You searched for:"Rachel Duarte Moritz"
We found (12) results for your search.-
Original Articles – Clinical Research
Routine chest radiography in intensive care: impact on decision-making
Rev Bras Ter Intensiva. 2012;24(3):252-257
Abstract
Original Articles – Clinical ResearchRoutine chest radiography in intensive care: impact on decision-making
Rev Bras Ter Intensiva. 2012;24(3):252-257
DOI 10.1590/S0103-507X2012000300008
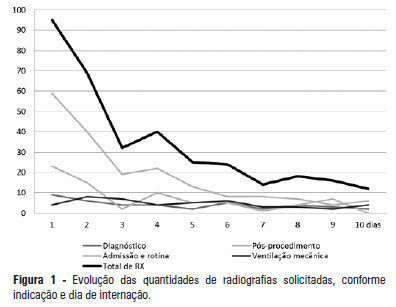
Views0See moreOBJECTIVE: This study determined the prevalence of clinical abnormalities in chest radiographs and its relationship with decision-making in intensive care. METHODS: This prospective cohort study involved nonconsecutive patients who were admitted to the intensive care unit at the Hospital Universitário Professor Polydoro Ernani de São Thiago of the Universidade Federal de Santa Catarina. Imaging tests in the intensive care unit (ICU) were assessed daily between February and May 2011 and divided according to the reason for hospitalization, the type of test requested, anatomical segment under assessment and the purpose of the request. The imaging tests were interpreted by intensivists and subsequently divided according to the detected abnormalities and changes in medical care. The chi-squared test was used for statistical analysis. RESULTS: The study sample included 106 patients. A total of 447 imaging tests were assessed, 425 of which were anteroposterior chest radiographs. An average of 4.01 radiographs per patient was obtained. Among the requested radiographs, 79.3% were normal, and 35.2% of abnormal radiographs did not prompt changes in medical care. CONCLUSION: Most of the radiographs performed in the intensive care unit exhibited no statistically significant clinical alterations, and the radiographs that revealed abnormalities did not necessarily lead to changes in medical care.
-
II Forum of the “End of Life Study Group of the Southern Cone of America”: palliative care definitions, recommendations and integrated actions for intensive care and pediatric intensive care units
Rev Bras Ter Intensiva. 2011;23(1):24-29
Abstract
II Forum of the “End of Life Study Group of the Southern Cone of America”: palliative care definitions, recommendations and integrated actions for intensive care and pediatric intensive care units
Rev Bras Ter Intensiva. 2011;23(1):24-29
DOI 10.1590/S0103-507X2011000100005
Views0See morePalliative care is aimed to improve the quality of life of both patients and their family members during the course of life-threatening diseases through the prevention, early identification and treatment of the symptoms of physical, psychological, spiritual and social suffering. Palliative care should be provided to every critically ill patient; this requirement renders the training of intensive care practitioners and education initiatives fundamental. Continuing the Technical Council on End of Life and Palliative Care of the Brazilian Association of Intensive Medicine activities and considering previously established concepts, the II Forum of the End of Life Study Group of the Southern Cone of America was conducted in October 2010. The forum aimed to develop palliative care recommendations for critically ill patients.
