Abstract
Crit Care Sci. 2023;35(3):302-310
DOI 10.5935/2965-2774.20230141-pt
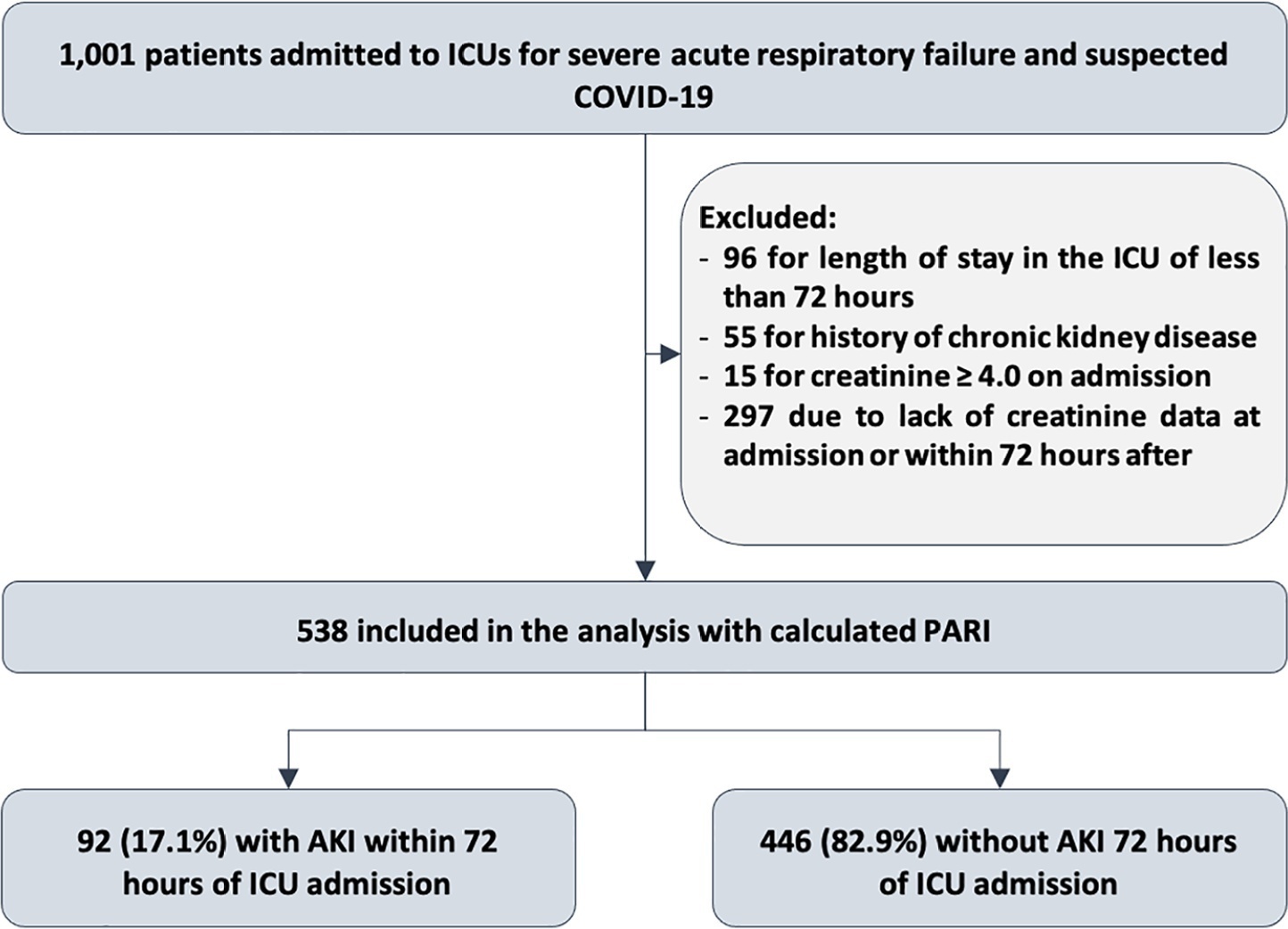
To evaluate the accuracy of the persistent AKI risk index (PARI) in predicting acute kidney injury within 72 hours after admission to the intensive care unit, persistent acute kidney injury, renal replacement therapy, and death within 7 days in patients hospitalized due to acute respiratory failure.
