Abstract
Rev Bras Ter Intensiva. 2009;21(4):384-390
DOI 10.1590/S0103-507X2009000400008
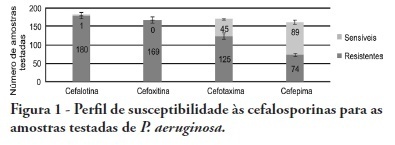
OBJECTIVES: Pseudomonas aeruginosa is an increasingly prevalent opportunistic pathogen in hospital infection cases. Its high resistance rates to many antimicrobials has given this microorganism a relevant role among other highly prevalent bacteria involved in nosocomial infections. This study aimed to analyze epidemiologic characteristics of P. aeruginosa and to evaluate its susceptibility to antimicrobial agents at Hospital das Clínicas of the Universidade Federal de Pernambuco METHODS: A retrospective study was performed based on the registry book of miscellaneous secretions from the bacteriology laboratory of the Hospital das Clínicas involving the period between January and June 2008. Among the secretions registered, were identified the positives samples for P. aeruginosa, whose origin was analyzed, as well as its susceptibility profile to routinely used in our laboratory antimicrobials. RESULTS: The bacteria most frequently isolated from miscellaneous secretions bacteria were P. aeruginosa (26%) and S. aureus (25%). P. aeruginosa was mainly isolated from respiratory infections, with 33% of positive samples for this organism from tracheal secretions and 21% from nasal. The most effective antimicrobials against P. aeruginosa were: amikacin, imipenem, meropenem and aztreonam. CONCLUSIONS: These results show a high prevalence of P. aeruginosa in the Hospital das Clínicas of the Universidade Federal de Pernambuco. Despite featuring high resistance rates to older antimicrobials, as cephalosporins first and second generations and chloramphenicol, this pathogen showed good susceptibility to agents routinely used in this hospital.