Abstract
Rev Bras Ter Intensiva. 2022;34(4):477-483
DOI 10.5935/0103-507X.20220280-en
To create and validate a model for predicting septic or hypovolemic shock from easily obtainable variables collected from patients at admission to an intensive care unit.
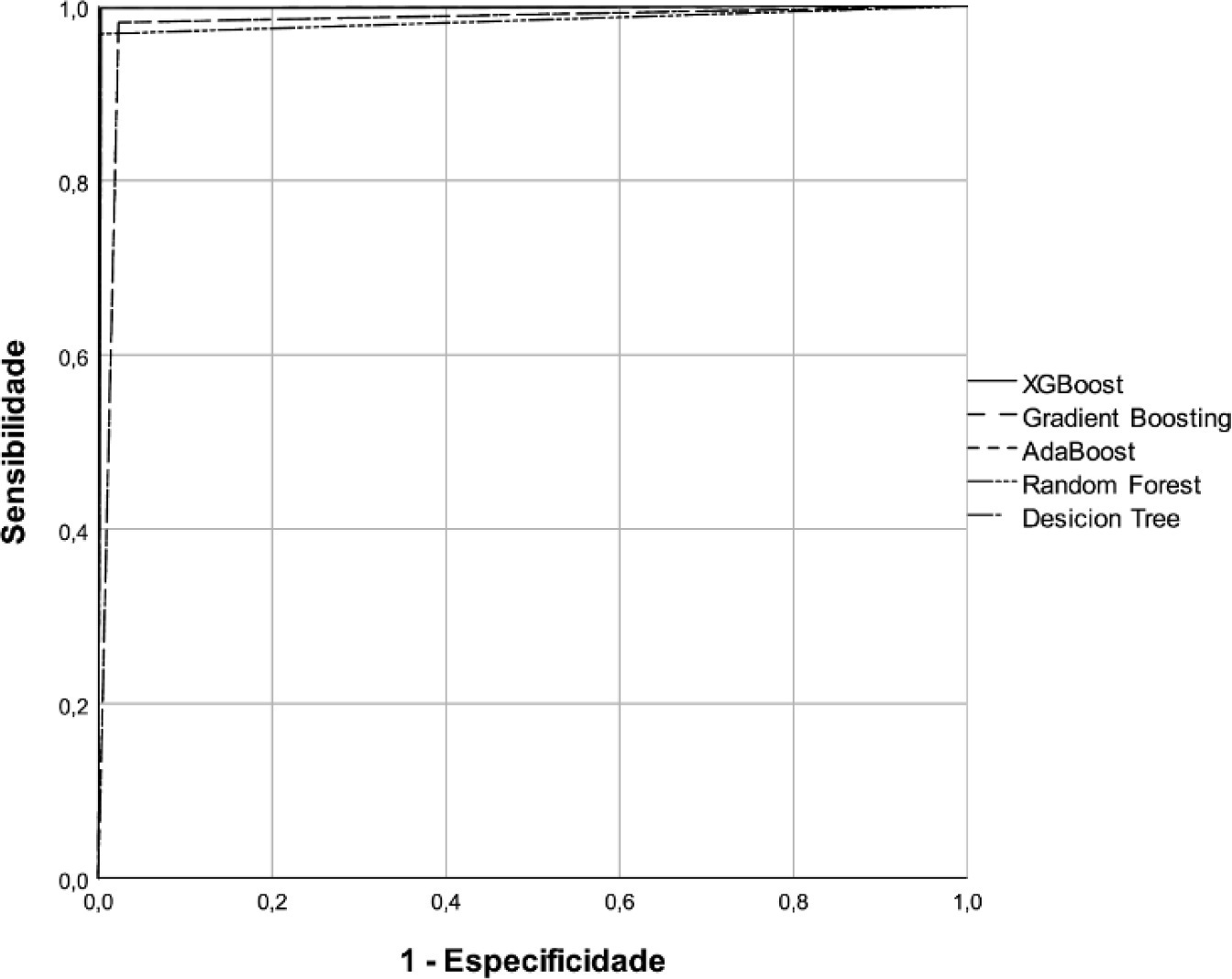
A predictive modeling study with concurrent cohort data was conducted in a hospital in the interior of northeastern Brazil. Patients aged 18 years or older who were not using vasoactive drugs on the day of admission and were hospitalized from November 2020 to July 2021 were included. The Decision Tree, Random Forest, AdaBoost, Gradient Boosting and XGBoost classification algorithms were tested for use in building the model. The validation method used was k-fold cross validation. The evaluation metrics used were recall, precision and area under the Receiver Operating Characteristic curve.
