Abstract
Rev Bras Ter Intensiva. 2021;33(3):428-433
DOI 10.5935/0103-507X.20210068
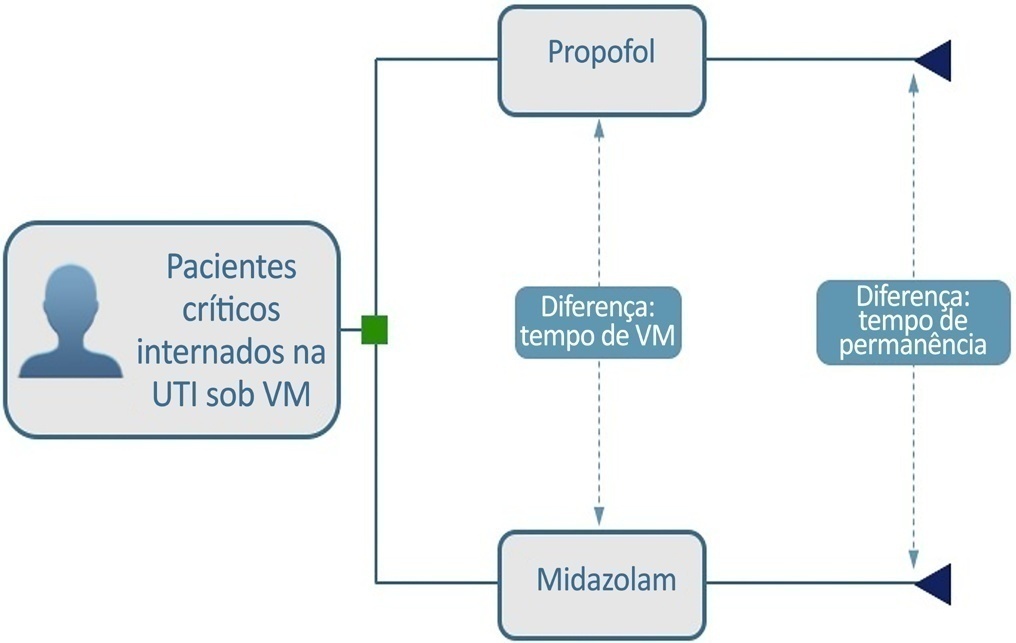
To build a cost-effectiveness model to compare the use of propofol versus midazolam in critically ill adult patients under mechanical ventilation.
We built a decision tree model for critically ill patients submitted to mechanical ventilation and analyzed it from the Brazilian private health care system perspective. The time horizon was that of intensive care unit hospitalization. The outcomes were cost-effectiveness per hour of intensive care unit stay avoided and cost-effectiveness per hour of mechanical ventilation avoided. We retrieved data for the model from a previous meta-analysis. We assumed that the cost of medication was embedded in the intensive care unit cost. We conducted univariate and probabilistic sensitivity analyses.
Mechanically ventilated patients using propofol had their intensive care unit stay and the duration of mechanical ventilation decreased by 47.97 hours and 21.65 hours, respectively. There was an average cost reduction of US$ 2,998.971 for propofol when compared to midazolam. The cost-effectiveness per hour of intensive care unit stay and mechanical ventilation avoided were dominant 94.40% and 80.8% of the time, respectively.
There was a significant reduction in costs associated with propofol use related to intensive care unit stay and duration of mechanical ventilation for critically ill adult patients.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):155-161
DOI 10.5935/0103-507X.20130027
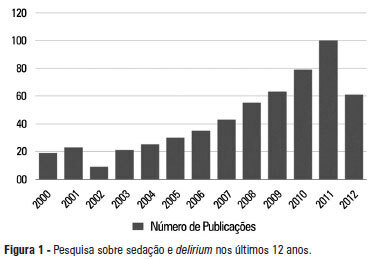
A significant number of landmark studies have been published in the last decade that increase the current knowledge on sedation for critically ill patients. Therefore, many practices that were considered standard of care are now outdated. Oversedation has been shown to be hazardous, and light sedation and no-sedation protocols are associated with better patient outcomes. Delirium is increasingly recognized as a major form of acute brain dysfunction that is associated with higher mortality, longer duration of mechanical ventilation and longer lengths of stay in the intensive care unit and hospital. Despite all the available evidence, translating research into bedside care is a daunting task. International surveys have shown that practices such as sedation interruption and titration are performed only in the minority of cases. Implementing best practices is a major challenge that must also be addressed in the new guidelines. In this review, we summarize the findings of sedation and delirium research over the last years. We also discuss the gap between evidence and clinical practice and highlight ways to implement best practices at the bedside.