This study was done in a cohort of diagnoses of consecutive adult patients admitted to the intensive care unit of eight hospitals in Curitiba, Brazil, between March and September 2020 due to acute respiratory failure secondary to suspected COVID-19. The COVID-19 diagnosis was confirmed or refuted by RT-PCR for the detection of SARS-CoV-2. The ability of PARI to predict acute kidney injury at 72 hours, persistent acute kidney injury, renal replacement therapy, and death within 7 days was analyzed by ROC curves in comparison to delta creatinine, SOFA, and APACHE II.
Of the 1,001 patients in the cohort, 538 were included in the analysis. The mean age was 62 ± 17 years, 54.8% were men, and the median APACHE II score was 12. At admission, the median SOFA score was 3, and 83.3% had no renal dysfunction. After admission to the intensive care unit, 17.1% had acute kidney injury within 72 hours, and through 7 days, 19.5% had persistent acute kidney injury, 5% underwent renal replacement therapy, and 17.1% died. The PARI had an area under the ROC curve of 0.75 (0.696 - 0.807) for the prediction of acute kidney injury at 72 hours, 0.71 (0.613 - 0.807) for renal replacement therapy, and 0.64 (0.565 - 0.710) for death.
The PARI has acceptable accuracy in predicting acute kidney injury within 72 hours and renal replacement therapy within 7 days of admission to the intensive care unit, but it is not significantly better than the other scores.
Abstract
Rev Bras Ter Intensiva. 2021;33(1):172-175
DOI 10.5935/0103-507X.20210019
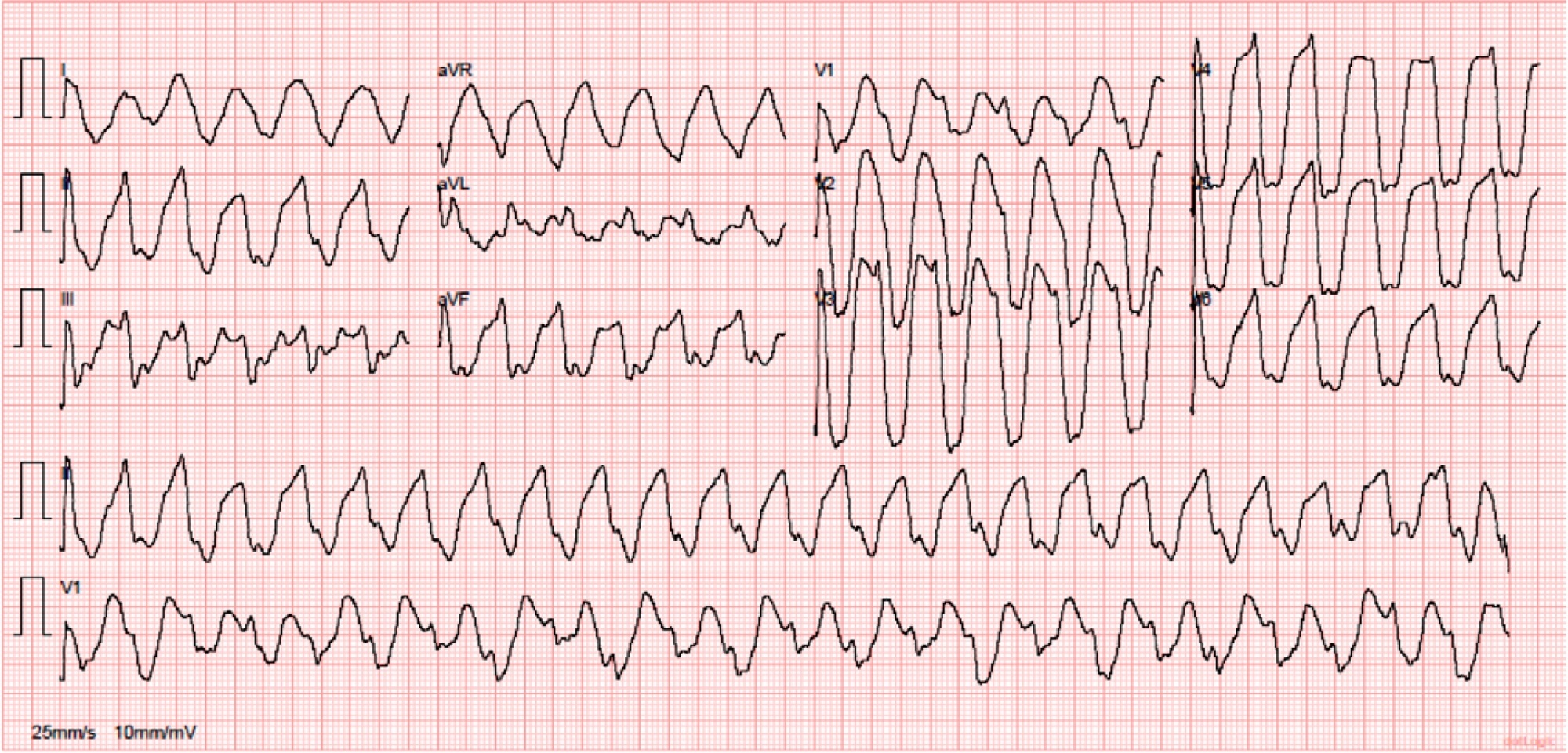
European yew (Taxus baccata) is a tree with alternate branchlets, green needles and reddish-brown bark. A high-dose ingestion of Taxus baccata for suicidal purposes usually results in death. The systemic toxicity is mainly cardiac. The authors describe the case of a young patient who ingested a high dose of yew needles and presented to the emergency department with a serious intoxication, which manifested as a chaotic malignant arrhythmia that was successfully treated after exhaustive supportive care.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):439-443
DOI 10.5935/0103-507X.20200074
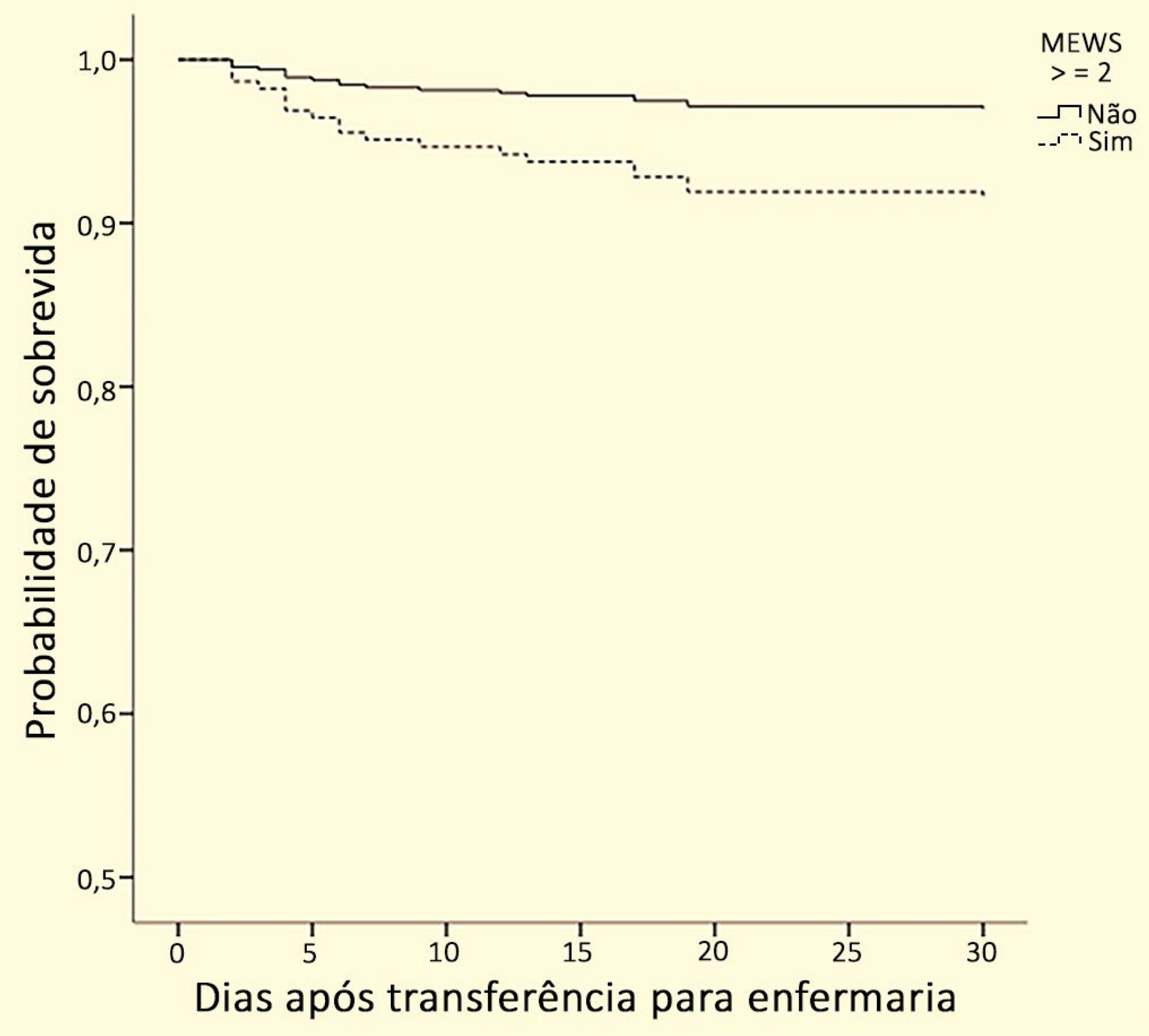
To verify whether there is an association between the Modified Early Warning Score before the transfer from the emergency room to the ward and death or admission to the intensive care unit within 30 days.