A total of 720 patients were used to create and validate the model. The models showed high predictive capacity with areas under the Receiver Operating Characteristic curve of 0.979; 0.999; 0.980; 0.998 and 1.00 for the Decision Tree, Random Forest, AdaBoost, Gradient Boosting and XGBoost algorithms, respectively.
The predictive model created and validated showed a high ability to predict septic and hypovolemic shock from the time of admission of patients to the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2022;34(2):272-278
DOI 10.5935/0103-507X.20220025-en
To translate, crossculturally adapt and evaluate the clinimetric properties of the Critical Care Functional Rehabilitation Outcome Measure for evaluating the functionality of patients admitted to intensive care units in Brazil.
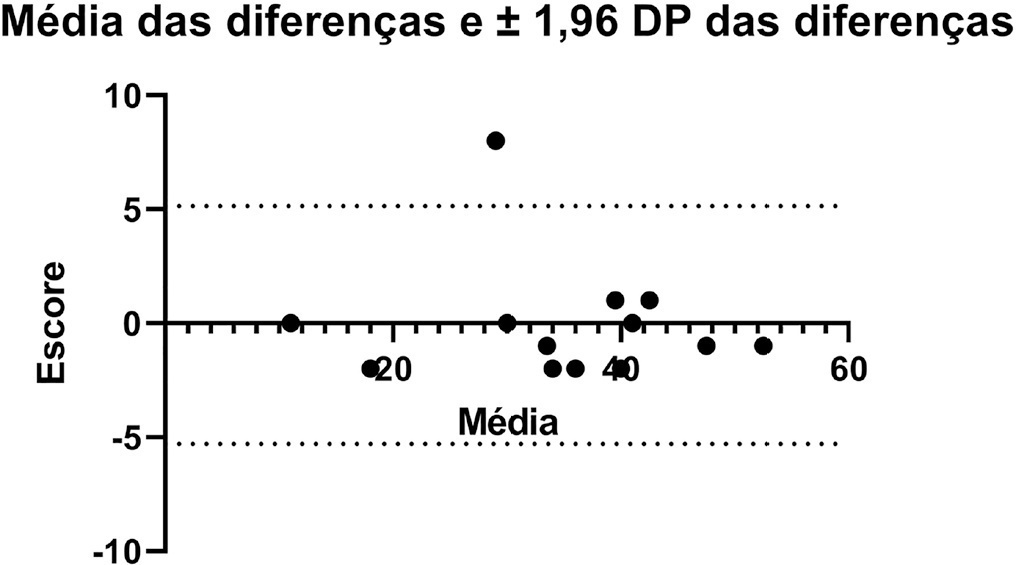
The process of translation and cross-cultural adaptation involved the following steps: initial translation, synthesis, back-translation, expert committee review and pretesting. The intra- and interrater reliability and agreement were analyzed between two physical therapists who evaluated the same group of patients (n = 35). The evaluations were performed by each therapist independently and blinded to the score assigned by the other professional. The qualitative analysis was performed by the review committee, and the experts adapted and synthesized the Portuguese translation of the Critical Care Functional Rehabilitation Outcome Measure.
