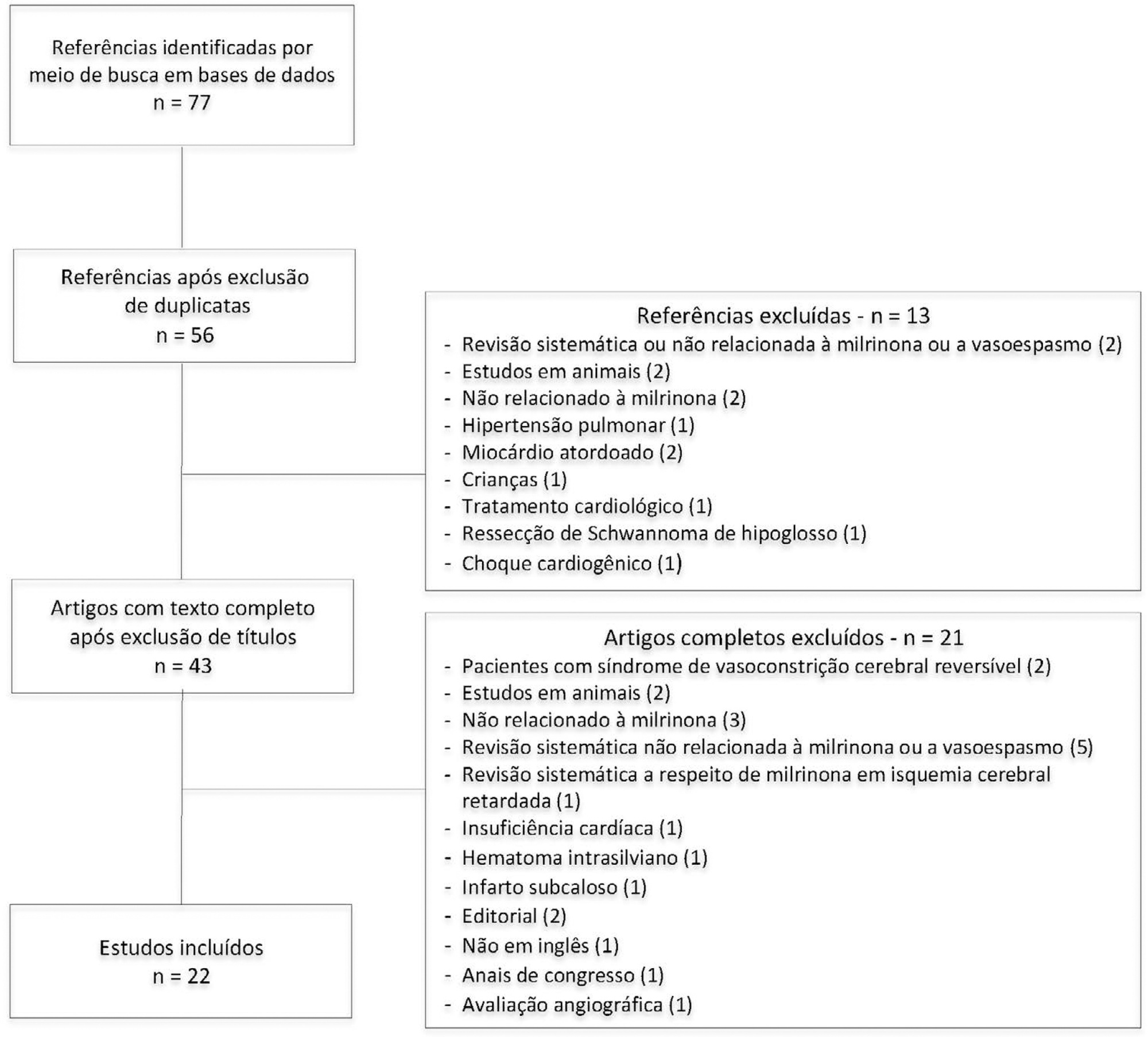
The Pubmed®, Cochrane and Embase databases were screened for articles published from April 2001 to February 2019. Two independent reviewers performed the methodological quality screening and data extraction of the studies.
Twenty-two studies were found to be relevant, and only one of these was a randomized control trial. Studies showed marked heterogeneity and weaknesses in key methodological criteria. Most patients presented with moderate to severe vasospasm. Angiography was the main method of diagnosing vasospasm. Intra-arterial administration of milrinone was performed in three studies, intravenous administration was performed in nine studies, and both routes of administration in six studies; the intrathecal route was used in two studies, the cisternal route in one study and endovascular administration in one study. The side effects of milrinone were described in six studies. Twenty-one studies indicated resolution of vasospasm.
The current evidence indicates that milrinone may have a role in treatment of vasospasm after aneurysmal subarachnoid hemorrhage. However, only one randomized control trial was performed, with a low quality level. Our findings indicate the need for future randomized control trials with patient-centered outcomes to provide definitive recommendations.


