Abstract
Crit Care Sci. 2023;35(2):117-146
DOI 10.5935/2965-2774.20230310-pt
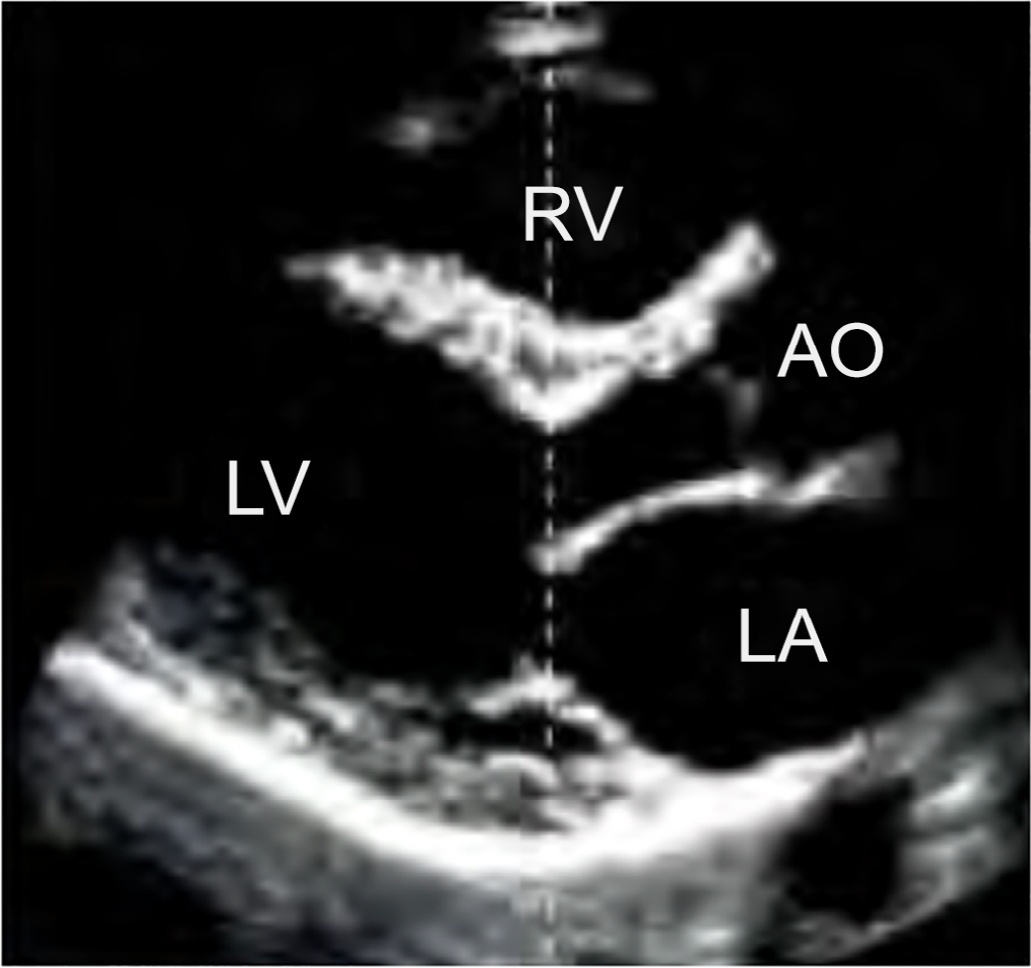
Echocardiography in critically ill patients has become essential in the evaluation of patients in different settings, such as the hospital. However, unlike for other matters related to the care of these patients, there are still no recommendations from national medical societies on the subject. The objective of this document was to organize and make available expert consensus opinions that may help to better incorporate echocardiography in the evaluation of critically ill patients. Thus, the Associação de Medicina Intensiva Brasileira, the Associação Brasileira de Medicina de Emergência, and the Sociedade Brasileira de Medicina Hospitalar formed a group of 17 physicians to formulate questions relevant to the topic and discuss the possibility of consensus for each of them. All questions were prepared using a five-point Likert scale. Consensus was defined a priori as at least 80% of the responses between one and two or between four and five. The consideration of the issues involved two rounds of voting and debate among all participants. The 27 questions prepared make up the present document and are divided into 4 major assessment areas: left ventricular function, right ventricular function, diagnosis of shock, and hemodynamics. At the end of the process, there were 17 positive (agreement) and 3 negative (disagreement) consensuses; another 7 questions remained without consensus. Although areas of uncertainty persist, this document brings together consensus opinions on several issues related to echocardiography in critically ill patients and may enhance its development in the national scenario.
