Abstract
Rev Bras Ter Intensiva. 2017;29(3):310-316
DOI 10.5935/0103-507X.20170039
To phenotypically evaluate biofilm production by Pseudomonas aeruginosa clinically isolated from patients with ventilator-associated pneumonia.
Twenty clinical isolates of P. aeruginosa were analyzed, 19 of which were from clinical samples of tracheal aspirate, and one was from a bronchoalveolar lavage sample. The evaluation of the capacity of P. aeruginosa to produce biofilm was verified using two techniques, one qualitative and the other quantitative.
The qualitative technique showed that only 15% of the isolates were considered biofilm producers, while the quantitative technique showed that 75% of the isolates were biofilm producers. The biofilm isolates presented the following susceptibility profile: 53.3% were multidrug-resistant, and 46.7% were multidrug-sensitive.
The quantitative technique was more effective than the qualitative technique for the detection of biofilm production. For the bacterial population analyzed, biofilm production was independent of the susceptibility profile of the bacteria, demonstrating that the therapeutic failure could be related to biofilm production, as it prevented the destruction of the bacteria present in this structure, causing complications of pneumonia associated with mechanical ventilation, including extrapulmonary infections, and making it difficult to treat the infection.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):297-305
DOI 10.5935/0103-507X.20130051
To describe a single center experience involving the administration of colistin to treat nosocomial infections caused by multidrug-resistant Gram-negative bacteria and identify factors associated with acute kidney injury and mortality.
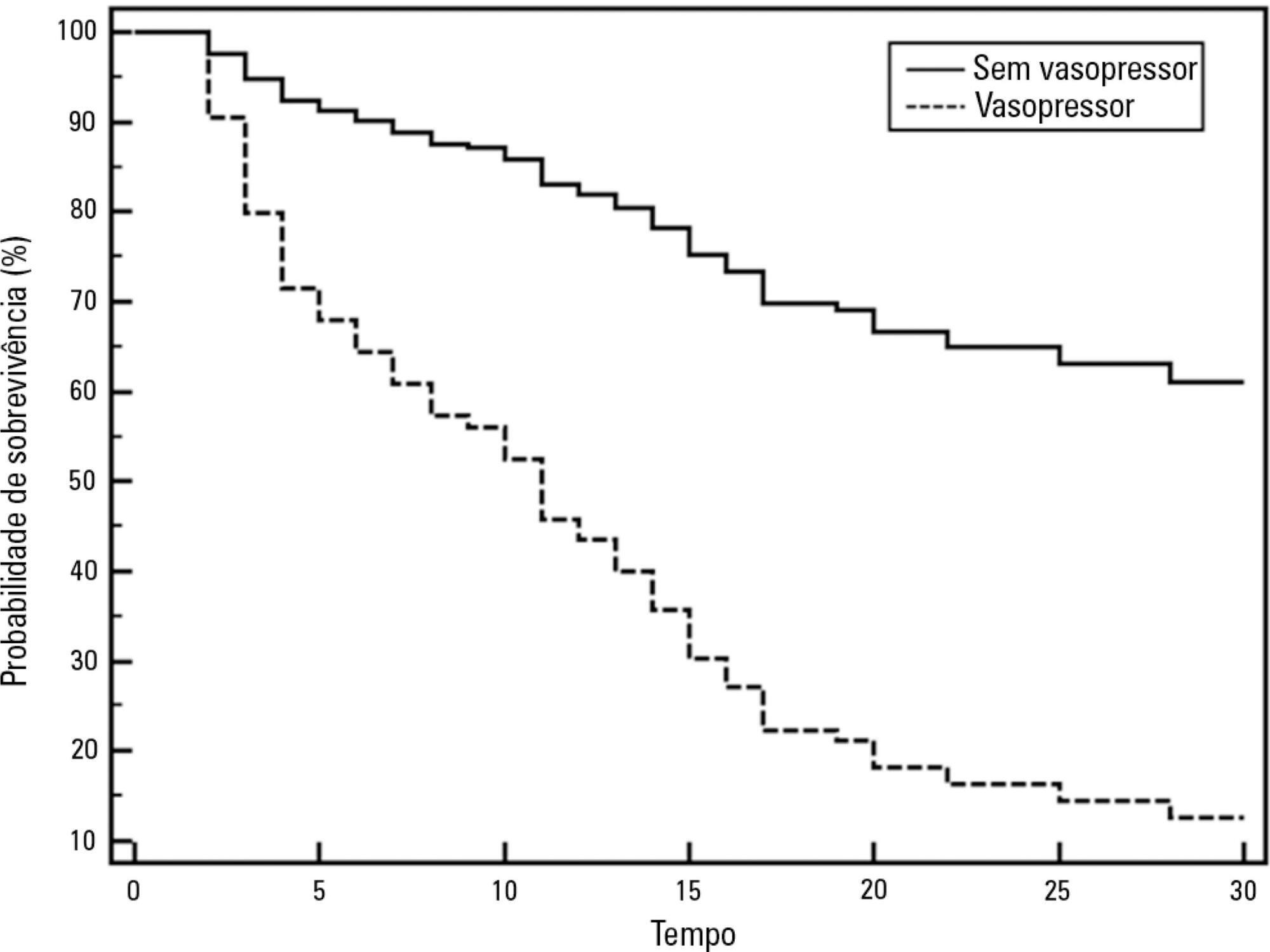
This retrospective longitudinal study evaluates critically ill patients with infections caused by multidrug-resistant Gram-negative bacteria. All adult patients who required treatment with intravenous colistin (colistimethate sodium) from January to December 2008 were considered eligible for the study. Data include demographics, diagnosis, duration of treatment, presence of acute kidney injury and 30-day mortality.
