Abstract
Rev Bras Ter Intensiva. 2014;26(1):65-70
DOI 10.5935/0103-507X.20140010
To evaluate the joint range of motion of critically ill patients during hospitalization in the intensive care unit.
This work was a prospective longitudinal study conducted in a critical care unit of a public hospital in the city of Salvador (BA) from September to November 2010. The main variable evaluated was the passive joint range of motion. A goniometer was used to measure the elbows, knees and ankles at the time of admission and at discharge. All patients admitted in the period were included other than patients with length of stay <72 hours and patients with reduced joint range of motion on admission.
The sample consisted of 22 subjects with a mean age of 53.5±17.6 years, duration of stay in the intensive care unit of 13.0±6.0 days and time on mechanical ventilation of 12.0±6.3 days. The APACHE II score was 28.5±7.3, and the majority of patients had functional independence at admission with a prior Barthel index of 88.8±19. The losses of joint range of motion were 11.1±2.1°, 11.0±2.2°, 8.4±1.7°, 9.2±1.6°, 5.8±0.9° and 5.1±1.0°, for the right and left elbows, knees and ankles, respectively (p<0.001).
There was a tendency towards decreased range of motion of large joints such as the ankle, knee and elbow during hospitalization in the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2010;22(4):315-320
DOI 10.1590/S0103-507X2010000400001
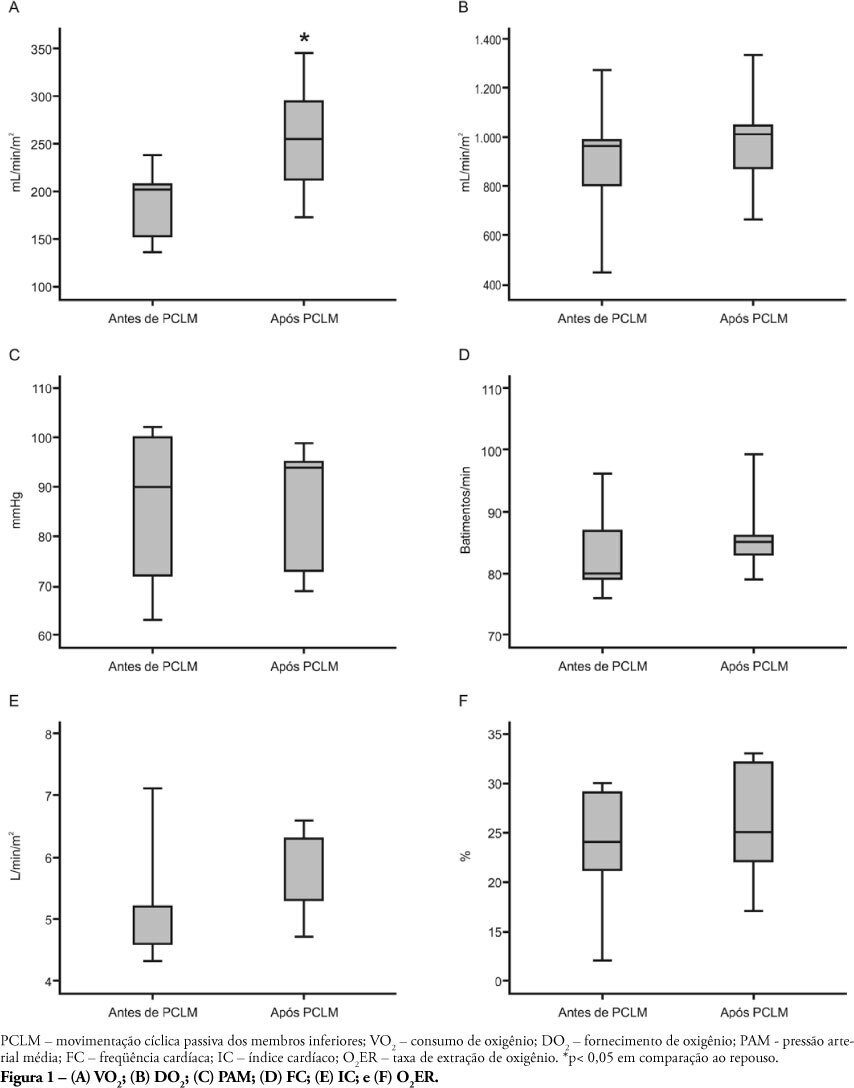
OBJECTIVE: Limb movements, passively performed by a physiotherapist, have been shown to result in significant increases in critically ill patients' metabolic and hemodynamic variables. This study objective was to determine whether passive cycling leg movement increases hemodynamic and metabolic variables in sedated mechanical ventilation dependent patients. METHODS: Five sedated mechanical ventilation dependent patients in a 18-bed intensive care unit of a university hospital were evaluated. Passive cycling leg movements were performed for 10min at a 30 movements/min rate. Complete hemodynamical data were recorded and arterial and mixed venous blood sample were collected 5 minutes before and after 5 minutes after the maneuver completion. RESULTS: All patients had increased oxygen consumption (VO2). The VO2 increase occurred with a concomitant drop in mixed venous blood saturation (SvO2), likely from both oxygen extraction ratio (O2ER) and cardiac index (CI) increase. CONCLUSION: passive cycling leg movements may influence hemodynamical and metabolic status in sedated mechanical ventilation-dependent patients.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)