This is a historical cohort study conducted in a high-complexity hospital in southern Brazil with patients who were transferred from the emergency room to the ward between January and June 2017. The following data were collected: sociodemographic variables; comorbidities, as determined by the Charlson index; reason for hospitalization; Modified Early Warning Score at the time of transfer; admission to the intensive care unit; care by the Rapid Response Team; mortality within 30 days; and hospital mortality.
A total of 278 patients were included in the study. Regarding the Modified Early Warning Score, patients who died within 30 days had a significantly higher score than surviving patients during this period (2.0 [1.0 - 3.0] versus 1.0 [1.0 - 2.0], respectively; p = 0.006). The areas under the receiver operating characteristic curve for death within 30 days and for ICU admission were 0.67 (0.55 - 0.80; p = 0.012) and 0.72 (0.59 - 0.84; p = 0.02), respectively, with a Modified Early Warning Score cutoff of ≥ 2. In the Cox regression, the Modified Early Warning Score was independently associated with mortality within 30 days after multivariate adjustment (hazard ratio 2.91; 95% confidence interval 1.04 - 8.13).
The Modified Early Warning Score before intrahospital transfer from the emergency room to the ward is associated with admission to the intensive care unit and death within 30 days. The Modified Early Warning Score can be an important indicator for monitoring these patients and can prompt the receiving team to take specific actions.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):51-56
DOI 10.5935/0103-507X.20150009
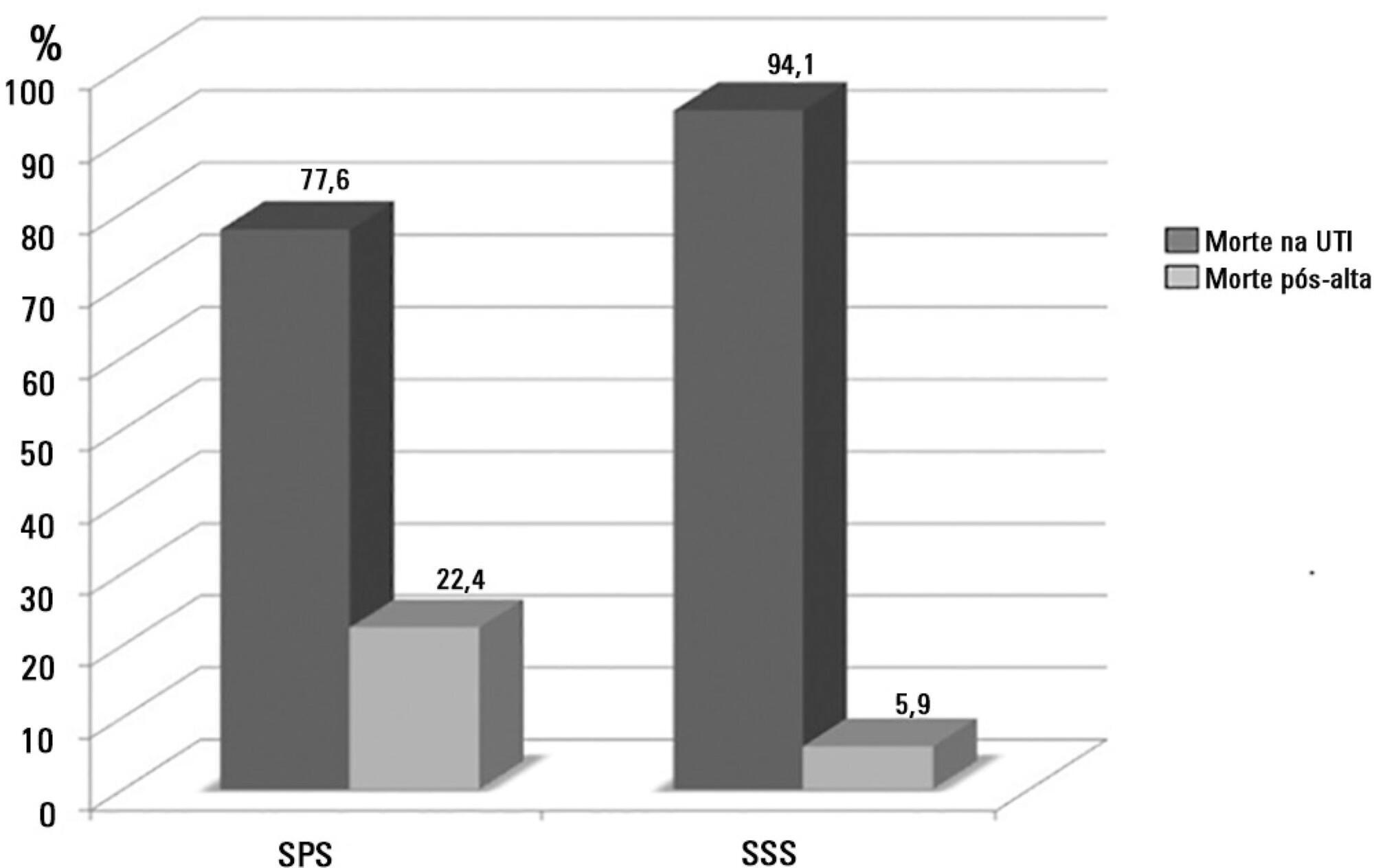
To assess the causes and factors associated with the death of patients between intensive care unit discharge and hospital discharge.
The present is a pilot, retrospective, observational cohort study. The records of all patients admitted to two units of a public/private university hospital from February 1, 2013 to April 30, 2013 were assessed. Demographic and clinical data, risk scores and outcomes were obtained from the Epimed monitoring system and confirmed in the electronic record system of the hospital. The relative risk and respective confidence intervals were calculated.