There was agreement between the initial Brazilian translations of the Critical Care Functional Rehabilitation Outcome Measure scale. The conceptual, idiomatic, semantic and experimental equivalences between the original and translated versions were assessed, resulting in the final Brazilian version of the scale, called the Medida de Resultado da Reabilitação Funcional em Cuidados Intensivos. The evaluation of the clinimetric properties showed evidence of a high degree of agreement and reliability, as all had an intraclass correlation coefficient above 0.75. The overall intraclass correlation coefficient was 0.89.
The translated version of the Critical Care Functional Rehabilitation Outcome Measure scale for assessing the functionality of patients admitted to an intensive care unit can be used reliably in Brazil following translation and cross-cultural adaptation to Brazilian Portuguese and presents evidence of excellent interrater reliability.
Abstract
Rev Bras Ter Intensiva. 2016;28(2):114-119
DOI 10.5935/0103-507X.20160025
To evaluate the variation in mobility during hospitalization in an intensive care unit and its association with hospital mortality.
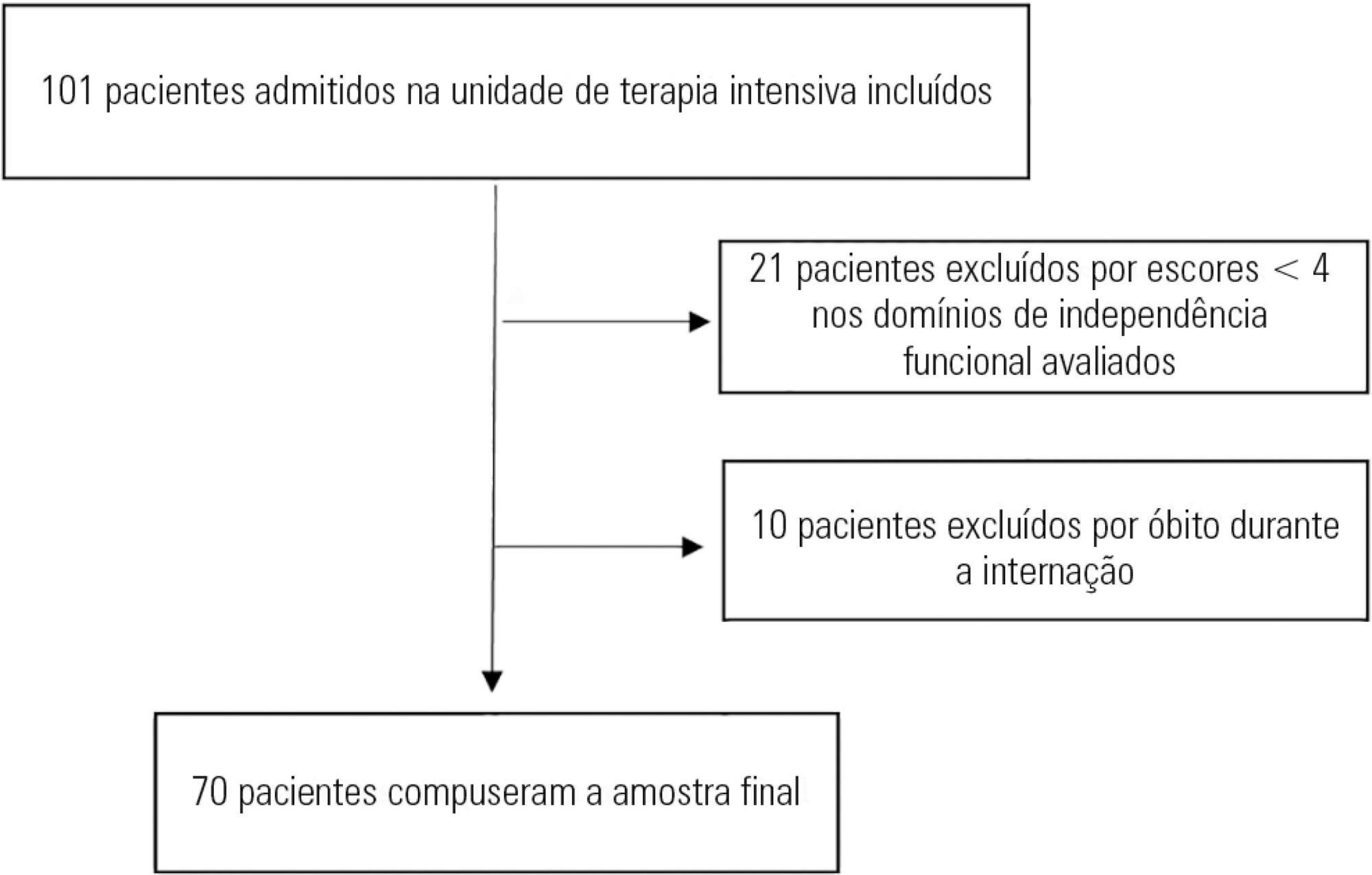
This prospective study was conducted in an intensive care unit. The inclusion criteria included patients admitted with an independence score of ≥ 4 for both bed-chair transfer and locomotion, with the score based on the Functional Independence Measure. Patients with cardiac arrest and/or those who died during hospitalization were excluded. To measure the loss of mobility, the value obtained at discharge was calculated and subtracted from the value obtained on admission, which was then divided by the admission score and recorded as a percentage.
The comparison of these two variables indicated that the loss of mobility during hospitalization was 14.3% (p < 0.001). Loss of mobility was greater in patients hospitalized for more than 48 hours in the intensive care unit (p < 0.02) and in patients who used vasopressor drugs (p = 0.041). However, the comparison between subjects aged 60 years or older and those younger than 60 years indicated no significant differences in the loss of mobility (p = 0.332), reason for hospitalization (p = 0.265), SAPS 3 score (p = 0.224), use of mechanical ventilation (p = 0.117), or hospital mortality (p = 0.063).
