Abstract
Crit Care Sci. 2023;35(1):73-83
DOI 10.5935/2965-2774.20230374-pt
To understand the perception of medical communication and needs of family members with loved ones in intensive care.
The study was mainly qualitative and exploratory, with thematic analysis of comments made by 92 family members with loved ones in intensive care units when answering in-person interviews comprising the Quality of Communication Questionnaire (QoC) and open-ended questions about their need for additional help, the appropriateness of the place where they received information, and additional comments.
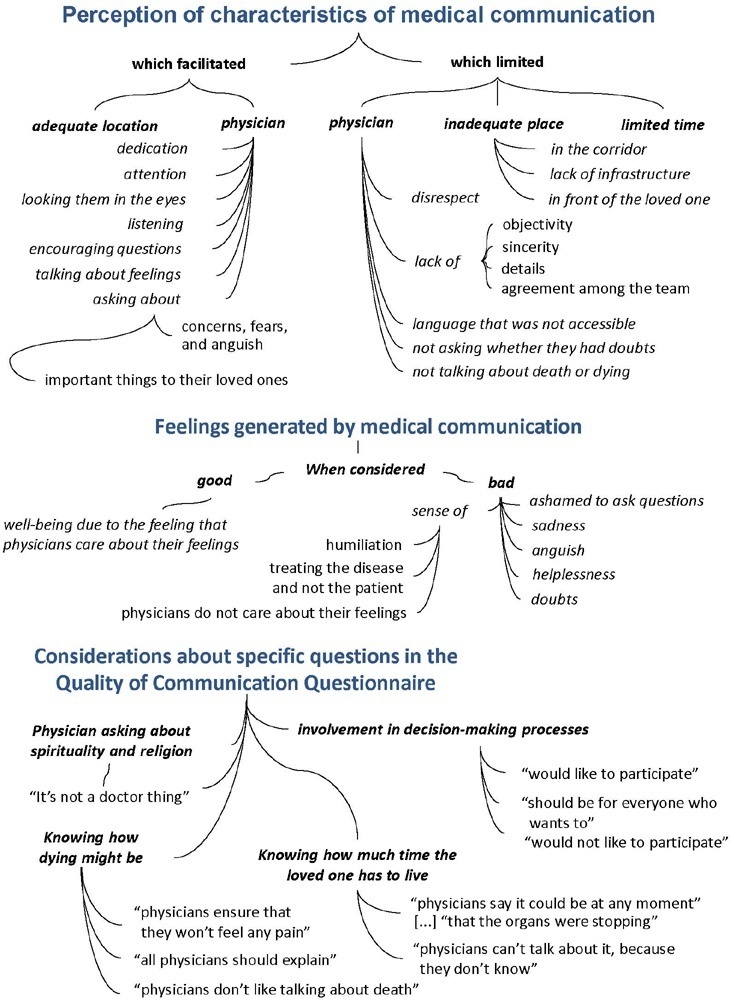
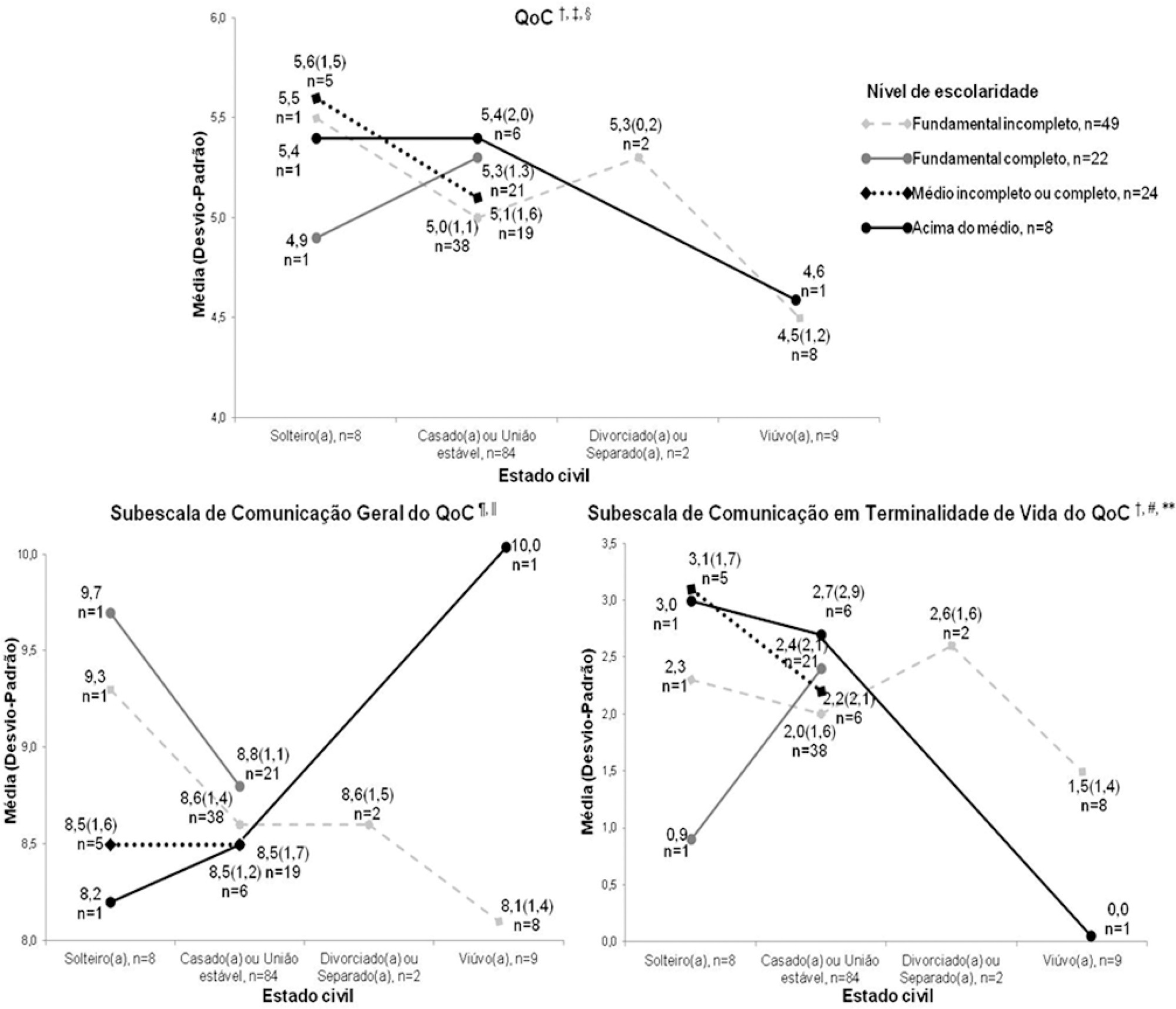
The participants’ mean age was 46.8 years (SD = 11.8), and most of them were female, married and had incomplete or completed elementary education. The following themes were found: perception of characteristics of medical communication; feelings generated by communication; considerations about specific questions in the QoC; family members’ needs; and strategies to overcome needs regarding communication. Characteristics that facilitated communication included attention and listening. Characteristics that made communication difficult included aspects of information sharing, such as inaccessible language; lack of clarity, objectivity, sincerity, and agreement among the team; limited time; and inadequate location. Feelings such as shame, helplessness, and sadness were cited when communication was inadequate. Family members’ needs related to communication included more details about the loved one’s diagnosis, prognosis, and health condition; participation in decisionmaking; and being asked about feelings, spirituality, dying and death. Others were related to longer visitation time, psychological support, social assistance, and better infrastructure.
It is necessary to enhance medical communication and improve hospital infrastructure to improve the quality of care for family members.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):386-392
DOI 10.5935/0103-507X.20220446-en
To analyze the association of patient safety culture perceived by nursing professionals with incidents recorded during nursing shifts in intensive care units.
This was a cross-sectional study that investigated patient safety culture measured by the Hospital Survey on Patient Safety Culture instrument. Descriptive statistics, chi-square tests, Student’s t-test and multiple linear regression models were analyzed considering a significance level of 5%.
