Abstract
Rev Bras Ter Intensiva. 2022;34(2):227-236
DOI 10.5935/0103-507X.20220020-en
To establish current Portuguese critical care practices regarding analgesia, sedation, and delirium based on a comparison between the activities reported and daily clinical practice.
A national survey was conducted among physicians invited to report their practice toward analgesia, sedation, and delirium in intensive care units. A point prevalence study was performed to analyze daily practices.
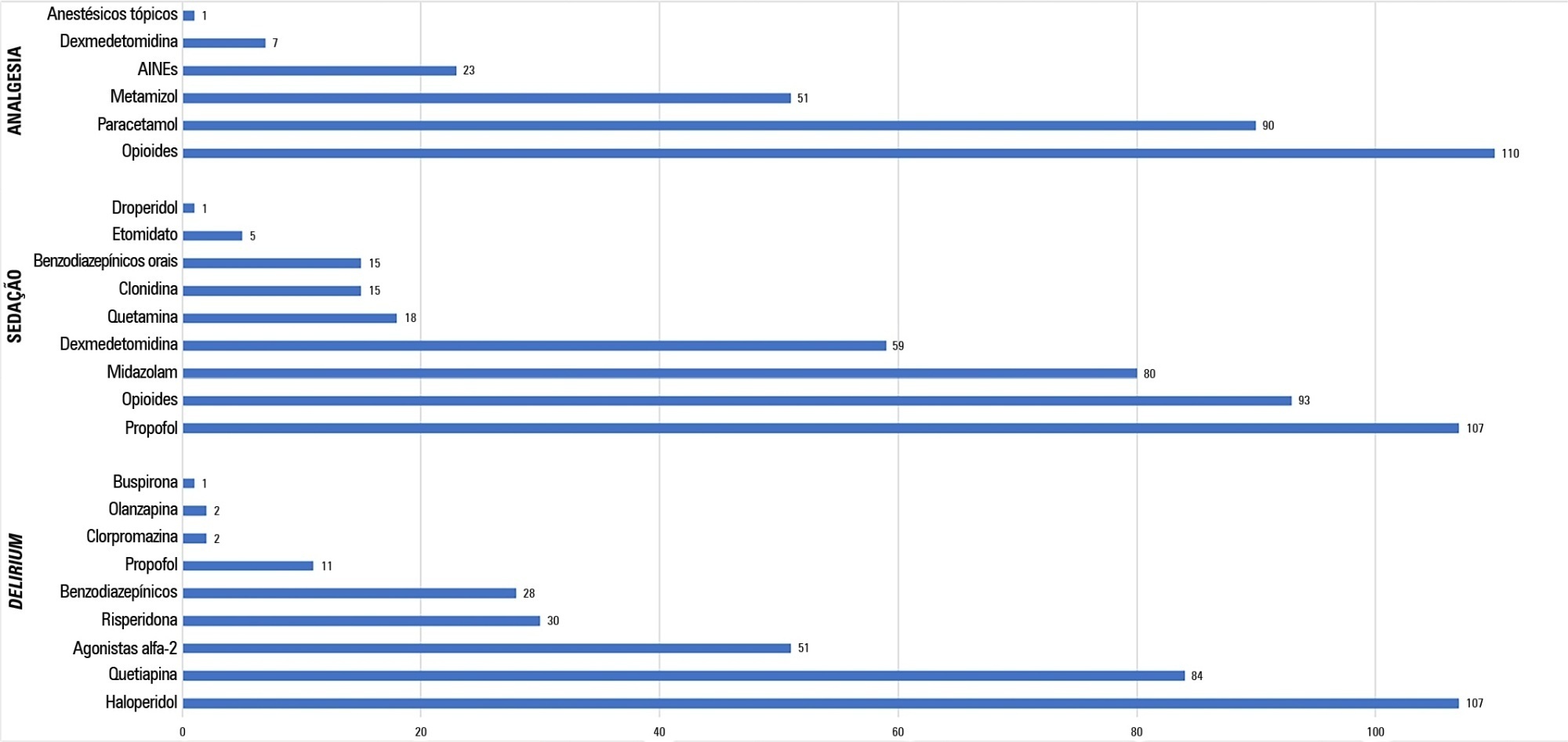
A total of 117 physicians answered the survey, and 192 patients were included in the point prevalence study. Survey and point prevalence studies reflect a high sedation assessment (92%; 88.5%), with the Richmond Agitated Sedation Scale being the most reported and used scale (41.7%; 58.2%) and propofol being the most reported and used medication (91.4%; 58.6%). Midazolam prescribing was reported by 68.4% of responders, but a point prevalence study revealed a use of 27.6%.