There was loss of mobility during hospitalization in the intensive care unit. This loss was greater in patients who were hospitalized for more than 48 hours and in those who used vasopressors; however, the causal and prognostic factors associated with this decline need to be elucidated.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):235-239
DOI 10.5935/0103-507X.20150043
To evaluate the association between the in-hospital mortality of patients hospitalized due to respiratory diseases and the availability of intensive care units.
This retrospective cohort study evaluated a database from a hospital medicine service involving patients hospitalized due to respiratory non-terminal diseases. Data on clinical characteristics and risk factors associated with mortality, such as Charlson score and length of hospital stay, were collected. The following analyses were performed: univariate analysis with simple stratification using the Mantel Haenszel test, chi squared test, Student’s t test, Mann-Whitney test, and logistic regression.
Three hundred thirteen patients were selected, including 98 (31.3%) before installation of the intensive care unit and 215 (68.7%) after installation of the intensive care unit. No significant differences in the clinical and anthropometric characteristics or risk factors were observed between the groups. The mortality rate was 18/95 (18.9%) before the installation of the intensive care unit and 21/206 (10.2%) after the installation of the intensive care unit. Logistic regression analysis indicated that the probability of death after the installation of the intensive care unit decreased by 58% (OR: 0.42; 95%CI 0.205 -0.879; p = 0.021).
Considering the limitations of the study, the results suggest a benefit, with a decrease of one death per every 11 patients treated for respiratory diseases after the installation of an intensive care unit in our hospital. The results corroborate the benefits of the implementation of intensive care units in secondary hospitals.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):347-352
DOI 10.5935/0103-507X.20150059
The positioning of a patient in bed may directly affect their respiratory mechanics. The objective of this study was to evaluate the respiratory mechanics of mechanically ventilated patients positioned with different head angles hospitalized in an intensive care unit.