-
Original Articles
Perceptions about end of life treatment in Argentina, Brazil and Uruguay intensive care units
Rev Bras Ter Intensiva. 2010;22(2):125-132
Abstract
Original ArticlesPerceptions about end of life treatment in Argentina, Brazil and Uruguay intensive care units
Rev Bras Ter Intensiva. 2010;22(2):125-132
DOI 10.1590/S0103-507X2010000200005
Views0ABSTRACT OBJECTIVE: To evaluate end-of-life procedures in intensive care units. METHODS: A questionnaire was prepared by the End-of-Life Study Group of the Argentinean, Brazilian and Uruguayan Intensive Care societies, collecting data on the participants’ demographics, institutions and limit therapeutic effort (LTE) decision making process. During this cross sectional study, the societies’ multidisciplinary teams members completed the questionnaire either during scientific meetings or online. The variables were analyzed with the Chi-square test, with a p<0.05 significance level. RESULTS: 420 professionals completed the questionnaire. The Brazilian units had more beds, unrestricted visit was less frequent, their professionals were younger and worked more recently in intensive care units, and more non-medical professionals completed the questionnaire. Three visits daily was the more usual number of visits for the three countries. The most influencing LTE factors were prognosis, co-morbidities, and therapeutic futility. In the three countries, more than 90% of the completers had already made LTE decisions. Cardiopulmonary resuscitation, vasoactive drugs administration, dialysis and parenteral nutrition were the most suspended/refused therapies in the three countries. Suspension of mechanic ventilation was more frequent in Argentina, followed by Uruguay. Sedation and analgesia were the less suspended therapies in the three countries. Legal definement and ethical issues were mentioned as the main barriers for the LTE decision making process. CONCLUSION: LTE decisions are frequent among the professionals working in the three countries’ intensive care units. We found a more proactive LTE decision making trend In Argentina, and more equity for decisions distribution in Uruguay. This difference appears to be related to the participants’ different ages, experiences, professional types and genders.
Keywords:Medical FutilityQuestionnairesTerminal careTerminally illTreatment refusalWithholding TreatmentSee more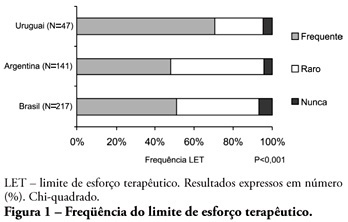
-
Editorial
Fairness, not maleficence, in terminal critical patients care
Rev Bras Ter Intensiva. 2009;21(4):341-342
Abstract
EditorialFairness, not maleficence, in terminal critical patients care
Rev Bras Ter Intensiva. 2009;21(4):341-342
-
1st Forum of the Southern Cone End-of-Life Study Group: proposal for care of patients, bearers of terminal disease staying in the ICU
Rev Bras Ter Intensiva. 2009;21(3):306-309
Abstract
1st Forum of the Southern Cone End-of-Life Study Group: proposal for care of patients, bearers of terminal disease staying in the ICU
Rev Bras Ter Intensiva. 2009;21(3):306-309
DOI 10.1590/S0103-507X2009000300011
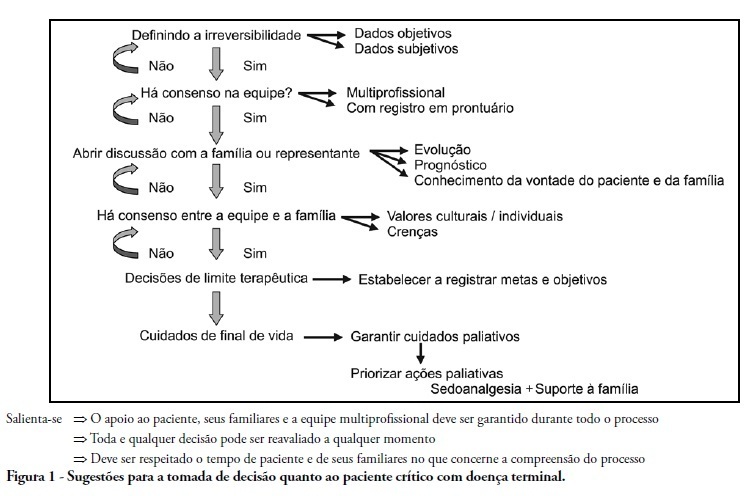
Views5See moreWithholding of treatment in patients with terminal disease is increasingly common in intensive care units, throughout the world. Notwithstanding, Brazilian intensivists still have a great difficulty to offer the best treatment to patients that have not benefited from curative care. The objective of this comment is to suggest an algorithm for the care of terminally ill patients. It was formulated based upon literature and the experience of experts, by members of the ethics committee and end-of-life of AMIB – Brazilian Association of Intensive Care.