Abstract
Crit Care Sci. 2023;35(1):73-83
DOI 10.5935/2965-2774.20230374-pt
To understand the perception of medical communication and needs of family members with loved ones in intensive care.
The study was mainly qualitative and exploratory, with thematic analysis of comments made by 92 family members with loved ones in intensive care units when answering in-person interviews comprising the Quality of Communication Questionnaire (QoC) and open-ended questions about their need for additional help, the appropriateness of the place where they received information, and additional comments.
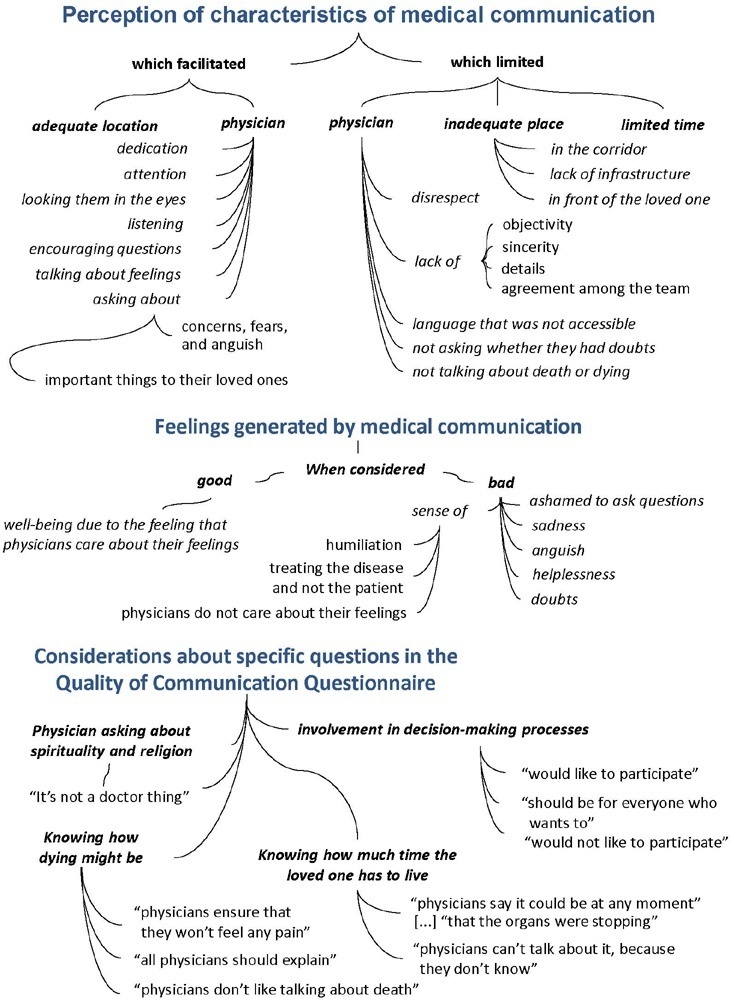
The participants’ mean age was 46.8 years (SD = 11.8), and most of them were female, married and had incomplete or completed elementary education. The following themes were found: perception of characteristics of medical communication; feelings generated by communication; considerations about specific questions in the QoC; family members’ needs; and strategies to overcome needs regarding communication. Characteristics that facilitated communication included attention and listening. Characteristics that made communication difficult included aspects of information sharing, such as inaccessible language; lack of clarity, objectivity, sincerity, and agreement among the team; limited time; and inadequate location. Feelings such as shame, helplessness, and sadness were cited when communication was inadequate. Family members’ needs related to communication included more details about the loved one’s diagnosis, prognosis, and health condition; participation in decisionmaking; and being asked about feelings, spirituality, dying and death. Others were related to longer visitation time, psychological support, social assistance, and better infrastructure.
It is necessary to enhance medical communication and improve hospital infrastructure to improve the quality of care for family members.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):426-432
DOI 10.5935/0103-507X.20220278-en
To characterize the knowledge and perceived attitudes toward pharmacologic interventions for light sedation in mechanically ventilated patients and to understand the current gaps comparing current practice with the recommendations of the Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the Intensive Care Unit.