Abstract
Rev Bras Ter Intensiva. 2020;32(4):592-602
DOI 10.5935/0103-507X.20200097
To systematically review the current evidence on the efficacy of milrinone in the treatment of cerebral vasospasm after subarachnoid hemorrhage.
The Pubmed®, Cochrane and Embase databases were screened for articles published from April 2001 to February 2019. Two independent reviewers performed the methodological quality screening and data extraction of the studies.
Twenty-two studies were found to be relevant, and only one of these was a randomized control trial. Studies showed marked heterogeneity and weaknesses in key methodological criteria. Most patients presented with moderate to severe vasospasm. Angiography was the main method of diagnosing vasospasm. Intra-arterial administration of milrinone was performed in three studies, intravenous administration was performed in nine studies, and both routes of administration in six studies; the intrathecal route was used in two studies, the cisternal route in one study and endovascular administration in one study. The side effects of milrinone were described in six studies. Twenty-one studies indicated resolution of vasospasm.
The current evidence indicates that milrinone may have a role in treatment of vasospasm after aneurysmal subarachnoid hemorrhage. However, only one randomized control trial was performed, with a low quality level. Our findings indicate the need for future randomized control trials with patient-centered outcomes to provide definitive recommendations.


Abstract
Rev Bras Ter Intensiva. 2016;28(2):141-146
DOI 10.5935/0103-507X.20160028
To compare the clinical evolution of perimesencephalic subarachnoid hemorrhage and non-perimesencephalic subarachnoid hemorrhage.
The study was conducted retrospectively in a tertiary hospital center in the north region of Portugal. Included patients had no identifiable cause for subarachnoid hemorrhage. Several epidemiologic, clinical and imaging aspects were statistically analyzed, taking into account the differences in perimesencephalic subarachnoid hemorrhage and non-perimesencephalic subarachnoid hemorrhage.
Sixty-two patients met the inclusion criteria (46.8% - perimesencephalic subarachnoid hemorrhage; 53.2% - non-perimesencephalic subarachnoid hemorrhage). Demographic and clinical background characteristics were similar in both groups. Complications were more frequent in patients with non-perimesencephalic subarachnoid hemorrhage - 84.8% of the patients had at least one complication versus 48.3% in perimesencephalic subarachnoid hemorrhage. Vasospasm, infection and hydrocephaly were the most common complications (each was detected more frequently in the non-perimesencephalic subarachnoid hemorrhage group than in perimesencephalic subarachnoid hemorrhage group). Two patients died, both had a non-perimesencephalic subarachnoid hemorrhage. The median inpatient time was longer in the non-perimesencephalic subarachnoid hemorrhage group (21 versus 14 days). No incidents of rebleeding were reported during the follow-up period (mean time of 15 ± 10.3 months).
Perimesencephalic subarachnoid hemorrhage and non-perimesencephalic subarachnoid hemorrhage are two different entities that have different clinical outcomes, namely in terms of complication rate and median inpatient time. The management of these patients should respect this difference to improve treatment and optimize health care resources.


Abstract
Rev Bras Ter Intensiva. 2016;28(2):141-146
DOI 10.5935/0103-507X.20160028
To compare the clinical evolution of perimesencephalic subarachnoid hemorrhage and non-perimesencephalic subarachnoid hemorrhage.
The study was conducted retrospectively in a tertiary hospital center in the north region of Portugal. Included patients had no identifiable cause for subarachnoid hemorrhage. Several epidemiologic, clinical and imaging aspects were statistically analyzed, taking into account the differences in perimesencephalic subarachnoid hemorrhage and non-perimesencephalic subarachnoid hemorrhage.
Sixty-two patients met the inclusion criteria (46.8% - perimesencephalic subarachnoid hemorrhage; 53.2% - non-perimesencephalic subarachnoid hemorrhage). Demographic and clinical background characteristics were similar in both groups. Complications were more frequent in patients with non-perimesencephalic subarachnoid hemorrhage - 84.8% of the patients had at least one complication versus 48.3% in perimesencephalic subarachnoid hemorrhage. Vasospasm, infection and hydrocephaly were the most common complications (each was detected more frequently in the non-perimesencephalic subarachnoid hemorrhage group than in perimesencephalic subarachnoid hemorrhage group). Two patients died, both had a non-perimesencephalic subarachnoid hemorrhage. The median inpatient time was longer in the non-perimesencephalic subarachnoid hemorrhage group (21 versus 14 days). No incidents of rebleeding were reported during the follow-up period (mean time of 15 ± 10.3 months).
Perimesencephalic subarachnoid hemorrhage and non-perimesencephalic subarachnoid hemorrhage are two different entities that have different clinical outcomes, namely in terms of complication rate and median inpatient time. The management of these patients should respect this difference to improve treatment and optimize health care resources.


Search
Search in:
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis