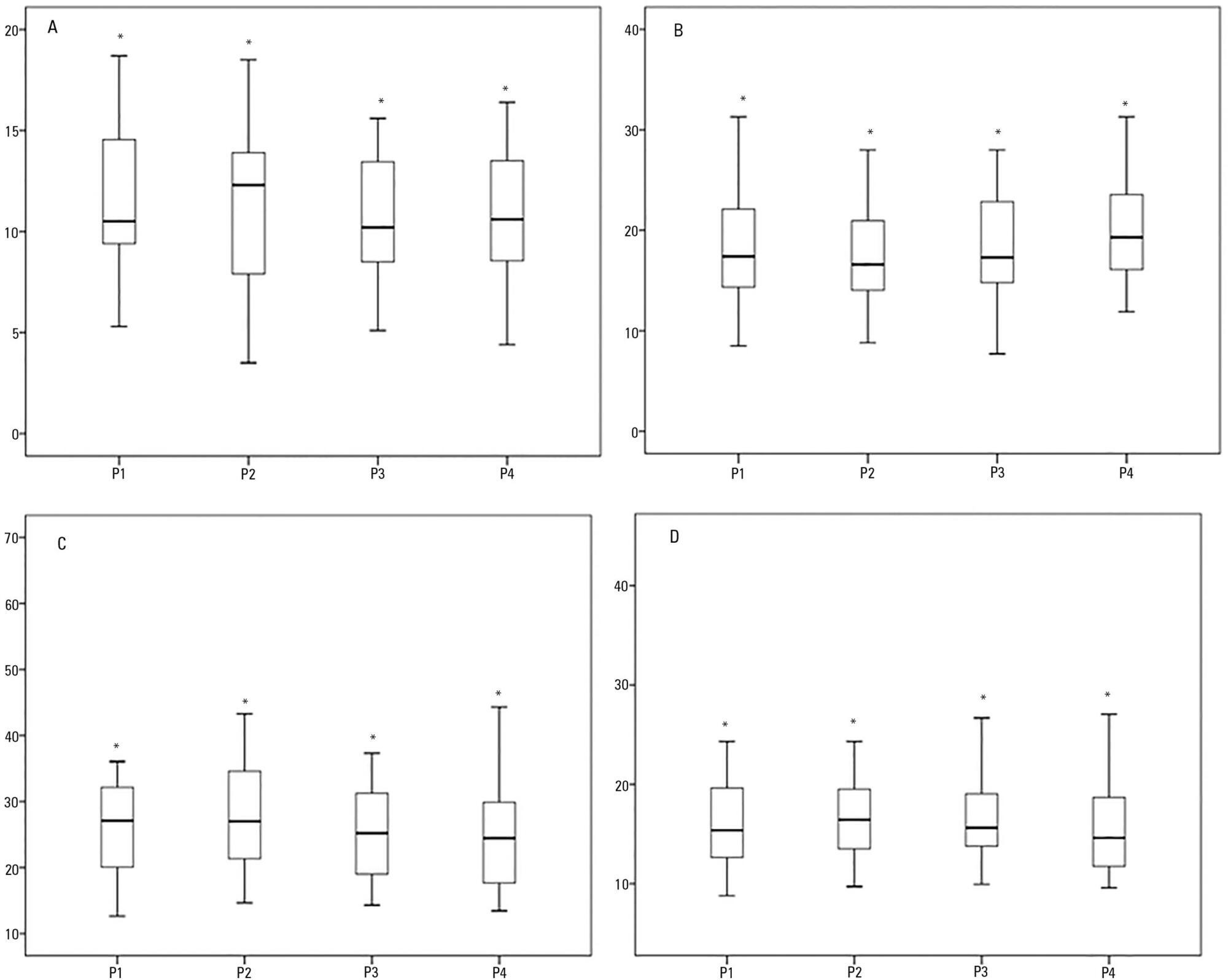
This was a prospective physiological study in which static and dynamic compliance, resistive airway pressure, and peripheral oxygen saturation were measured with the head at four different positions (0° = P1, 30° = P2, 45° = P3, and 60° = P4). Repeated-measures analysis of variance (ANOVA) with a Bonferroni post-test and Friedman analysis were used to compare the values obtained at the different positions.