The results from the survey did not accurately reflect the common practices in Portuguese intensive care units, as reported in the point prevalence study. Efforts should be made specifically to avoid oversedation and to promote delirium assessment.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):600-615
DOI 10.5935/0103-507X.20210087
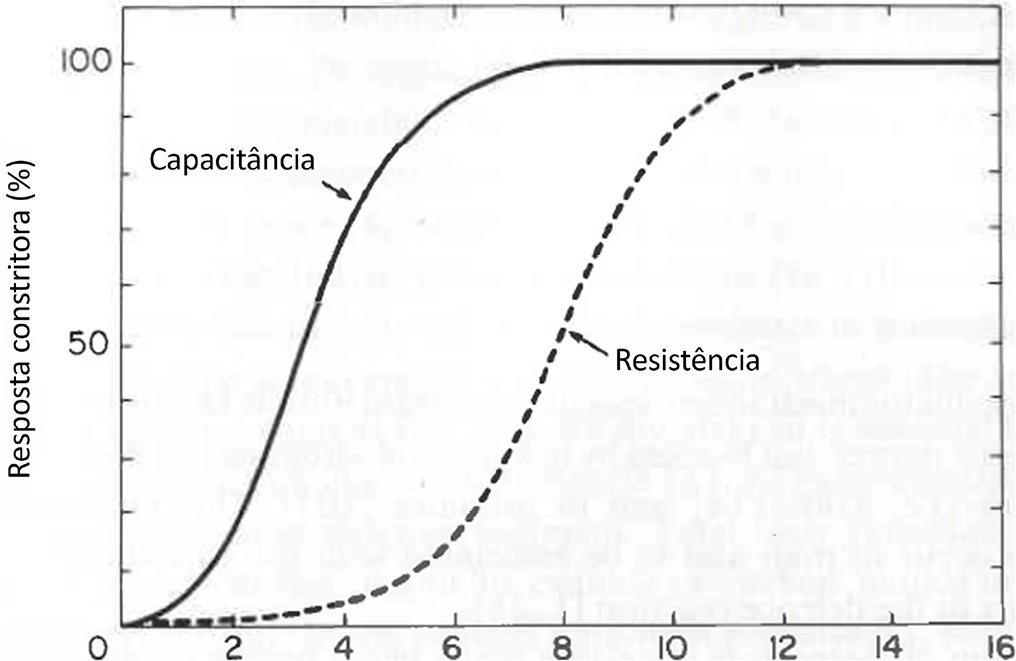
Cardiac, ventilatory and kidney management in the critical care setting has been optimized over the past decades. Cognition and sedation represent one of the last remaning challenges. As conventional sedation is suboptimal and as the sedation evoked by alpha-2 adrenergic agonists (“cooperative” sedation with dexmedetomidine, clonidine or guanfacine) represents a valuable alternative, this manuscript covers three practical topics for which evidence-based medicine is lacking: a) Switching from conventional to cooperative sedation (“switching”): the short answer is the abrupt withdrawal of conventional sedation, immediate implementation of alpha-2 agonist infusion and the use of “rescue sedation” (midazolam bolus[es]) or “breakthrough sedation” (haloperidol bolus[es]) to stabilize cooperative sedation. b) Switching from conventional to cooperative sedation in unstable patients (e.g., refractory delirium tremens, septic shock, acute respiratory distress syndrome, etc.): to avoid hypotension and bradycardia evoked by sympathetic deactivation, the short answer is to maintain the stroke volume through volume loading, vasopressors and inotropes. c) To avoid these switches and associated difficulties, alpha-2 agonists may be considered first-line sedatives. The short answer is to administer alpha-2 agonists slowly from admission or endotracheal intubation up to stabilized cooperative sedation. The “take home” message is as follows: a) alpha-2 agonists are jointly sympathetic deactivators and sedative agents; b) sympathetic deactivation implies maintaining the stroke volume and iterative assessment of volemia. Evidence-based medicine should document our propositions.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):497-503
DOI 10.5935/0103-507X.20190087
To evaluate whether electromyographical findings could predict intensive care unit mortality among mechanically ventilated septic patients under profound sedation.