The study reported a mean of 3.1 (standard deviation of 0.4) for the culture of patient safety in the perception of nursing professionals and 480 incidents with and without damage recorded during the nursing shifts. The variables patient safety culture with a difference between means of 0.543 (95%CI 0.022 - 1.065; p < 0.05) and nursing assistants with a difference between means of -0.133 (95%CI -0.192 - -0.074; p < 0.05) were associated with the incidents recorded during the nursing shifts. Further, nursing assistants had a lower tendency to record incidents than did the nurses.
The strengthening of the patient safety culture and the aspects tangential to the nursing professionals represent a possible target for interventions to encourage the recording of incidents during the nursing shift shifts and improve patient safety.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):401-411
DOI 10.5935/0103-507X.20210050
To understand the perception of patients about medical communication as well as their needs during hospitalization in the intensive care unit.
This study was cross-sectional descriptive and qualitative exploratory including 103 patients admitted to or recently discharged from the intensive care units of four hospitals in Greater Florianópolis, Santa Catarina state, Brazil. The patients’ sociodemographic and clinical variables were studied, as were the score they gave to the quality of medical communication through the Quality of Communication Questionnaire and their spontaneous comments with reflections or justifications for the scores given, and their responses on how they felt and what complementary help they would have liked to receive. The quantitative data were analyzed by descriptive and analytical statistics, and the qualitative data were analyzed by thematic content analysis.
The mean Quality of Communication Questionnaire score was 5.1 (standard deviation - SD = 1.3), with 8.6 (SD = 1.3) on the general communication subscale and 2.1 (SD = 1.8) on the end-of-life communication subscale. The patients had a variable understanding of medical language. Some physicians seemed to be “rushed”, according to some patients. Other patients would like to receive more frequent and detailed information and/or be respected and taken “more seriously” when they reported pain. Anxiety, sadness, and fear were among the reported feelings. Other needs included silence, more time for visits, the presence of a companion, psychological and social-work care, a bathroom that they could use, and better food in the intensive care unit.