-
Original Articles
Evaluation of medical decisions at the end-of-life process
Rev Bras Ter Intensiva. 2009;21(2):141-147
Abstract
Original ArticlesEvaluation of medical decisions at the end-of-life process
Rev Bras Ter Intensiva. 2009;21(2):141-147
DOI 10.1590/S0103-507X2009000200005
Views0See moreOBJECTIVES: To evaluate the medical decisions at end-of-life of patients admitted at HU/UFSC and to compare these decisions and the profile of patients who died in the intensive care unit (ICU) to those who died in medical (MW) and surgical wards (SW). METHODS: This is a retrospective and observational study. Demographic data, clinical features, treatment and the end-of-life care decisions of adult patients who died in wards and the intensive care unit of HU/UFSC from July/2004 to December/2008 were analyzed . For statistical analysis the Student’s t, χ2 and ANOVA tests were used: (significance p <0.05). RESULTS: An analysis was made of 1124 deaths: 404 occurred in ICU, 607 in MW and 113 in SW. The overall hospital mortality rate was 5.9% (ICU=24.49%, MW=7.2%, SW=1.69%). Mean ages of patients were: ICU=56.7, MW=69.3 and SW=70.4 years (p <0.01). Withholding/withdrawing life support was performed prior to 30.7% of deaths in the intensive care unit and 10% in the wards (p <0.01). Cardiopulmonary resuscitation was not carried out in 65% of cases in ICU, 79% in MW and 62% in SW. Besides cardiopulmonary resuscitation, the more frequent withholding/withdrawing life support in the intensive care unit were vasoactive drugs and in the wards refusal of admission to intensive care unit . Do-not-resuscitate order was documented in 2.4% of cases in ICU and 2.6% in MW. Palliative and comfort care were provided to 2% of patients in ICU, 11.5% in MW and 8% in SW. Terminality of the disease was recognized in 40% of cases in ICU, 34.6% in MW and 16.8% in SW. CONCLUSIONS: The profile of patients who died and medical decisions during the end-of-life process were different in the intensive care unit, clinical and surgical wards.
-
Review Articles
End of life and palliative care in intensive care unit
Rev Bras Ter Intensiva. 2008;20(4):422-428
Abstract
Review ArticlesEnd of life and palliative care in intensive care unit
Rev Bras Ter Intensiva. 2008;20(4):422-428
DOI 10.1590/S0103-507X2008000400016
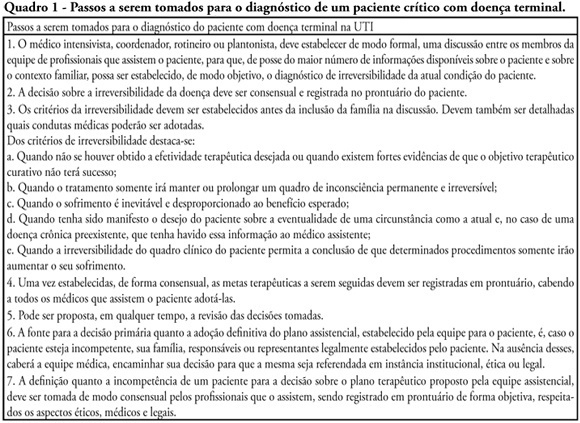
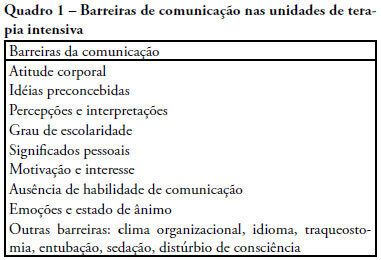
Views0See moreThe objective of this review was to evaluate current knowledge regarding terminal illness and palliative care in the intensive care unit, to identify the major challenges involved and propose a research agenda on these issues The Brazilian Critical Care Association organized a specific forum on terminally ill patients, to which were invited experienced and skilled professionals on critical care. These professionals were divided in three groups: communication in the intensive care unit, the decision making process when faced with a terminally ill patient and palliative actions and care in the intensive care unit. Data and bibliographic references were stored in a restricted website. During a twelve hour meeting and following a modified Delphi methodology, the groups prepared the final document. Consensual definition regarding terminality was reached. Good communication was considered the cornerstone to define the best treatment for a terminally ill patient. Accordingly some communication barriers were described that should be avoided as well as some approaches that should be pursued. Criteria for palliative care and palliative action in the intensive care unit were defined. Acceptance of death as a natural event as well as respect for the patient’s autonomy and the nonmaleficence principles were stressed. A recommendation was made to withdraw the futile treatment that prolongs the dying process and to elected analgesia and measures that alleviate suffering in terminally ill patients. To deliver palliative care to terminally ill patients and their relatives some principles and guides should be followed, respecting individual necessities and beliefs. The intensive care unit staff involved with the treatment of terminally ill patients is subject to stress and tension. Availability of a continuous education program on palliative care is desirable.