A total of 581 patients were evaluated. The mortality rate in the intensive care unit was 20.8% and in the hospital was 24.9%. Septic shock was the cause of death in 58.3% of patients who died after being discharged from the intensive care unit. Of the patients from the public health system, 73 (77.6%) died in the intensive care unit and 21 (22.4%) died in the hospital after being discharged from the unit. Of the patients from the Supplementary Health System, 48 (94.1%) died in the intensive care unit and 3 (5.9%) died in the hospital after being discharged from the unit (relative risk, 3.87%; 95% confidence interval, 1.21 - 12.36; p < 0.05). The post-discharge mortality rate was significantly higher in patients with intensive care unit hospitalization time longer than 6 days.
The main cause of death of patients who were discharged from the intensive care unit and died in the ward before hospital discharge was septic shock. Coverage by the public healthcare system and longer hospitalization time in the intensive care unit were factors associated with death after discharge from the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):297-305
DOI 10.5935/0103-507X.20130051
To describe a single center experience involving the administration of colistin to treat nosocomial infections caused by multidrug-resistant Gram-negative bacteria and identify factors associated with acute kidney injury and mortality.
This retrospective longitudinal study evaluates critically ill patients with infections caused by multidrug-resistant Gram-negative bacteria. All adult patients who required treatment with intravenous colistin (colistimethate sodium) from January to December 2008 were considered eligible for the study. Data include demographics, diagnosis, duration of treatment, presence of acute kidney injury and 30-day mortality.