The quality of medical communication with patients is good but could improve if physicians and the healthcare team had more time for patients. Other felt needs included respect, pain relief, and adjustments in the intensive care unit dynamics and environment.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):448-454
DOI 10.1590/S0103-507X2011000400009
OBJECTIVES: This study aimed to assess family member acceptance of orthotanasia as related to symptom management, patient preference and the influence of the medical team's communication on therapy. METHODS: This was a descriptive one-year study conducted at the adult intensive care unit of the Hospital do Servidor Público Estadual. A structured questionnaire based on the Quality of Dying and Death (QODD 22) instrument and prior informal interviews were used. RESULTS: Sixty family members were assessed; the mean age was 51.7 + 12.1 years, and 81.7% were female. The patients were hospitalized for a mean of 31 + 26.9 days, and 17.0% of these days were spent in the intensive care unit. Most of the patients had neurological conditions. Most of the patients (53.3%) had discussed their end-of-life care wishes with family members; however, 76.7% of them had not discussed this issue with their doctors (p < 0.00). The family members reported being favorable to orthotanasia in 83.3% of the cases. Most (85.0%) desired the medical team to clearly approach the subject, and 65.0% wished to take part in the quality of end-of-life decision making process. The family members were generally satisfied with information they received from the doctors: 93.3% believed they had received appropriately frequent communications about the clinical conditions; 81.7% were able to clarify their doubts regarding the patient's clinical status; the communication was understood by 83.3% of the respondents; and 80.0% believed that clear and honest information had been provided. Only 43.3% of the respondents wished to be present at the time of their loved ones' deaths. A significant association between family member acceptance of orthotanasia and participation in end-of-life decisions (p = 0.042) was observed. CONCLUSIONS: Most of the respondents were favorable to orthotanasia and wished to participate in end-of-life discussions.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):112-117
DOI 10.1590/S0103-507X2010000200003
OBJECTIVES: Communication issues between healthcare professionals in intensive care units may be related to critically ill patients’ increased mortality. This study aimed to evaluate if communication issues involving assistant physicians and routine intensive care unit physicians would impact critically ill patients’ morbidity and mortality. METHODS: This was a cohort study that included non-consecutive patients admitted to the intensive care unit for 18 months. The patients were categorized in 3 groups according to their assistant doctors’ versus routine doctors communication uses: DC - daily communication during the stay (>75% of the days); EC - eventual communication (25 to 75% of the days); RC - rare communication (< 25% of the days). Demographic data, severity scores, reason for admission to the intensive care unit and interventions were recorded. The consequences of the medical professionals communication failures (delayed procedures, diagnostic tests, antibiotics, ventilatory weaning, vasopressors) and medical prescriptions inadequacies (no bed head elevation, no stress ulceration and deep venous thrombosis drug prophylaxis), and their relationship with the patients outcomes were analyzed. RESULTS: 792 patients were included, and categorized as follows: DC (n=529); EC (n=187) and RC (n=76). The mortality was increased in the RC patients group (26.3%) versus the remainder groups (DC = 13.6% and EC = 17.1%; p<0.05). A multivariate analysis showed that delayed antibiotics [RR 1.83 (CI95%: 1.36 -2.25)], delayed ventilatory weaning [RR 1.63 (CI95%: 1.25-2.04)] and no deep venous thrombosis prophylaxis [RR 1.98 (CI95%: 1.43 - 3.12)] contributed independently for the increased mortality. CONCLUSION: The failure in the assistant and routine intensive care doctors communication may increase the patients’ mortality, particularly due to delayed antibiotics and ventilation weaning, and lack of deep venous thrombosis prophylaxis prescription.
Abstract
Rev Bras Ter Intensiva. 2007;19(4):485-489
DOI 10.1590/S0103-507X2007000400014
BACKGROUND AND OBJECTIVES: The suffering with the death and the prolonged time of patient's admission in a intensive care unit (ICU) are factors that leads to necessity the best communication with the personal that works in ICU, patients and their family, and its justify this work, whose objective is discuss this subject. CONTENTS: The professional experience of the author was used in this issue and the articles written during the last five years about death, communication and ICU were reviewed by means of MedLine, Up to Date, Google and Brazilian Journal of Intensive Therapy. CONCLUSIONS: It was concluded that the physician, the patient together with her/his family, and the multiprofessional staff of the ICU is one of the main factors that interferes with the process of satisfying both the patient and the ones who work on such unities. For adequate information, the physician must be conscious about therapeutic limits, and must learn how to treat the patient during the process of dying. In this way, the physician will be apt to talk about death. The ideal situation would be that the professional, responsible to give the news, should be experience, from the technical point of view as well as ethical, and should be the same person, as always as possible, when necessary. The patient mostly little be able to influence in her/his process of dying, but if communication is possible, it be simple, honest and humane. The patient's family members have the right of being together with the one who they love, and of being steadily informed about the real situation. All the members in the process must know the truth and the chosen therapeutic orientation to be taken. Communication should be done in a quiet and prived place.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)