-
Evaluate the clonidine use for sedoanalgesia in intensive care unit patients under prolonged mechanical ventilation
Rev Bras Ter Intensiva. 2008;20(1):24-30
Abstract
Evaluate the clonidine use for sedoanalgesia in intensive care unit patients under prolonged mechanical ventilation
Rev Bras Ter Intensiva. 2008;20(1):24-30
DOI 10.1590/S0103-507X2008000100004
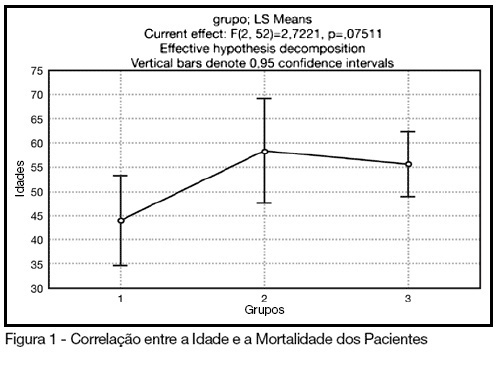
Views0See moreBACKGROUND AND OBJECTIVES: The control of patient discomfort in the intensive care unit (ICU) has become an integral part of critical care practice. The sedoanalgesic drugs could influence critically ill patient’s morbimortality. Alpha²-adrenoceptor agonists might have an interesting future in ICU. The objective of this study is to evaluate the clonidine use for sedoanalgesia in ICU patients under prolonged mechanical ventilation. METHODS: Historical cohort study. Admitted patient files, January-December 2006, which stayed under mechanical ventilation, analgesia and sedation > 7days were analyzed. Demographic, clinical features and therapeutic data concerning analgesia and sedation were remarked. The data allowed classify the patients in three different groups: G1 = patients that used clonidine and other drugs; G2 = patients that used three or more drugs, without clonidine and G3 = patients that used fentanyl and midazolam. The mean daily doses of infused clonidine were registered, and the values of heat rate (HR), blood arterial pressure (BAP) before starting use of clonidine, after six hours and 24 hours were also registered. Statistical analyzes were performed using Variance Analysis (ANOVA), t tests and x² (significance p < 0.05). RESULTS: Were selected 55 patients. Fifteen (27.2%) belonged to G1, 11 (20%) belonged to G2 and 29 (52.7%) belonged to G3. The mean age of patients was 44 (G1), 50 (G2) and 56 (G3) (p = NS). The mean score APACHE II was 18 (G1), 20.4 (G2) and 20.7 (G3) (p = NS). G1 and G2 patients presented higher ICU length-of-stay (p < 0.05). The mean dose of clonidine used was 1.21 ± 0.54 mg/kg/min. G1 patients had HR and BAP decreased, however these effects were not considered clinically relevant. The mortality was lower in the patients from G1 (20%) when compared to G2 (54.5%) and G3 (62%) (p < 0.05). CONCLUSIONS: The clonidine use to analyzed patients did not result in clinical relevant side effects. The lower mortality index in patients that used clonidine was statistical significant.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