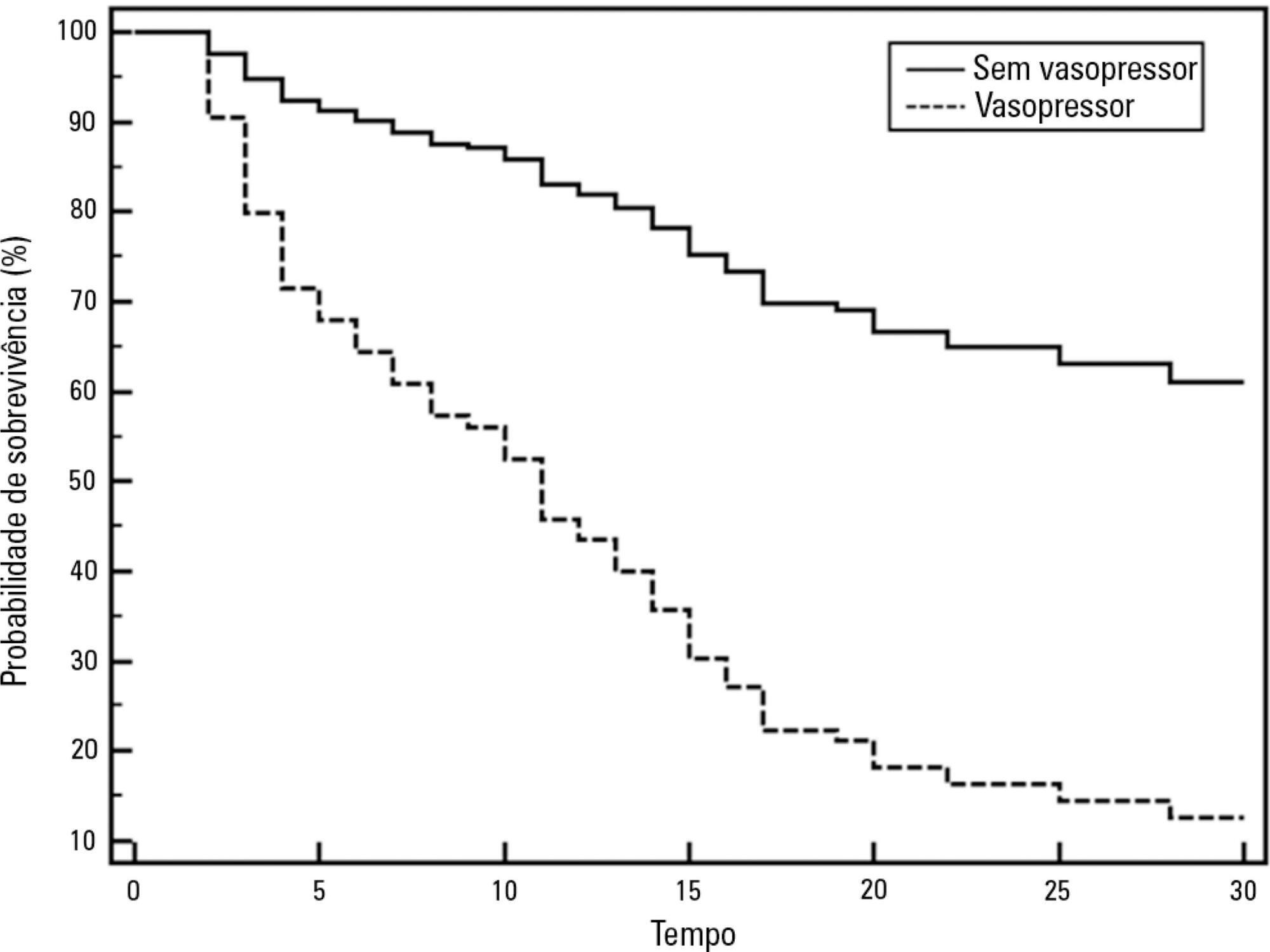
Colistin was used to treat an infection in 109 (13.8%) of the 789 patients admitted to the intensive care unit. The 30-day mortality observed in these patients was 71.6%. Twenty-nine patients (26.6%) presented kidney injury prior to colistin treatment, and six of these patients were able to recover kidney function even during colistin treatment. Twenty-one patients (19.2%) developed acute kidney injury while taking colistin, and 11 of these patients required dialysis. The variable independently associated with the presence of acute kidney injury was the Sequential Organ Failure Assessment at the beginning of colistin treatment (OR 1.46; 95%CI 1.20-1.79; p<0.001). The factors age (OR 1.03; 95%CI 1.00-1.05; p=0.02) and vasopressor use (OR 12.48; 95%CI 4.49-34.70; p<0.001) were associated with death in the logistic-regression model.