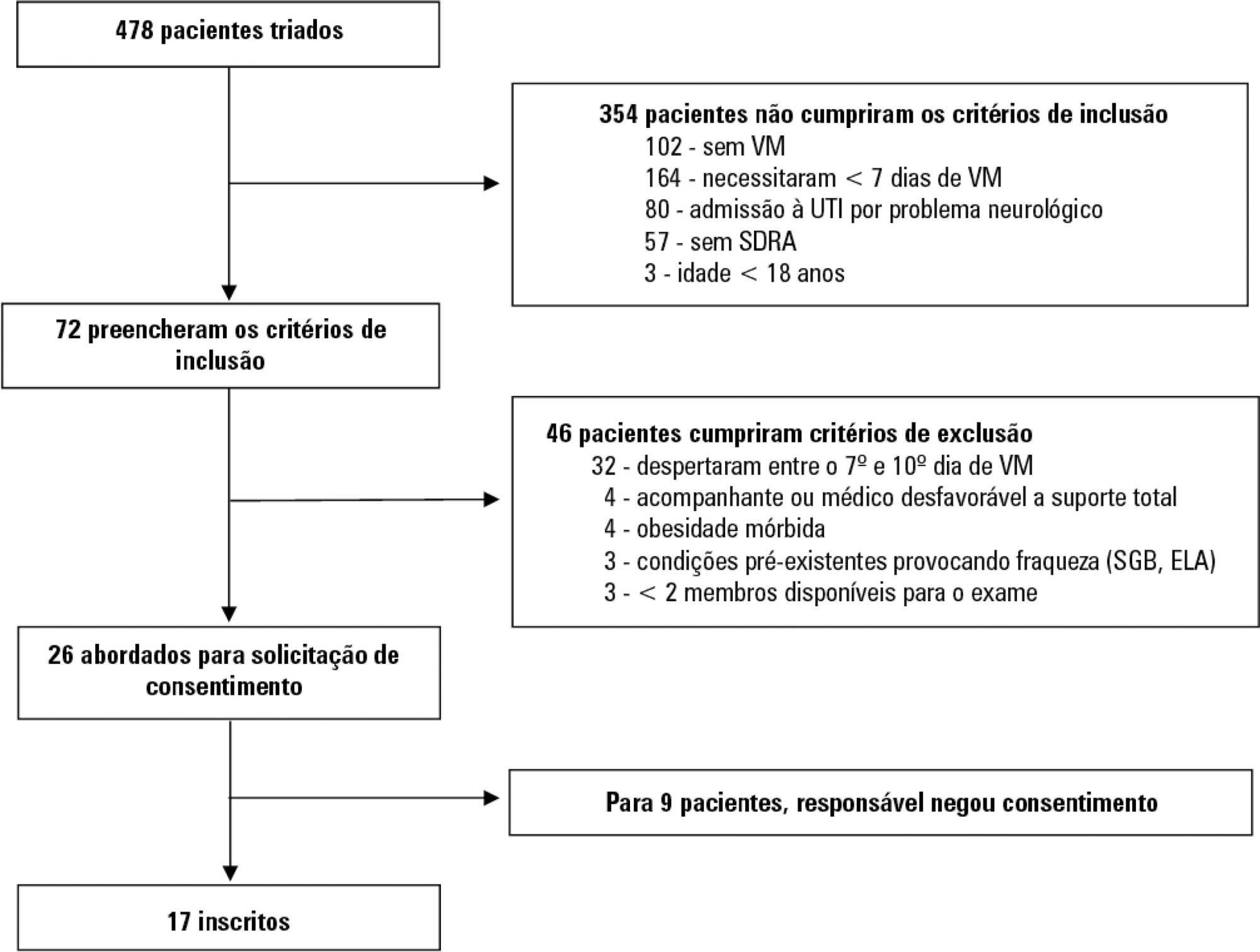
A prospective cohort study that consecutively enrolled moderate-severe acute respiratory distress syndrome (partial pressure of oxygen/fraction of inspired oxygen < 200) patients who were ≥ 18 years of age, dependent on mechanical ventilation for ≥ 7 days, and under profound sedation (Richmond Agitation Sedation Scale ≤ -4) was conducted. Electromyographic studies of the limbs were performed in all patients between the 7th and the 10th day of mechanical ventilation. Sensory nerve action potentials were recorded from the median and sural nerves. The compound muscle action potentials were recorded from the median (abductor pollicis brevis muscle) and common peroneal (extensor digitorum brevis muscle) nerves.