A comparison of the 35 evaluated patients revealed that the resistive airway pressure values in the 0° position were higher than those obtained when patients were positioned at greater angles. The elastic pressure analysis revealed that the 60° position produced the highest value relative to the other positions. Regarding static compliance, a reduction in values was observed from the 0° position to the 60° position. The dynamic compliance analysis revealed that the 30° angle produced the greatest value compared to the other positions. The peripheral oxygen saturation showed little variation, with the highest value obtained at the 0° position.
The highest dynamic compliance value was observed at the 30° position, and the highest oxygenation value was observed at the 0° position.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):65-70
DOI 10.5935/0103-507X.20140010
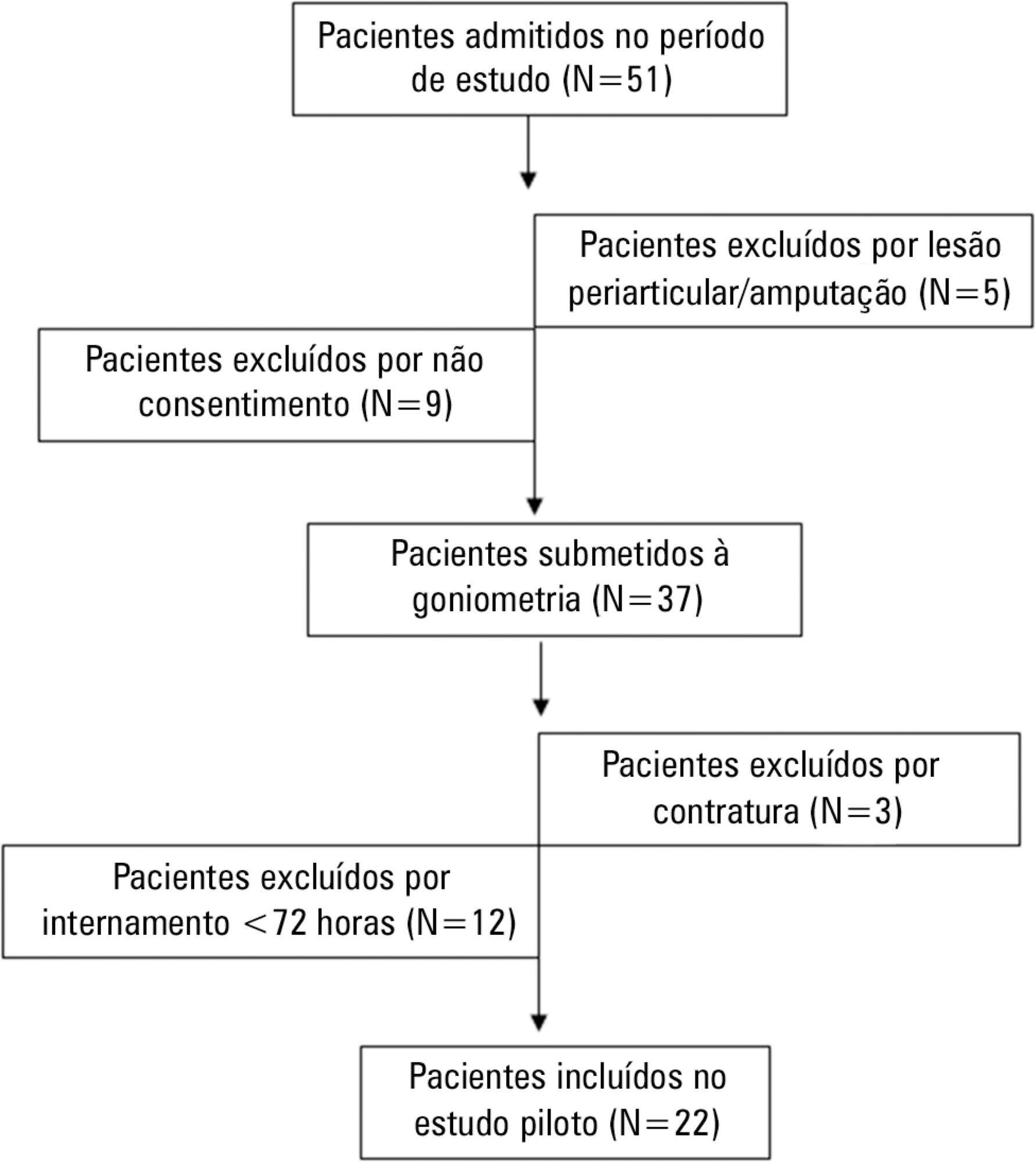
To evaluate the joint range of motion of critically ill patients during hospitalization in the intensive care unit.