This was a cross-sectional cohort study based on the application of an electronic questionnaire focused on sedation practices.
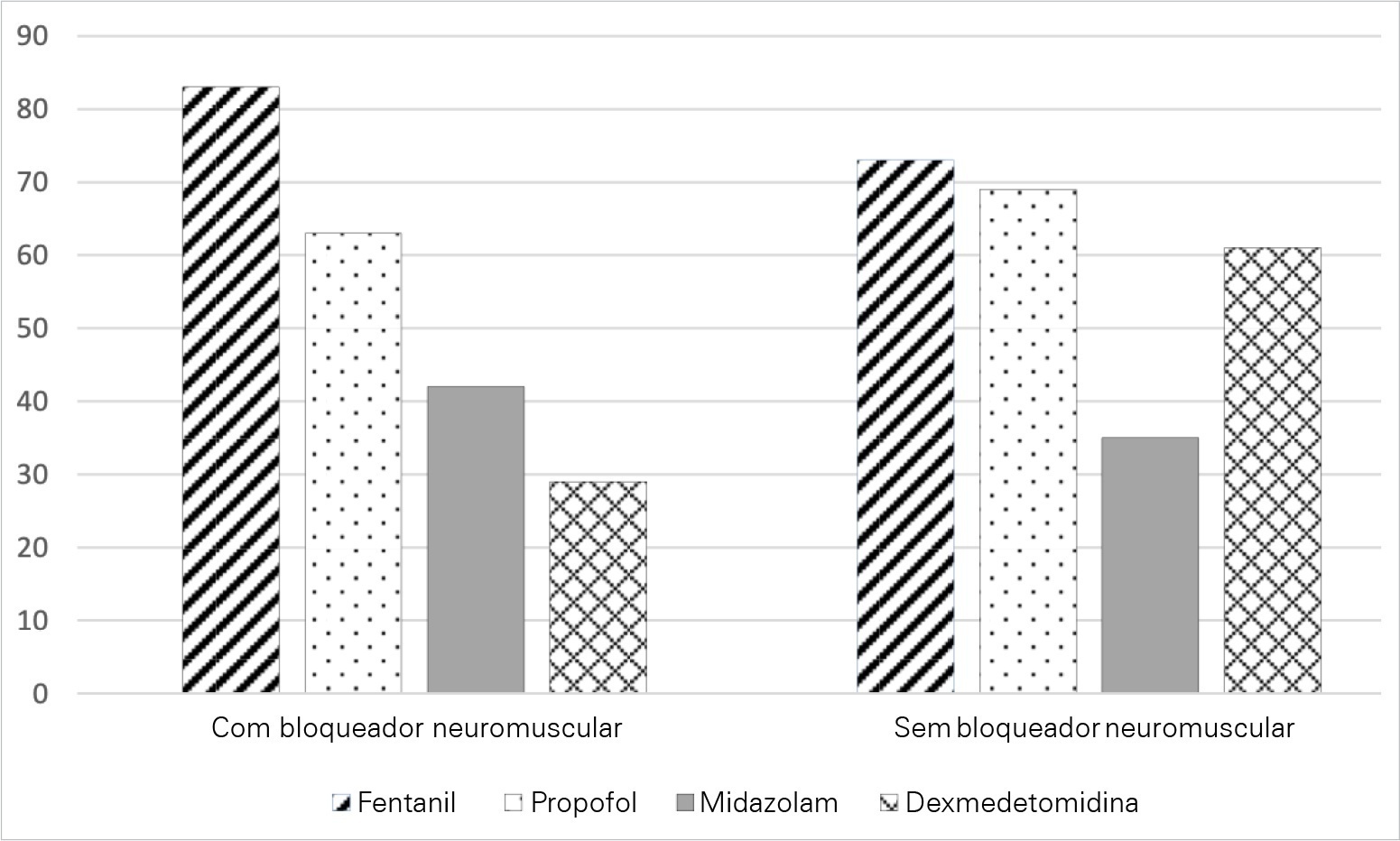
A total of 303 critical care physicians provided responses to the survey. Most respondents reported routine use of a structured sedation scale (281; 92.6%). Almost half of the respondents reported performing daily interruptions of sedation (147; 48.4%), and the same percentage of participants (48.0%) agreed that patients are often over sedated. During the COVID-19 pandemic, participants reported that patients had a higher chance of receiving midazolam compared to before the pandemic (178; 58.8% versus 106; 34.0%; p = 0.05), and heavy sedation was more common during the COVID-19 pandemic (241; 79.4% versus 148; 49.0%; p = 0.01).