Organ dysfunction at the beginning of colistin treatment was associated with acute kidney injury. In a small group of patients, we were able to observe an improvement of kidney function during colistin treatment. Age and vasopressor use were associated with death.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):306-309
DOI 10.1590/S0103-507X2009000300011
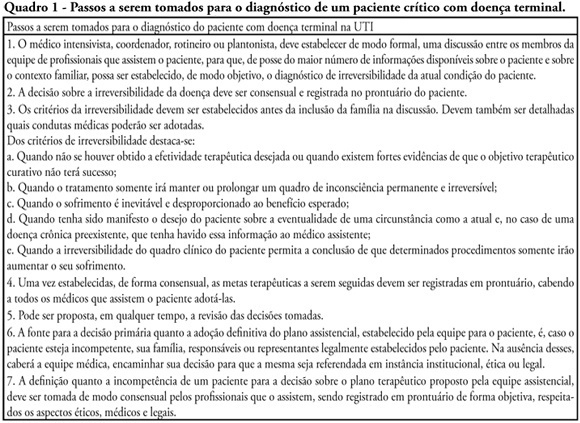
Withholding of treatment in patients with terminal disease is increasingly common in intensive care units, throughout the world. Notwithstanding, Brazilian intensivists still have a great difficulty to offer the best treatment to patients that have not benefited from curative care. The objective of this comment is to suggest an algorithm for the care of terminally ill patients. It was formulated based upon literature and the experience of experts, by members of the ethics committee and end-of-life of AMIB - Brazilian Association of Intensive Care.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):144-148
DOI 10.1590/S0103-507X2008000200005
BACKGROUND AND OBJECTIVES: Failure or delay to diagnose brain death leads to needless occupation of a hospital bed, emotional and financial losses, and unavailability of organs for transplants. The intensive care physician plays an essential role in this diagnosis. This study intended to evaluate intensivists' knowledge concerning brain death. METHODS: Cross-sectional study in 15 intensive care units (ICU) in eight hospitals in the city of Porto Alegre, Brazil. RESULTS: Two hundred forty-six intensivists were interviewed in a consecutive sample between April and December 2005. The prevalence of lack of knowledge regarding the concept was of 17%. Twenty per cent of the interviewees ignored the legal need for complementary confirmatory tests for their diagnosis. Forty-seven per cent considered themselves as having the highest level of assurance to explain the concept to a patient's family members. Twenty-nine per cent erroneously determined the legal time of death for brain dead patients. Pediatric intensivists had less knowledge about the concept, when compared to intensivists for adults (p < 0.001). CONCLUSIONS: Current knowledge of brain death is insufficient in Brazil, among the health care professionals who most often find patients in this situation. Education on the subject is needed to avoid unnecessary expenses, reduce family suffering and increase the offer of organs for transplant.
Abstract
Rev Bras Ter Intensiva. 2007;19(4):485-489
DOI 10.1590/S0103-507X2007000400014
BACKGROUND AND OBJECTIVES: The suffering with the death and the prolonged time of patient's admission in a intensive care unit (ICU) are factors that leads to necessity the best communication with the personal that works in ICU, patients and their family, and its justify this work, whose objective is discuss this subject. CONTENTS: The professional experience of the author was used in this issue and the articles written during the last five years about death, communication and ICU were reviewed by means of MedLine, Up to Date, Google and Brazilian Journal of Intensive Therapy. CONCLUSIONS: It was concluded that the physician, the patient together with her/his family, and the multiprofessional staff of the ICU is one of the main factors that interferes with the process of satisfying both the patient and the ones who work on such unities. For adequate information, the physician must be conscious about therapeutic limits, and must learn how to treat the patient during the process of dying. In this way, the physician will be apt to talk about death. The ideal situation would be that the professional, responsible to give the news, should be experience, from the technical point of view as well as ethical, and should be the same person, as always as possible, when necessary. The patient mostly little be able to influence in her/his process of dying, but if communication is possible, it be simple, honest and humane. The patient's family members have the right of being together with the one who they love, and of being steadily informed about the real situation. All the members in the process must know the truth and the chosen therapeutic orientation to be taken. Communication should be done in a quiet and prived place.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (115) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)