Seventeen patients were enrolled during the seven months of the study. Nine patients (53%) had electromyographic signs of critical illness myopathy or neuropathy. The risk of death during the intensive care unit stay was increased in patients with electromyographical signs of critical illness myopathy or neuropathy in comparison to those without these diagnostics (77.7% versus 12.5%, log-rank p = 0.02).
Electromyographical signs of critical illness myopathy or neuropathy between the 7th and the 10th day of mechanical ventilation may be associated with intensive care unit mortality among moderate-severe acute respiratory distress syndrome patients under profound sedation, in whom clinical strength assessment is not possible.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):155-161
DOI 10.5935/0103-507X.20130027
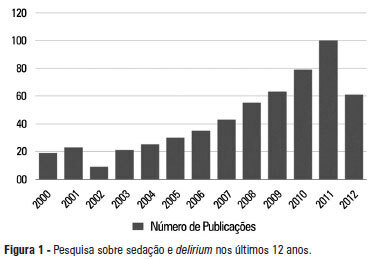
A significant number of landmark studies have been published in the last decade that increase the current knowledge on sedation for critically ill patients. Therefore, many practices that were considered standard of care are now outdated. Oversedation has been shown to be hazardous, and light sedation and no-sedation protocols are associated with better patient outcomes. Delirium is increasingly recognized as a major form of acute brain dysfunction that is associated with higher mortality, longer duration of mechanical ventilation and longer lengths of stay in the intensive care unit and hospital. Despite all the available evidence, translating research into bedside care is a daunting task. International surveys have shown that practices such as sedation interruption and titration are performed only in the minority of cases. Implementing best practices is a major challenge that must also be addressed in the new guidelines. In this review, we summarize the findings of sedation and delirium research over the last years. We also discuss the gap between evidence and clinical practice and highlight ways to implement best practices at the bedside.
Abstract
Rev Bras Ter Intensiva. 2006;18(2):186-189
DOI 10.1590/S0103-507X2006000200012
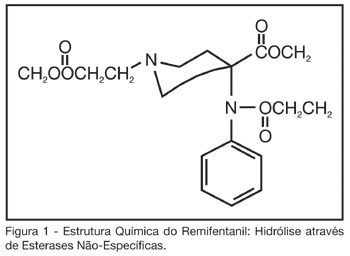
BACKGROUND AND OBJECTIVES: Critically ill patients frequently need to use sedative and analgesic drugs, as part of their treatment or during several procedures. It is a challenge for all intensive care providers to determine the best drug to be used for each patient, with less collateral effects. The objective of this study is to describe the background to give the use of remifentanil in intensive care clinical practice. CONTENTS: Remifentanil is a short acting opioid agonist little used in intensive care medicine. Several studies have been published, showing that remifentanil is a safe drug to be used for the sedation and analgesia for intensive care patients, still needing more information regardless to septic shock patients. CONCLUSIONS: Because remifentanil is a relatively new drug, it is not yet part of the routine drugs used for intensive care providers, although solid evidences of its safety and efficiency for critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2008;20(1):24-30
DOI 10.1590/S0103-507X2008000100004
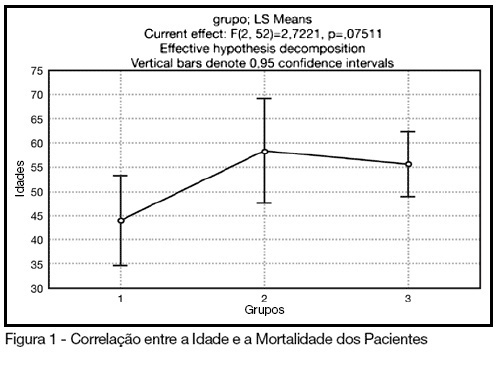
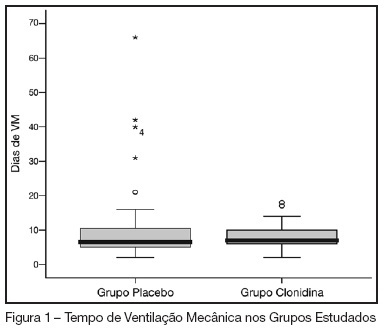