This survey provides valuable data on the perceived attitudes of Brazilian intensive care physicians regarding sedation. Although daily interruption of sedation was a well-known concept and sedation scales were often used by the respondents, insufficient effort was put into frequent monitoring, use of protocols and systematic implementation of sedation strategies. Despite the perception of the benefits linked with light sedation, there is a need to identify improvement targets to propose educational strategies to improve current practices.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):484-491
DOI 10.5935/0103-507X.20220264-en
To obtain data on bed refusal in intensive care units in Brazil and to evaluate the use of triage systems by professionals.
A cross-sectional survey. Using the Delphi methodology, a questionnaire was created contemplating the objectives of the study. Physicians and nurses enrolled in the research network of the Associação de Medicina Intensiva Brasileira (AMIBnet) were invited to participate. A web platform (SurveyMonkey®) was used to distribute the questionnaire. The variables in this study were measured in categories and expressed as proportions. The chi-square test or Fisher’s exact test was used to verify associations. The significance level was set at 5%.
In total, 231 professionals answered the questionnaire, representing all regions of the country. The national intensive care units had an occupancy rate of more than 90% always or frequently for 90.8% of the participants. Among the participants, 84.4% had already refused admitting patients to the intensive care unit due to the capacity of the unit. Half of the Brazilian institutions (49.7%) did not have triage protocols for admission to intensive beds.
Bed refusal due to high occupancy rates is common in Brazilian intensive care units. Even so, half of the services in Brazil do not adopt protocols for triage of beds.
Abstract
Rev Bras Ter Intensiva. 2022;34(2):272-278
DOI 10.5935/0103-507X.20220025-en
To translate, crossculturally adapt and evaluate the clinimetric properties of the Critical Care Functional Rehabilitation Outcome Measure for evaluating the functionality of patients admitted to intensive care units in Brazil.
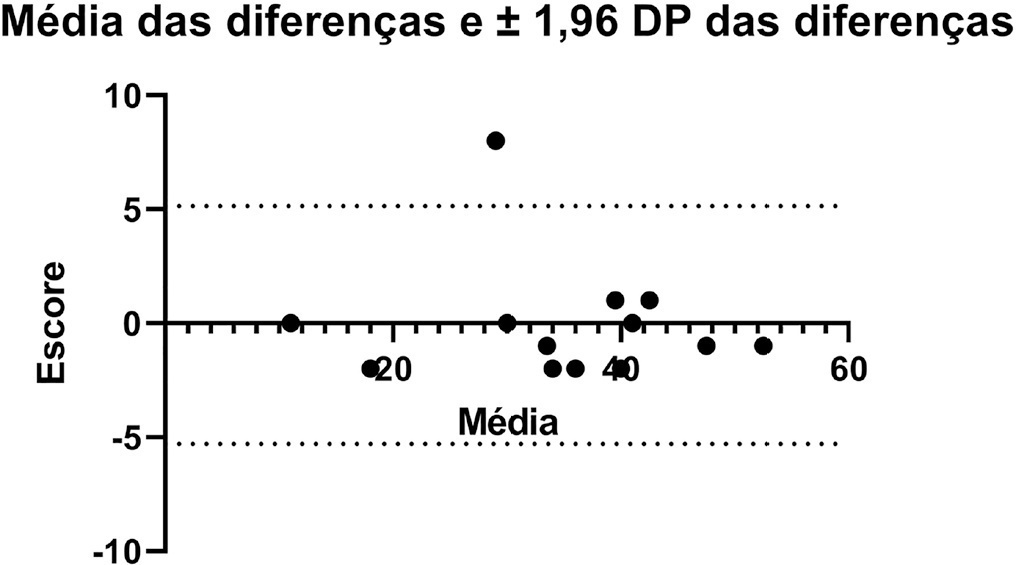
The process of translation and cross-cultural adaptation involved the following steps: initial translation, synthesis, back-translation, expert committee review and pretesting. The intra- and interrater reliability and agreement were analyzed between two physical therapists who evaluated the same group of patients (n = 35). The evaluations were performed by each therapist independently and blinded to the score assigned by the other professional. The qualitative analysis was performed by the review committee, and the experts adapted and synthesized the Portuguese translation of the Critical Care Functional Rehabilitation Outcome Measure.