This work was a prospective longitudinal study conducted in a critical care unit of a public hospital in the city of Salvador (BA) from September to November 2010. The main variable evaluated was the passive joint range of motion. A goniometer was used to measure the elbows, knees and ankles at the time of admission and at discharge. All patients admitted in the period were included other than patients with length of stay <72 hours and patients with reduced joint range of motion on admission.
The sample consisted of 22 subjects with a mean age of 53.5±17.6 years, duration of stay in the intensive care unit of 13.0±6.0 days and time on mechanical ventilation of 12.0±6.3 days. The APACHE II score was 28.5±7.3, and the majority of patients had functional independence at admission with a prior Barthel index of 88.8±19. The losses of joint range of motion were 11.1±2.1°, 11.0±2.2°, 8.4±1.7°, 9.2±1.6°, 5.8±0.9° and 5.1±1.0°, for the right and left elbows, knees and ankles, respectively (p<0.001).
There was a tendency towards decreased range of motion of large joints such as the ankle, knee and elbow during hospitalization in the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):99-105
DOI 10.5935/0103-507X.20130020
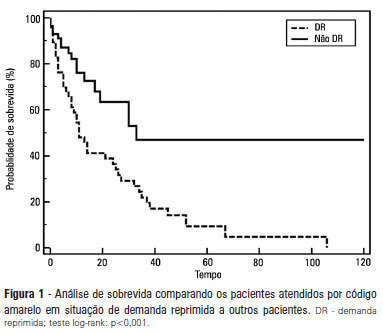
OBJECTIVE: To describe the epidemiological data of the clinical instability events in patients attended to by the rapid response team and to identify prognostic factors. METHODS: This was a longitudinal study, performed from January to July 2010, with an adult inpatient population in a hospital environment. The data collected regarding the code yellow service included the criteria of the clinical instability, the drug and non-drug therapies administered and the activities and procedures performed. The outcomes evaluated were the need for intensive care unit admission and the hospital mortality rates. A level of p=0.05 was considered to be significant. RESULTS: A total of 150 code yellow events that occurred in 104 patients were evaluated. The most common causes were related to acute respiratory insufficiency with hypoxia or a change in the respiratory rate and a concern of the team about the patient's clinical condition. It was necessary to request a transfer to the intensive care unit in 80 of the 150 cases (53.3%). It was necessary to perform 42 procedures. The most frequent procedures were orotracheal intubation and the insertion of a central venous catheter. The patients who were in critical condition and had to wait for an intensive care unit bed had a higher risk of death compared to the other patients (hazard ratio: 3.12; 95% CI: 1.80-5.40; p<0.001). CONCLUSIONS: There are patients in critical condition that require expert intensive care in the regular ward unit hospital beds. The events that most frequently led to the code yellow activation were related to hemodynamic and respiratory support. The interventions performed indicate the need for a physician on the team. The situation of pent-up demand is associated with a higher mortality rate.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)