BACKGROUND AND OBJECTIVES: The control of patient discomfort in the intensive care unit (ICU) has become an integral part of critical care practice. The sedoanalgesic drugs could influence critically ill patient's morbimortality. Alpha²-adrenoceptor agonists might have an interesting future in ICU. The objective of this study is to evaluate the clonidine use for sedoanalgesia in ICU patients under prolonged mechanical ventilation. METHODS: Historical cohort study. Admitted patient files, January-December 2006, which stayed under mechanical ventilation, analgesia and sedation > 7days were analyzed. Demographic, clinical features and therapeutic data concerning analgesia and sedation were remarked. The data allowed classify the patients in three different groups: G1 = patients that used clonidine and other drugs; G2 = patients that used three or more drugs, without clonidine and G3 = patients that used fentanyl and midazolam. The mean daily doses of infused clonidine were registered, and the values of heat rate (HR), blood arterial pressure (BAP) before starting use of clonidine, after six hours and 24 hours were also registered. Statistical analyzes were performed using Variance Analysis (ANOVA), t tests and x² (significance p < 0.05). RESULTS: Were selected 55 patients. Fifteen (27.2%) belonged to G1, 11 (20%) belonged to G2 and 29 (52.7%) belonged to G3. The mean age of patients was 44 (G1), 50 (G2) and 56 (G3) (p = NS). The mean score APACHE II was 18 (G1), 20.4 (G2) and 20.7 (G3) (p = NS). G1 and G2 patients presented higher ICU length-of-stay (p < 0.05). The mean dose of clonidine used was 1.21 ± 0.54 mg/kg/min. G1 patients had HR and BAP decreased, however these effects were not considered clinically relevant. The mortality was lower in the patients from G1 (20%) when compared to G2 (54.5%) and G3 (62%) (p < 0.05). CONCLUSIONS: The clonidine use to analyzed patients did not result in clinical relevant side effects. The lower mortality index in patients that used clonidine was statistical significant.
Abstract
Rev Bras Ter Intensiva. 2007;19(3):284-291
DOI 10.1590/S0103-507X2007000300003
BACKGROUND AND OBJECTIVES: In our country, the abstinence syndrome has high prevalence and besides the distress prolongs the length of hospital stay. The aim of this study was to evaluate the influence of associating oral clonidine to the intravenous morphine plus midazolam continuous infusion in children submitted to mechanical ventilation. METHODS: Randomized, double blind, placebo controlled study, conducted in the PICU at the Hospital Geral of Caxias do Sul. All children (1-36 months) submitted to mechanical ventilation over 12 hours (May-2005/August-2006), which had used intravenous morphine and midazolam continuous infusion were included. They were randomized to received clonidine (5 µg/kg) or placebo associated to the sedative continuous infusion. The infusion sedative doses were at the discretion of the assistant physician. The administered doses in the previous 24 hours and the doses of intermittent sedation were daily collected. The abstinence syndrome was defined based on Finnegan Score. The groups were compared regarding the cumulative doses of sedatives, length of use of sedative continuous infusion, presence and duration of the abstinence. RESULTS: Were included 69 patients (31 in the clonidine group and 38 in the placebo group). The two groups were similar regarding the general characteristics (weight, age, gender, indication of mechanical ventilation). The midazolam and morphine doses (cumulative and intermittent doses) were not different in both groups. Completed the study 59 patients, 25 in clonidine group and 34 in placebo group. The prevalence of the abstinence was similar (72% and 75%, respectively), without difference in the recovery time neither related to the length of mechanical ventilation. CONCLUSIONS: In children submitted to mechanical ventilation using high dose of opioids and diazepinic infusion the addiction of clonidine did not decrease the daily doses neither the cumulative doses and nevertheless reduced the prevalence and the evolution of abstinence syndrome.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)