Colistin was used to treat an infection in 109 (13.8%) of the 789 patients admitted to the intensive care unit. The 30-day mortality observed in these patients was 71.6%. Twenty-nine patients (26.6%) presented kidney injury prior to colistin treatment, and six of these patients were able to recover kidney function even during colistin treatment. Twenty-one patients (19.2%) developed acute kidney injury while taking colistin, and 11 of these patients required dialysis. The variable independently associated with the presence of acute kidney injury was the Sequential Organ Failure Assessment at the beginning of colistin treatment (OR 1.46; 95%CI 1.20-1.79; p<0.001). The factors age (OR 1.03; 95%CI 1.00-1.05; p=0.02) and vasopressor use (OR 12.48; 95%CI 4.49-34.70; p<0.001) were associated with death in the logistic-regression model.
Organ dysfunction at the beginning of colistin treatment was associated with acute kidney injury. In a small group of patients, we were able to observe an improvement of kidney function during colistin treatment. Age and vasopressor use were associated with death.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):384-390
DOI 10.1590/S0103-507X2009000400008
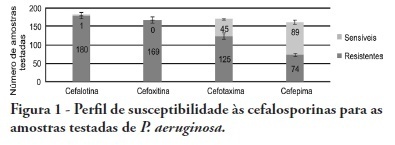
OBJECTIVES: Pseudomonas aeruginosa is an increasingly prevalent opportunistic pathogen in hospital infection cases. Its high resistance rates to many antimicrobials has given this microorganism a relevant role among other highly prevalent bacteria involved in nosocomial infections. This study aimed to analyze epidemiologic characteristics of P. aeruginosa and to evaluate its susceptibility to antimicrobial agents at Hospital das Clínicas of the Universidade Federal de Pernambuco METHODS: A retrospective study was performed based on the registry book of miscellaneous secretions from the bacteriology laboratory of the Hospital das Clínicas involving the period between January and June 2008. Among the secretions registered, were identified the positives samples for P. aeruginosa, whose origin was analyzed, as well as its susceptibility profile to routinely used in our laboratory antimicrobials. RESULTS: The bacteria most frequently isolated from miscellaneous secretions bacteria were P. aeruginosa (26%) and S. aureus (25%). P. aeruginosa was mainly isolated from respiratory infections, with 33% of positive samples for this organism from tracheal secretions and 21% from nasal. The most effective antimicrobials against P. aeruginosa were: amikacin, imipenem, meropenem and aztreonam. CONCLUSIONS: These results show a high prevalence of P. aeruginosa in the Hospital das Clínicas of the Universidade Federal de Pernambuco. Despite featuring high resistance rates to older antimicrobials, as cephalosporins first and second generations and chloramphenicol, this pathogen showed good susceptibility to agents routinely used in this hospital.
Abstract
Rev Bras Ter Intensiva. 2007;19(4):421-427
DOI 10.1590/S0103-507X2007000400003
BACKGROUND AND OBJECTIVES: The frequency of multiple-antibiotic resistant bacteria has been increasing in recent years. Among the gram-negative bacteria Pseudomonas aeruginosa (P. aeruginosa) shows a great propensity for the development of multidrug resistance mechanisms. The objective of this study was to identify the profile of susceptibility to antibiotics, the frequency of multidrug resistance and the cross-resistance between drugs of P. aeruginosa strains in two tertiary hospitals in Recife, Pernambuco. METHODS: The study was carried out between September 2004 and January 2006. The antimicrobial susceptibility testing was performed in 304 strains of P. aeruginosa by the disc diffusion method in accordance with National Committee for Clinical and Laboratory Standards (NCCLS) guidelines. RESULTS: The most frequent materials were urine (26.7%) and respiratory tract secretion (26.1%) The antibiotics tested and their respective susceptibilities were as follows: piperacillin-tazobactam (66.2%); aztreonam (59.8%); amikacin (59.4%); meropenem (58.2%); imipenem (57.7%); ciprofloxacin (49.7%); gentamicin and cefepime (48.6%); ceftazidime (30%) and cefotaxime (6.8%). A high prevalence of multi-resistance was detected. Half (49.7%) the strains showed resistance to three or more antibiotics and 28% were resistant to six antimicrobials or more. Also, cross-resistance between the beta-lactams (carbapenems and piperacilin/tazobactam) and aminoglicosides and quinolones was between 22.9% and 38.1%. These drugs are commonly combined in the treatment of severe infections caused by Pseudomonas, which reflects the difficulty in choosing the appropriate option for combination therapy. CONCLUSIONS: The frequency of multidrug-resistant strains of P. aeruginosa in this study was similar to other hospitals in Brazil and higher than in other countries. In order to reduce the frequency of these multiresistant clones, epidemiologic surveillance and the rational use of antibiotic protocols need to be urgently implemented.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)