There was agreement between the initial Brazilian translations of the Critical Care Functional Rehabilitation Outcome Measure scale. The conceptual, idiomatic, semantic and experimental equivalences between the original and translated versions were assessed, resulting in the final Brazilian version of the scale, called the Medida de Resultado da Reabilitação Funcional em Cuidados Intensivos. The evaluation of the clinimetric properties showed evidence of a high degree of agreement and reliability, as all had an intraclass correlation coefficient above 0.75. The overall intraclass correlation coefficient was 0.89.
The translated version of the Critical Care Functional Rehabilitation Outcome Measure scale for assessing the functionality of patients admitted to an intensive care unit can be used reliably in Brazil following translation and cross-cultural adaptation to Brazilian Portuguese and presents evidence of excellent interrater reliability.
Abstract
Rev Bras Ter Intensiva. 2022;34(1):107-115
DOI 10.5935/0103-507X.20220005-en
To evaluate clinical practices and hospital resource organization during the early COVID-19 pandemic in Brazil.
This was a multicenter, cross-sectional survey. An electronic questionnaire was provided to emergency department and intensive care unit physicians attending COVID-19 patients. The survey comprised four domains: characteristics of the participants, clinical practices, COVID-19 treatment protocols and hospital resource organization.
Between May and June 2020, 284 participants [median (interquartile ranges) age 39 (33 - 47) years, 56.3% men] responded to the survey; 33% were intensivists, and 9% were emergency medicine specialists. Half of the respondents worked in public hospitals. Noninvasive ventilation (89% versus 73%; p = 0.001) and highflow nasal cannula (49% versus 32%; p = 0.005) were reported to be more commonly available in private hospitals than in public hospitals. Mechanical ventilation was more commonly used in public hospitals than private hospitals (70% versus 50%; p = 0,024). In the Emergency Departments, positive endexpiratory pressure was most commonly adjusted according to SpO2, while in the intensive care units, positive end-expiratory pressure was adjusted according to the best lung compliance. In the Emergency Departments, 25% of the respondents did not know how to set positive end-expiratory pressure. Compared to private hospitals, public hospitals had a lower availability of protocols for personal protection equipment during tracheal intubation (82% versus 94%; p = 0.005), managing mechanical ventilation [64% versus 75%; p = 0.006] and weaning patients from mechanical ventilation [34% versus 54%; p = 0.002]. Finally, patients spent less time in the emergency department before being transferred to the intensive care unit in private hospitals than in public hospitals [2 (1 - 3) versus 5 (2 - 24) hours; p < 0.001].
This survey revealed significant heterogeneity in the organization of hospital resources, clinical practices and treatments among physicians during the early COVID-19 pandemic in Brazil.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):592-599
DOI 10.5935/0103-507X.20210086
To translate and culturally adapt the Pediatric Intensive Care Unit-Quality of Dying and Death questionnaire into Brazilian Portuguese.
This was a cross-cultural adaptation process including conceptual, cultural, and semantic equivalence steps comprising three stages. Stage 1 involved authorization to perform the translation and cultural adaptation. Stage 2 entailed independent translation from English into Brazilian Portuguese, a synthesis of the translation, back-translation, and an expert panel. Stage 3 involved a pretest conducted with family caregivers and a multidisciplinary team.
The evaluation by the expert panel resulted in an average agreement of 0.8 in relation to semantic, cultural, and conceptual equivalence. The pretests of both versions of the questionnaire showed that the participants had adequate comprehension regarding the ease of understanding the items and response options.
After going through the process of translation and cultural adaptation, the Pediatric Intensive Care Unit-Quality of Dying and Death caregiver and multidisciplinary team versions were considered culturally adapted, with both groups having a good understanding of the items. The questionnaires include relevant items to evaluate the process of death and dying in the intensive care setting, and suggest changes in care centered on patients and especially family caregivers, given the finitude of their children.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)