Abstract
Rev Bras Ter Intensiva. 2021;33(4):600-615
DOI 10.5935/0103-507X.20210087
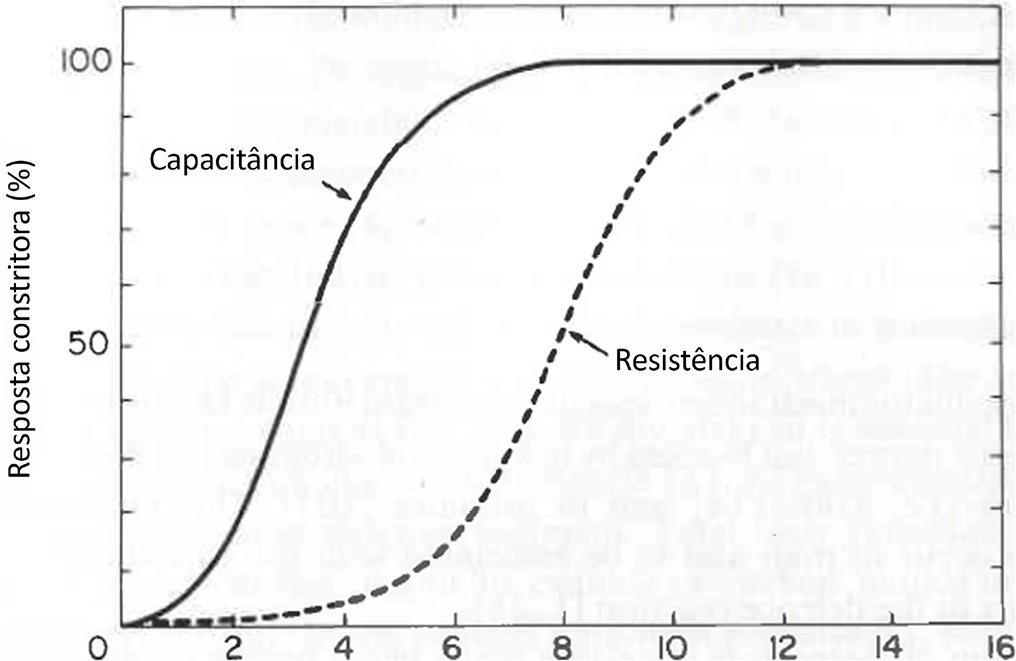
Cardiac, ventilatory and kidney management in the critical care setting has been optimized over the past decades. Cognition and sedation represent one of the last remaning challenges. As conventional sedation is suboptimal and as the sedation evoked by alpha-2 adrenergic agonists (“cooperative” sedation with dexmedetomidine, clonidine or guanfacine) represents a valuable alternative, this manuscript covers three practical topics for which evidence-based medicine is lacking: a) Switching from conventional to cooperative sedation (“switching”): the short answer is the abrupt withdrawal of conventional sedation, immediate implementation of alpha-2 agonist infusion and the use of “rescue sedation” (midazolam bolus[es]) or “breakthrough sedation” (haloperidol bolus[es]) to stabilize cooperative sedation. b) Switching from conventional to cooperative sedation in unstable patients (e.g., refractory delirium tremens, septic shock, acute respiratory distress syndrome, etc.): to avoid hypotension and bradycardia evoked by sympathetic deactivation, the short answer is to maintain the stroke volume through volume loading, vasopressors and inotropes. c) To avoid these switches and associated difficulties, alpha-2 agonists may be considered first-line sedatives. The short answer is to administer alpha-2 agonists slowly from admission or endotracheal intubation up to stabilized cooperative sedation. The “take home” message is as follows: a) alpha-2 agonists are jointly sympathetic deactivators and sedative agents; b) sympathetic deactivation implies maintaining the stroke volume and iterative assessment of volemia. Evidence-based medicine should document our propositions.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):155-161
DOI 10.5935/0103-507X.20130027
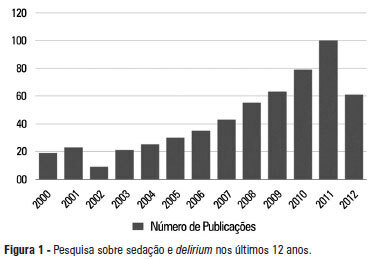
A significant number of landmark studies have been published in the last decade that increase the current knowledge on sedation for critically ill patients. Therefore, many practices that were considered standard of care are now outdated. Oversedation has been shown to be hazardous, and light sedation and no-sedation protocols are associated with better patient outcomes. Delirium is increasingly recognized as a major form of acute brain dysfunction that is associated with higher mortality, longer duration of mechanical ventilation and longer lengths of stay in the intensive care unit and hospital. Despite all the available evidence, translating research into bedside care is a daunting task. International surveys have shown that practices such as sedation interruption and titration are performed only in the minority of cases. Implementing best practices is a major challenge that must also be addressed in the new guidelines. In this review, we summarize the findings of sedation and delirium research over the last years. We also discuss the gap between evidence and clinical practice and highlight ways to implement best practices at the bedside.